Clinical Analysis of Acupuncture Combined with Tuina in Treating Cervical Vertigo
Second People’s Hospital of Yiwu City, Zhejiang 322002, China
CLINICAL STUDY
Clinical Analysis of Acupuncture Combined with Tuina in Treating Cervical Vertigo
Wang Zheng-xin, Chen Guang-hui, Zhang Jin-yi, Shi Xiao-cheng, Wu Li-chun, Feng Zhi-wei, Wang Kang, Ding Hui-chun
Second People’s Hospital of Yiwu City, Zhejiang 322002, China
Author:Wang Zheng-xin, bachelor, associate chief physician of Chinese medicine.
E-mail: zjywwzx@163.com
Objective: To investigate the clinical efficacy of acupuncture combined with tuina in treating patients with cervical vertigo.
Methods: According to the principle of randomization, 258 cases with cervical vertigo who met the inclusion criteria for the study were randomly divided into an observation group and a control group, with 129 cases in each. The patients in the observation group received acupuncture combined with tuina therapy, while those in the control group were just treated by the same acupuncture therapy as in the observation group. After 10-day continuous treatments, the clinical efficacies of the two groups were analyzed and compared.
Results: The total effective rate of the observation group was 100%, versus 86.0% of the control group, and the difference was significant (P<0.05). After treatment, cervical range of motion (ROM) scores in both groups were statistically significantly different from those before treatment (allP<0.05); in addition, there was a statistically significant difference in inter-group comparison of ROM score (P<0.05).
Conclusion: Compared with simple acupuncture treatment, acupuncture combined with tuina therapy has a better effect in improving the ROM of cervical vertigo patients, with higher clinical efficacy.
Acupuncture Therapy; Tuina; Massage; Vertigo; Spondylosis; Range of Motion, Articular
Clinically, cervical vertigo (CV), also called vertebral artery ischemic syndrome, is one of the most common types of vertigo, and it’s mostly caused by organic lesions of cervico-occipital, neck-shoulder or other parts, or is caused by tissue dysfunctions[1]. The incidence of CV in the middle and elder population is relatively high. In recent years, with the development of social and economic change in China, there is a growing of aged population, as well as changing of people's lifestyles, thus the incidence of the disease increases year by year[2]. Some studies suggested that acupuncture and tuina therapies could be used to treat CV[3-4]. To investigate the clinical efficacy of acupuncture combined with tuina in treating CV, 129 cases were enrolled in this study, and compared with the other 129 patients who were treated only by acupuncture as a control group. And the results are reported as follows.
1 Clinical Materials
1.1 Diagnostic criteria
According to the summary of the third national cervical spondylosis topic discussion meeting[5], CV is a vertebral artery type of cervical spondylosis,and its diagnostic criteria are as follows: there are cervical vertigo, or (and) a history of cataplexy attacks; neck rotation test is positive; mostly complicated with head symptoms, including blurred vision, tinnitus and hearing disorders; the X-ray examination shows segmental instability in cervical spine or luschka joint osteoarthritis; patients with ocular vertigo, cardiogenic vertigo, central vertigo or aural vertigo need to be excluded; magnetic resonance angiography (MRA) or vertebral artery ultrasound showed that second vertebral artery (V-Ⅱ) had local stenosis or architectural distortion; the patients with basilar artery insufficiency caused by the compression of the first segment of vertebral artery (V-I) (The segment which extends to the point where the artery enters the transverse foramen of the sixth cervical vertebra) and the third segment of vertebral artery (V-Ⅲ) (the segment which comes out of cervical spine and extends to the entering point into the brain) need to be excluded.
1.2 Inclusion criteria
Conforming the above diagnostic criteria; age 37-72 years; no gender limitation; who have signed informed consent form.
1.3 Exclusion criteria
Those were suffering from severe liver or kidney disease or psychiatric disease; those with cervical spine fracture; those with cervical spinal disc herniation; those who did not cooperate with the researchers.
1.4 Statistical analysis
The SPSS 19.0 version statistical software package was used for data processing and statistics. The enumeration data were expressed as percentage form, with between-group comparison by Chi-square test. And the measurement data were expressed as mean ± standard deviationwith betweengroup comparison by independent samplet-test, andP<0.05 indicates a statistical significance.
1.5 General data
Between December 2011 and November 2013, a total of 258 cases with CV who met the inclusion criteria were enrolled and randomized into an observation group and a control group, with 129 cases in each. There were no statistically significant difference in gender, average age, and the average duration between two groups (P>0.05), indicating that the two groups were comparable (Table 1).

Table 1. Inter-group comparison of general data
2 Therapeutic Methods
2.1 Observation group
2.1.1 Acupuncture
Main acupoints: Baihui (GV 20), Taiyang (EX-HN 5), Fengchi (GB 20), Touwei (ST 8) and cervical Jiaji (EX-B 2) points.
Adjunct acupoints: Add Xingjian (LR 2) and Qiuxu (GB 40) for syndrome of upward disturbance of wind yang; Sanyinjiao (SP 6) and Zusanli (ST 36) for syndrome of qi-blood deficiency; Taixi (KI 3) and Fuliu (KI 7) for syndrome of liver-kidney yin deficiency.
Operation: Ask the patient to take a supine position. After routine disinfection, disposable needles of 0.35 mm in diameter and 40 mm in length were used for acupuncture treatment. Insert the needle subcutaneously into Baihui (GV 20) for 1 cun, and conduct even reinforcing-reducing manipulation after arrival of qi. Insert the needle subcutaneously into Taiyang (EX-HN5) for 1 cun. When puncturing Fengchi (GB 20), the needle tip should direct to ipsilateral mouth angle for 1 cun. The rest acupoints were acupunctured by regular method. The needles were retained for 15-20 min each time. The patients were treated once a day.
2.1.2 Tuina
After acupuncture treatment was finished, tuina was manipulated.
First, ask the patient to take a prone position, then Tui-push, Na-grasp, Rou-knead, Dian-tip and Tanbo-pluck the soft tissues of neck as well as the muscles and ligaments to relax.
Second, ask the patient to take a supine position, and correct the malposed small joints in neck by obliquely Ban-pulling the cervical vertebrae.
Third, manipulate traction for cervical spine for 3-5 min by cervical spine stretching method in a supine position, in order to pull the cervical intervertebral space and relieve the situation of vertebral artery compression.
Finally, digital An-press Baihui (GV 20), Taiyang (EX-HN 5), Fengchi (GB 20) and Touwei (ST 8) for 1-2 min for each acupoint.
Tuina was manipulated twice a day, 10 times constitute a course, and the therapeutic efficacy was observed after 2 courses (10 d).
2.2 Control group
Patients in the control group were treated by the same acupuncture treatment as those in the observation group.
3 Therapeutic Efficacy Observation
3.1 Observation index
Cervical spine range of motion (ROM) was scored.
1 point: Moving freely.
2 points: Limitation of motion.
3 points: Stiffness of motion.
4 points: Hard to move.
The higher score indicates more severe illness condition.
3.2 Therapeutic efficacy criteria
Therapeutic efficacy criteria of this study refer red to some related literatures[6-7].
Recovery: After treatment, the clinical symptoms (including headache, dizziness, etc.) were completely eliminated, neck can move normally and the patient can be engaged in the daily work and life, without recurrence within six months.
Marked effect: After treatment, the clinical symptoms were relieved obviously, neck can move normally; however, there may be occasional neck discomfort during daily work and life.
Improvement: After treatment, clinical symptoms and neck function showed improvements.
Failure: After treatment, there was no significant relief in clinical symptoms and signs, which even became worse.
3.3 Results
3.3.1 Comparisons of ROM scores before and after treatment between the two groups
Before treatment, there was no statistical difference in ROM score between the two groups (P>0.05). After treatment, the ROM scores in both groups were statistically significantly different from those before treatment (all P<0.05), there were also significant differences in ROM scores between the two groups (P<0.05), indicating a better effect of symptom relief in the observation group than that in the control group (Table 2).
Table 2. Between-group comparison of ROM score (point)
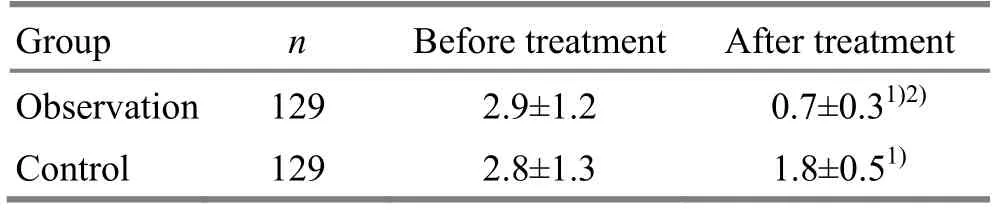
Table 2. Between-group comparison of ROM score (point)
Note: Compared with the same group before treatment, 1) P<0.05; compared with the control group after treatment, 2) P<0.05
?
3.3.2 Comparison of clinical therapeutic efficacy
After continuous treatment of 10 d, the recovery rate in the observation group was 55.8%, and the total effective rate was 100%, versus 30.2% and 86.0% in the control group, showing statistical differences (all P<0.05), and suggesting a higher therapeutic efficacy in the observation group (Table 3).

Table3. Between-group comparison of clinical therapeutic efficacy (case)
4 Discussion
In traditional Chinese medicine, CV belongs to the category of ‘vertigo’, and the major pathogenesis is deficiency in root cause and excess in symptoms. Causes for CV can be summarized as internal and external ones[7]. Internal causes include weakened bodily resistance, congenital deficiency, as well as liver and kidney deficiency; external causes include exogenous pathogen of wind and cold and acute or chronic injuries. Currently, it is generally agreed in clinic that the main cause of CV should be mechanical imbalance of cervical spine due to small cervical joints subluxation, cervical osteoarthritis, cervical disc herniation and cervical curve abnormalities. Cervical mechanical imbalances can compress the sympathetic plexus around the vertebral artery and block blood circulation, so that there are a series of induced symptoms such as hypoxia, malnutrition, dizziness, nausea, and vomiting. Therefore, in traditional Chinese medicine, the treatment principle for CV is mainly to strengthen vital qi to eliminate pathogenic factor, and to correct the cervical mechanical imbalance[8].
Both acupuncture and tuina are common treatment methods for CV[9-12]. Baihui (GV 20) locatesin vertex and can restore consciousness and resuscitate the patient as well as lift spleen-qi and yang; Taiyang (EX-HN 5) can mainly treat patients with headache, migraine headache, toothache and other diseases; Fengchi (GB 20) can cure dizziness and kill pain, and dredge meridians; Touwei (ST 8) is the crossing point of the Stomach Meridian and the Gall Bladder Meridian, it can treat dizziness, ophthalmalgia and epiphora induced by wind; cervical Jiaji (EX-B 2) points can promote flow of qi and blood and strengthen muscles and bones. Needling Baihui (GV 20), Taiyang (EX-HN 5), Fengchi (GB 20), Touwei (ST 8) and cervical Jiaji (EX-B 2) points, combining adjunct acupoints on the basis of syndrome differentiation including Zusanli (ST 36), Sanyinjiao (SP 6), Xingjian (LR 2) or Qiuxu (GB 40) can dredge meridians and activate collaterals, inhibit hyperactive liver yang, as well as lower adverse qi and cure vertigo. Combining with tuina therapy can promote blood circulation, correct cervical small joint subluxation, restore cervical mechanical equilibrium[13], which can be described as addressing both the symptoms and root causes.
In the study, results showed that acupuncture combined with tuina treatment for CV was more significantly effective than simple acupuncture treatment; it is worth further application in clinical practice.
Conflict of Interest
The authors declared that there was no conflict of interest in this article.
Acknowledgments
This work was supported by 2012 Scientific Research Project of Yiwu (the Second Batch, No. 120316).
Statement of Informed Consent
All of the patients in the study signed the informed consent.
[1] Meng ZJ. Tuina therapy of Dian-tipping and Rou-kneading for cervical vertigo. Zhongyi Waizhi Zazhi, 2012, 2(1): 23.
[2] Liu QL. Clinical study on acupuncturing Sishencong acupoint for cervical vertigo. Wuhan: Master Thesis of Hubei University of Traditional Chinese Medicine, 2013.
[3] Chen LQ. Clinical analysis of acupuncture combined withYang Xue Qing Naogranules for cervical vertigo. Zhongguo Yiyao Kexue, 2012, 2(1): 117-118.
[4] Feng WX, Wang WG, Yuan HG. Tuina and tendon-regulation combined with musculoskeletal manipulations for 60 cases with cervical vertigo. Henan Zhongyi, 2013, 33(11): 2003-2004.
[5] Lei PZ. Clinical analysis of tuina for cervical vertigo. Neimenggu Zhongyiyao, 2013, 32(35): 45-46.
[6] Li ZC, Chen DY, Wu DS, Zhao J, Wang XW, Lu XH, Guo YF, Yu B, Liu ZH, Zhao DL. Meeting summary of the third national cervical spondylosis topic discussion meeting. Zhonghua Waike Zazhi, 2008, 46(23): 1797-1798.
[7] Jing RH. Therapeutic efficacy observation of acupuncture combined with tuina for cervical headache. Zhongguo Yiyao Zhinan, 2013, 11(33): 490-491.
[8] Chen B, Cai LH. Clinical efficacy observation of acupuncture combined with tuina for cervical vertigo. Neimenggu Zhongyiyao, 2011, 30(12): 73-74.
[9] Weng JS. Observation on efficacy comparison of treating cervical headache with massage combined with acupuncture and simple acupuncture treatment. Zhongyi Linchuang Yanjiu, 2013, 5(4): 35-36.
[10] Luo RH, Luo RH, Xu K. Therapeutic observation on electroacupuncture for cervical vertigo. Shanghai Zhenjiu Zazhi, 2012, 31(5): 311-312.
[11] Liu GX, Chen X, Yang Y. Observation on clinical efficacy of acupuncture therapy for posterior circulation ischemia vertigo. J Acupunct Tuina Sci, 2012, 10(3): 165-168.
[12] Lu JZ, Li YP. Clinical observations on electroacupuncture plus sitting-position pulling and stretching reduction manipulation for the treatment of cervical vertigo. Shanghai Zhenjiu Zazhi, 2013, 32(6): 495-496.
[13] Hu F, Mao ZF. Clinical observation of acupuncture combined with tuina for cervical vertigo. Zhenjiu Linchuang Zazhi, 2009, 25(7): 28-29.
Translator:Deng Ying
R246.2
: A
Date:June 10, 2014
 Journal of Acupuncture and Tuina Science2014年5期
Journal of Acupuncture and Tuina Science2014年5期
- Journal of Acupuncture and Tuina Science的其它文章
- Therapeutic Observation on Tuina plus Electroacupuncture for Lateral Humeral Epicondylitis
- Effect of Electroacupuncture Combined with Tuina on Lumbar Muscle Tone in Patients with Acute Lumbar Sprain
- Comparative Study on the Analgesic Effects of Different Moxibustion Methods with Tai-yi Moxa Stick in Treating Primary Dysmenorrhea
- Warm Needling Combined with Iontophoresis of Chinese Medicine for Temporomandibular Joint Disorder
- Chinese Herbal Foot Bath plus Acupoint Massage Beneficial to the Improvement of Grade 0 Diabetic Foot
- Observation on Clinical Effects of Acupotomy plus Cupping for Knee Osteoarthritis
