Congestive Heart Failure Clinics: How to Make Them Work in a Community-Based Hospital System
Joshua Larned, MD, Mohamad Kabach, MD, Leonardo Tamariz, MD, MPH and Kristine Raimondo, MSN, ARNP-BC
1Jim Moran Heart and Vascular Research Institute, Holy Cross Hospital, Fort Lauderdale, FL, USA;University of Miami Miller School of Medicine, FL, USA
2Miller School of Medicine at the University of Miami, Veterans Affairs Medical Center, Miami, FL, USA
Introduction
Congestive heart failure (CHF) is a complex medical syndrome that affects more than fi ve million people in the United States alone [1]. More than 500,000 new diagnoses are made each year in the United States. This number is projected to increase because of an aging population and better care of the comorbid conditions that cause CHF [2]. Despite advances in medical therapy, half of all people who develop CHF will die within 5 years of their initial diagnosis [1]. CHF accounts for more than $32 billion in health care costs per year and is at the epicenter of health care reform [2]. Although this staggeringly high fi gure includes hospitalizations,outpatient medical encounters, medications, and devices, it does not fully account for less measurable effects such as missed days of work, missed family days of work, and other community/biopsychosocial impacts. Despite standardized CHF therapy and management guidelines [3], CHF remains a major cause of hospitalizations [4]. The overall rate of CHF hospitalizations did not change signifi cantly from 2000 to 2010 although the risk of hospitalization increases according to increasing age [4]. As there are far more community hospitals than tertiary hospitals, CHF hospitalizations have disproportional consequences in community health systems; yet community health systems remain underequipped to address the complex needs of CHF patients. The paradox remains that CHF disease management programs still cluster in tertiary hospital systems. Ironically, CHF educational pathways, including fellowship programs and board certif i cation pathways, focus on advanced therapies such as transplant and device therapy rather than disease management, prevention, and new target therapies. There are numerous factors that complicate CHF care, including delayed diagnosis, inadequate treatment, inadequate education,and ineffective transitions of care. It should come as no surprise that 24% of all CHF patients are likely to be readmitted to a hospital within 30 days [5]. A sobering fact is that health systems have struggled to reduce readmission rates and readmission penalties irrespective of a patient’s socioeconomic status [6].CHF disease management programs have emerged as a potential solution to the CHF epidemic [7].There are some data that demonstrate that specialized heart failure clinics result in better management of patient behavior and medication adherence, with fewer hospitalizations [7–10]. Meta-analyses of CHF disease management programs, however, have demonstrated variable impact on CHF populations[11]. This heterogeneity may be explained by a lack of a standardized multidisciplinary process and variable levels of provider training and care delivery [12,13]. It is known and has been reported that missed diagnosis of and missed opportunities to treat CHF are associated with higher mortality and morbidity[14, 15]. The transition from inpatient to outpatient care can be an especially vulnerable period because of the progressive nature of the disease state, complex medical regimens, the large number of comorbid conditions, and the multiple clinicians who may be involved [16–20]. The impact of CHF specialists and specialty teams in community health systems is less well understood. Currently there are not enough CHF-trained providers to address this unmet health need.
Methods
Our institution set out to examine the impact of a CHF disease management program at Holy Cross Hospital, Fort Lauderdale, Florida. Holy Cross Hospital is a 570-bed nontransplant/nonimplant community hospital in metropolitan Fort Lauderdale. Our program infrastructure uses a trained advanced registered nurse practitioner (ARNP) to identify all CHF hospitalized patients and standardize adherence to national guidelines. Additionally, the ARNP facilitates provider follow-up visits after hospital discharge and encourages 1-week follow-up in an ARNP-maintained CHF clinic on our hospital campus. Patients who are referred to the CHF clinic are seen within 1 week to 10 days of discharge by the ARNP team and on a weekly/as-needed basis until congestion-free stability is achieved. At appropriate intervals, evidence-based treatment is recommended or initiated and titrated according to protocols. Quality-of-life scores are obtained at the index visit and 6-min-walk testing is performed on able patients. The Seattle Heart Failure Risk Assessment is used, when appropriate,to communicate risk with referring providers and drive therapy changes. When mild decompensation episodes occur, patients may receive intravenous diuretics and may be monitored in the clinic.Patients receive additional services such as dietary education or follow-up phone calls (if needed).Family members or support persons are encouraged to accompany patients to the clinic. Patients are seen for up to 1 year, when possible, and discharged from the clinic after 1 year if they maintain continued stability. A CHF fellowship-trained and board-certif i ed specialist provides program oversight. Patents who exhibit progressive features are referred to the CHF specialist for further management. If appropriate, high-risk patients undergo cardiopulmonary exercise testing and right-sided heart catheterization, and are referred to tertiary systems for potential stage D therapies such as transplant or left ventricular assist device (LVAD) therapy. If appropriate, patients are referred for palliative care by the CHF clinic. As a means of tracking our outcomes, we created a CHF clinic disease management registry where individual data were entered on a recurring-visit basis. We used this registry to conduct our analysis. Our hypothesis was that management in our CHF clinic would result in a primary end point of fewer hospitalizations compared with all patients discharged with CHF at our community-based institution. We also used our registry to review mortality and appropriate use of evidence-based medicines with systolic CHF.
A total of 384 patients were seen in the CHF clinic and entered into the CHF registry between 2012 and 2015. A detailed medical record review of patients with a diagnosis of heart failure based on International Classification of Diseases, Ninth Revision(ICD-9) coding during the 3-year timeframe was done. Data regarding age, sex, type of heart failure,New York Heart Association (NYHA) class, ejection fraction, serum creatinine and brain natriuretic peptide values, and readmission and mortality rates within 30 days, 3 months, 6 months, and 1 year were collected. Fifty-nine patients were lost to follow-up and were not included in our analysis. The registry data were analyzed with Pearson’s chi-square test and Fischer’s exact test, and independent samplesttests were used to compare the baseline characteristics. All analyses were performed with SPSS for Windows version 16.0.
Results
The baseline characteristics of CHF clinic enrollees are given in Table 1. Most of our patients had NHYA class II heart failure symptoms (72%); 28% had NYHA class III-IV heart failure symptoms. Patients were likelier to receive standard medical therapy if they were enrolled in the CHF clinic. Our usage rate of beta-blocker and angiotensin-convertingenzyme inhibitor/angiotensin-receptor blocker therapy in patients with systolic heart failure is illustrated in Table 2. Readmission and mortality rates for patients enrolled in the CHF clinic is shown in Table 3. As shown in Table 4, the effect of evidence-based medications at maximum target dosages on readmission and mortality rates was not statistically significant. However, we were able to demonstrate a statistically significant difference in readmission rates between patients who were followed up in the CHF clinic versus those who were not seen in the CHF clinic (Figure 1).

Table 1 Baseline Characteristics of Congestive Heart Failure Clinic Enrollees.

Table 2 Medication Use in Systolic Congestive Heart Failure.

Table 3 Readmission and Mortality Rates for Patients Enrolled in the Congestive Heart Failure Clinic.
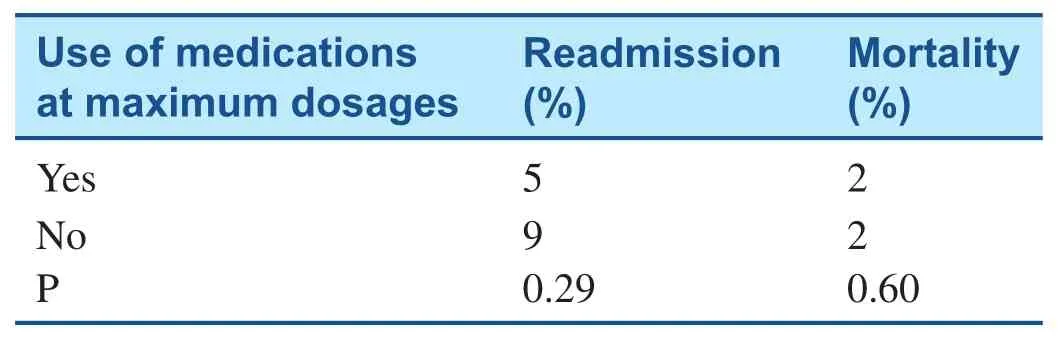
Table 4 Effect of Evidence-Based Medications at Maximum Target Dosages on Readmission and Mortality Rates.
Discussion
Our CHF clinic has been able to demonstrate a consistent favorable impact on readmission rates versus readmission rates for CHF patients who were not referred to a community-based CHF clinic, as illustrated in Figure 1. Over the 1-year course of longitudinal follow-up in the CHF clinic, the readmission risk increased in all groups, thereby ref l ecting the risk of CHF progression. Recurrent CHF hospitalizations indicate a higher risk prognosis across multiple CHF clinical trials, which supports why our center tries to maintain longitudinal care for 1 year, when possible [21, 22].
One explanation for our favorable readmission data may lie in our follow-up protocols. Our followup regimen is rigorous, encouraging patients to be followed up in the CHF clinic on a weekly basis,until they are deemed clinically stable, then on a 1–3-month recurring basis for 1 year after hospitalization. Urgent visits are encouraged, and mild to moderate CHF decompensations are treated with intravenous diuretics, as needed, in the clinic.Patients are encouraged to call the CHF clinic if there is a change in their clinical status, and recommendations may be made to patients accordingly via the telephone. Nutritional services and social support services are provided to all patients enrolled in the CHF clinic. If indicated, home health and cardiac rehabilitation is provided to appropriate patients. Monthly educational group sessions are held for enrolled patients though our Heart Failure University to promote CHF self-management. This medical home approach seems to provide an infrastructure that allows more mechanisms to intervene on CHF patients and across the spectrum of their illness. Our follow-up protocol may be a more costeffective alternative in the context of the cost of a CHF admission along with readmission penalties.
As described above, our experience demonstrates that most of our CHF clinic patients had NHYA class II symptoms. This may be attributable to careful management and follow-up of our patient population. Even when medical therapy could not be achieved to target doses, patients still had fewer hospital events and fewer CHF symptoms. Despite their mean ejection fraction and baseline N-terminal brain natriuretic peptide levels, only 28% of our population had severe CHF symptoms as def i ned by NHYA class III or greater.

Figure 1 Readmission Rates of Congestive Heart Failure (HF) Clinic Patients versus Nonclinic Patients (2012–2015).
Across the NYHA classes we report 15% mortality at 1 year for CHF clinic enrollees. This statistic was not signifi cantly related to achieving target therapy, according to our data. Yet, our mortality rates at 1 year were lower than rates reported by other investigators [23–25].
With regard to a comparison group, we do not have complete mortality data on those CHF patients who were discharged from our hospital but were not followed up in the CHF clinic.
We were able to achieve a high usage rate of betablocker and angiotensin-converting enzyme inhibitor/angiotensin-receptor blocker therapy in patients with systolic heart failure. Accordingly, we report a lower usage rate of aldosterone antagonist therapy in systolic heart failure patients. Our aldosterone antagonist use may ref l ect the fact that, although aldosterone antagonists are integrated into the current guidelines for use in systolic heart failure of NYHA class II or greater, they tend to be used less in patients with NYHA class II CHF [26, 27]. This may also ref l ect the challenges of aldosterone antagonists and their side effects in an elderly population.
In our experience, our specialty team consisting of a CHF-trained ARNP and CHF-trained cardiologist may have impacted our CHF clinic outcomes.CHF community hospital programs represent opportunities to identify patients who may be “CHF rapid progressors.” Early identif i cation of the highest-risk CHF patients facilitates early evaluation and referrals for stage D therapies such as LVAD therapy,transplant, inotropes, palliative care, or hospice care.
Study Limitations
Our sample size is small and likely ref l ects our referral patterns within our hospital system. Our experience demonstrates the challenges in treating CHF within a nontransplant/nonimplant community hospital setting. Our hospital system is not unique in that it is an “open” system where both hospitalemployed and non–hospital employed physicians may treat CHF patients when they are admitted to the hospital. Hospitalized heart failure patients are likelier to be referred to the CHF clinic if they are admitted to the hospitalist service or a hospital medical group service versus a nonemployed provider.Therefore, the bulk of our analysis is limited to those patients who were ultimately referred to the CHF clinic. Secondly, during our CHF clinic’s early existence, our impact was lessened by the fact that we were conf i ned initially to making recommendations rather than directly changing therapy. We were able to shift from an advisory role to a more active role within the first year, but it stands to reason that this initial limitation may have affected our outcomes.
Our data do not account for decompensation episodes within the CHF clinic population. In fact,decompensation episodes did occur in our clinic population but in many circumstances could be managed in an outpatient setting by either administration of intravenous diuretics in the clinic or through increase of oral diuretic therapy followed by rapid follow-up in the clinic.
Conclusion and Take-Home Message
We conclude that CHF community hospital clinics that use a rapid and frequent follow-up format with an ARNP with CHF specialist oversight effectively reduce rehospitalization rates at 1 year. We demonstrate that CHF-trained teams are likelier to place emphasis on evidence-based therapy and achieve greater symptom relief. Having a CHF-trained team in a community hospital setting may create an extra edge that allows earlier recognition of high-risk CHF and facilitate appropriate referrals for LVAD therapy, transplant, or palliative care. This construct presents potential opportunities to reduce medical costs at it pertains to the CHF epidemic. Future directions in CHF management should focus on improving and standardizing the delivery of heart failure care in a community setting.
Conflict of Interest
The authors declare no conf l ict of interest.
Funding
This research received no specific grant from any funding agency in the public, commercial or notfor-profit sectors.
1. Go AS, Mozaffarian D, Roger VL,Benjamin EJ, Berry JD, Borden WB, et al. Heart disease and stroke statistics – 2013 update: a report from the American Heart Association. Circulation 2013;127:e6–245.
2. Roger VL. Epidemiology of heart failure. Circ Res 2013;113:646–59.
3. Yancy CW, Jessup M, Bozkurt B, Butler J, Drazner MH, Fonarow GC, et al. 2013 ACCF/AHA guideline for the management of heart failure: executive summary:a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol 2013;62:1495–539.
4. Hall MJ, DeFrances CJ, Williams SN, Golosinskiy A, Schwartzman A. National Hospital Discharge Survey: 2007. Natl Health Stat Report 2010;26:1–20, 24.
5. Krumholz HM, Merrill AR, Schone EM, Schreiner GC, Chen J, Bradley EH, et al. Patterns of hospital performance in acute myocardial infarction and heart failure 30-day mortality and readmission. Circ Cardiovascular Quality Outcomes 2009;2:407–13.
6. Mahmood SS, Wang TJ. The epidemiology of congestive heart failure:the Framingham Heart Study perspective. Glob Heart 2013;8:77–82.
7. Akosah KO, Schaper AM, Havlik P, Barnhart S, Devine S. Improving care for patients with chronic heart failure in the community: the importance of a disease management program. Chest 2002;122:906–12.
8. Fonarow GC, Stevenson LW,Walden JA, Livingston NA, Steimle AE, Hamilton MA, et al. Impact of a comprehensive heart failure management program on hospital readmission and functional status of patients with advanced heart failure.J Am Coll Cardiol 1997;30:725–32.
9. Ramahi TM, Longo MD, Rohlfs K, Sheynberg N. Effect of heart failure program on cardiovascular drug utilization and dosage in patients with chronic heart failure.Clin Cardiol 2000;23:909–14.
10. Whellan DJ, Gaulden L, Gattis WA, Granger B, Russell SD,Blazing MA, et al. The benef i t of implementing a heart failure disease management program. Arch Intern Med 2001;161:2223–8.
11. Viswanathan M, Kahwati LC, Golin CE, Blalock SJ, Coker-Schwimmer E, Posey R. Medication therapy management interventions in outpatient settings: a systematic review and meta-analysis. JAMA Intern Med 2015;175:76–87.
12. Driscoll A, Worrall-Carter L, Hare DL, Davidson PM, Riegel B,Tonkin A, et al. Evidence-based chronic heart failure management programs: reality or myth? Qual Saf Health Care 2009;18:450–5.
13. Driscoll A, Worrall-Carter L,McLennan S, Dawson A, O‘Reilly J, Stewart S. Heterogeneity of heart failure management programs in Australia. Eur J Cardiovasc Nurs 2006;5:75–82.
14. Akosah KO, Moncher K, Schaper A,Havlik P, Devine S. Chronic heart failure in the community: missed diagnosis and missed opportunities. J Card Fail 2001;7:232–8.
15. Fonarow GC, ADHERE Scientif i c Advisor Committee. The acute decompensated heart failure national registry (ADHERE):opportunities to improve care of patients hospitalized with acute decompensated heart failure. Rev Cardiovasc Med 2003;7:21–30.
16. Amarasingham R, Moore B,Tabak Y, Drazner MH, Clark CA,Zhang S, et al. An automated model to identify heart failure patients at risk for 30-day readmission or death using electronic medical record data. Med Care 2010;48:981–8.
17. Bindman AB, Grumbach K,Osmond D, Komaromy M, Vranizan K, Lurie N, et al. Preventable hospitalizations and access to health care.J Am Med Assoc 1995;274:305–11.
18. Billings J, Anderson GM, Newman LS. Recent fi ndings on preventable hospitalizations. Health Aff (Millwood) 1996;15:239–49.
19. Blustein J, Hanson K, Shea S.Preventable hospitalizations and socioeconomic status. Health Aff(Millwood) 1998;17:177–89.
20. Culler SD, Parchman ML, Przybylski M. Factors related to potentially preventable hospitalizations among the elderly. Med Care 1998;36:804–17.
21. Kommuri NV, Koelling TM,Hummel SL. The impact of prior heart failure hospitalizations on long-term mortality differs by baseline risk of death. Am J Med 2012;125(2):209.e9–e15.
22. Krumholz HM, Lin Z, Keenan PS,Chen J, Ross JS, Drye EE, et al.Relationship between hospital readmission and mortality rates for patients hospitalized with acute myocardial infarction, heart failure,or pneumonia. J Am Med Assoc 2013;309(6):587–93.
23. Curtis LH, Greiner MA, Hammill BG, Kramer JM, Whellan DJ,Schulman KA, et al. Early and long-term outcomes of heart failure in elderly persons, 2001–2005.Arch Intern Med 2008;168:2481–8.
24. Kosiborod M, Lichtman JH,Heidenreich PA, Normand SL,Wang Y, Brass LM, et al. National trends in outcomes among elderly patients with heart failure. Am J Med 2006;119:616.e1–7.
25. The SOLVD Investigators. Effect of enalapril on survival in patients with reduced left ventricular ejection fractions and congestive heart failure. N Engl J Med 1991;325:293–302.
26. The RALES Investigators. Effectiveness of spironolactone added to an angiotensin-converting enzyme inhibitor and a loop diuretic for severe chronic congestive heart failure (the Randomized Aldactone Evaluation Study [RALES]). Am J Cardiol 1996;78:902–7.
27. Boccanelli A, Mureddu GF,Cacciatore G, Clemenza F, Di Lenarda A, Gavazzi A, et al. Antiremodelling effect of canrenone in patients with mild chronic heart failure (AREA IN-CHF study):fi nal results. Eur J Heart Fail 2009;11(1):68–76.
 Cardiovascular Innovations and Applications2015年4期
Cardiovascular Innovations and Applications2015年4期
- Cardiovascular Innovations and Applications的其它文章
- Strategies to Reduce Heart Failure Hospitalizations and Readmissions:How Low Can We Go?
- Cardiac Sarcoidosis: Sorting Fact from Fiction in This Rare Cardiomyopathy
- Unusual Cardiomyopathies: Some May Be More Usual Than Previously Thought and Simply Underdiagnosed
- Epidemiological Study of Heart Failure in China
- Noninvasive Hemodynamic Monitoring for Heart Failure: A New Era of Heart Failure Management
- The Evaluation of the Heart Failure Patient by Echocardiography: Time to go beyond the Ejection Fraction
