Acute Care/Trauma Surgeon's role in obstetrical/ gynecologic emergencies (The OBCAT Alert)
Seong K. Lee, Eddy H. Carrillo, Andrew Rosenthal, Rafael Sanchez, Chauniqua Kiffi n, Dafney L. Davare Division of Acute Care Surgery and Trauma, Memorial Regional Hospital, Hollywood, FL 33021, USA Corresponding Author: Seong K. Lee, Email: SLee@mhs.net
Acute Care/Trauma Surgeon's role in obstetrical/ gynecologic emergencies (The OBCAT Alert)
Seong K. Lee, Eddy H. Carrillo, Andrew Rosenthal, Rafael Sanchez, Chauniqua Kiffi n, Dafney L. Davare Division of Acute Care Surgery and Trauma, Memorial Regional Hospital, Hollywood, FL 33021, USA Corresponding Author: Seong K. Lee, Email: SLee@mhs.net
BACKGROUND: Overwhelming hemorrhage or other intra-abdominal complications may be associated with obstetrical or gynecologic (OB/GYN) procedures and may require the surgical training of an Acute Care/Trauma Surgeon. The OB Critical Assessment Team (OBCAT Alert) was developed at our institution to facilitate a multidisciplinary response to complex OB/GYN cases. We sought to review and characterize the Acute Care/Trauma Surgeon's role in these cases.
METHODS: We conducted a retrospective review of all emergency consults during an OB/GYN case at our institution from 2008 to 2015. An OBCAT is a hospital based alert system designed to immediately notify OB/GYN, anesthesiology, Acute Care/Trauma, the intensive care unit (ICU), and the blood bank of a potential emergency during an OB/GYN case.
RESULTS: There were 7±3 OBCAT alerts/year. Seventeen patients required Acute Care/ Trauma surgery intervention for hemorrhage. Thirteen patients required damage control packing during their hospitalization. Blood loss averaged 6.8±5.5 L and patients received a total of 21±14 units during deliveries with hemorrhage. There were 17 other surgical interventions not related to hemorrhage; seven of these cases were related to adhesions or intestinal injury. Seven additional cases required evaluation post routine OB/GYN procedure; the most common reason was for severe wound complications. There were three deaths during this study period.
CONCLUSION: Emergency OB/GYN cases are associated with high morbidity and may require damage control or other surgical techniques in cases of overwhelming hemorrhage. Acute Care/ Trauma Surgeons have a key role in the treatment of these complex cases.
Obstetric hemorrhage; Postpartum hemorrhage; Damage control packing; Acute care surgery; OBCAT
World J Emerg Med 2016;7(4):274–277
INTRODUCTION
The incidence of hemorrhage during or following obstetrical/gynecologic (OB/GYN) procedures has had an increased incidence over the past decade.[1,2]Severe morbidity and mortality has been associated with overwhelming hemorrhage due to the various causes of obstetrical hemorrhage and its subsequent coagulopathy.[3]In addition, complicated intraabdominal pathology in some OB/GYN cases may require the expertise and skills of an Acute Care/Trauma Surgeon. In response to the increased complexity of some OB/GYN cases, our institution developed a system to coordinate its resources in order to address the need for a multi-disciplinary approach. The OB Critical Assessment Team (OBCAT Alert) was developed at our institution with the goal to address the increasing frequency of severe hemorrhage during obstetrical cases. We sought to review and characterize the Acute Care/Trauma Surgeon's role in complex OB/GYN cases at our institution.
METHODS
A retrospective review (October 2008 to February 2015) was conducted of all patients at our institution that required either intra-operative or post-operative surgical consultation for hemorrhage or complications. The daily trauma service census was queried for surgical cases or consultations involving OB/GYN patients treated at our institution during a delivery or other primary gynecologic procedure. Data was collected and analyzed for the delivery method, placental abnormalities, procedures performed, use of packing, estimated blood loss, units of blood products, operations performed, hospital course and outcomes. This retrospective review was approved by the Memorial Health System Institutional Review Board.
OBCAT Alert
An OBCAT is a hospital wide alert used as notifi cation that an OB/GYN case with anticipated or on-going hemorrhage has occurred. The responders include OB/ GYN, anesthesia, Acute Care/Trauma Services, blood bank, pharmacy, intensivists, neonatology, radiology and nursing. An institutional Massive Transfusion Protocol (MTP) is usually activated as well. This coordinated system was developed to rapidly address complex OB/ GYN cases with severe hemorrhage. In most cases, the Acute Care/Trauma Surgeon assisted the obstetrician when overwhelming hemorrhage was identifi ed following delivery or during an emergency hysterectomy. The Acute Care/Trauma Surgeon would then assist with packing or post-operative care depending on the clinical presentation.
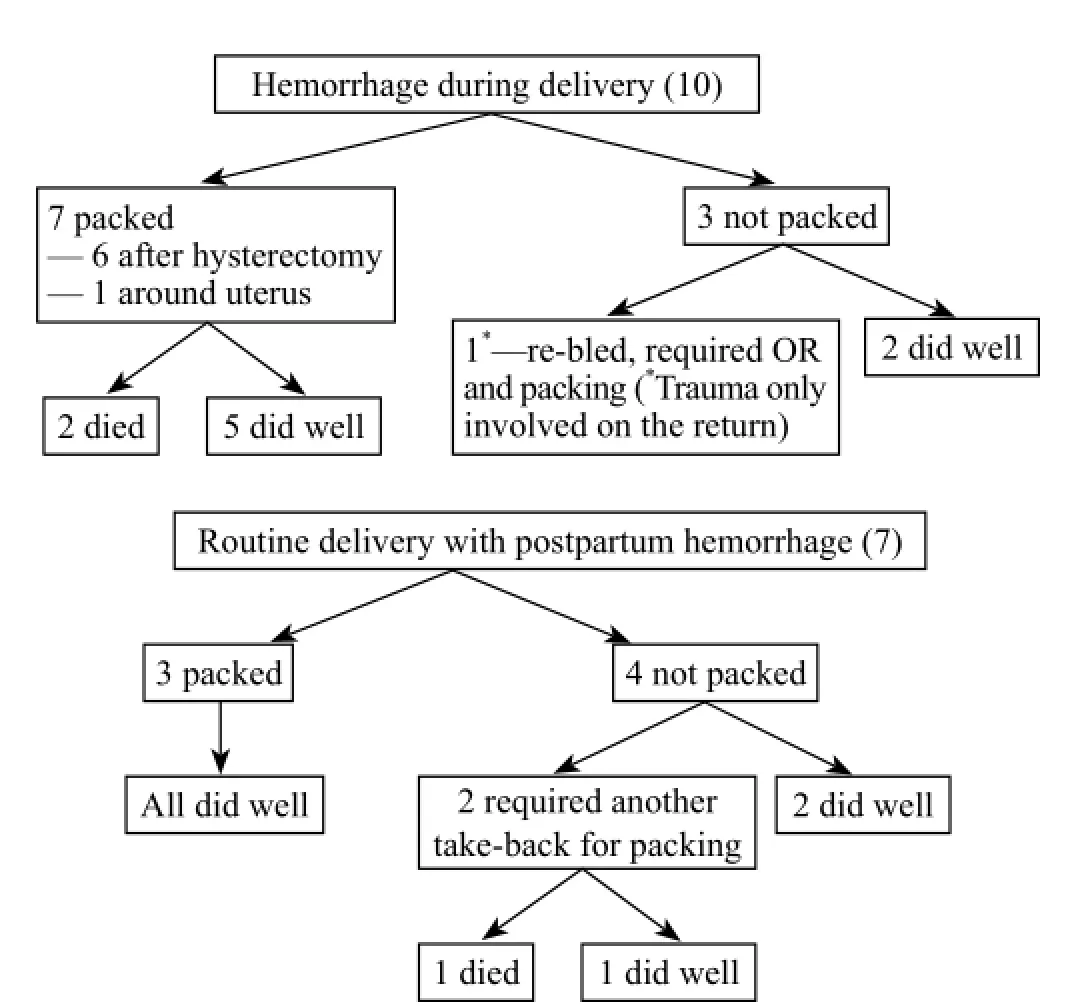
Figure 1. Damage control and timing.
RESULTS
During this period, there were 7±3 OBCAT alerts/ year. Seventeen patients required surgical intervention for hemorrhage (Table 1). Hemorrhage occurred during the primary delivery (10 patients) or at some point (7 patients) in the postpartum time period (Figure 1). Packing was used in a total of 13 patients during their hospital course, but not always during the first surgical intervention (Table 1). Emergency hysterectomy was required in 13 cases of peripartum hemorrhage. Eleven of these peripartum hysterectomies were associated with packing (Table 1).
Blood loss averaged 6.8±5.5 L and patients received a total of 21±14 units during deliveries with hemorrhage. Blood loss averaged 8.5±9.2 L and patients received a total of 18±9.5 units during returns for postpartum hemorrhage.
There were 17 other instances of emergent surgical intervention during a primary OB/GYN case not related to overwhelming hemorrhage. The most common reason for emergent consultation was for small intestinal injury or adhesions (7 patients), followed by exploration (4 patients), appendectomy (3 patients), bladder repair (2patients), colon stricture (1 patient).
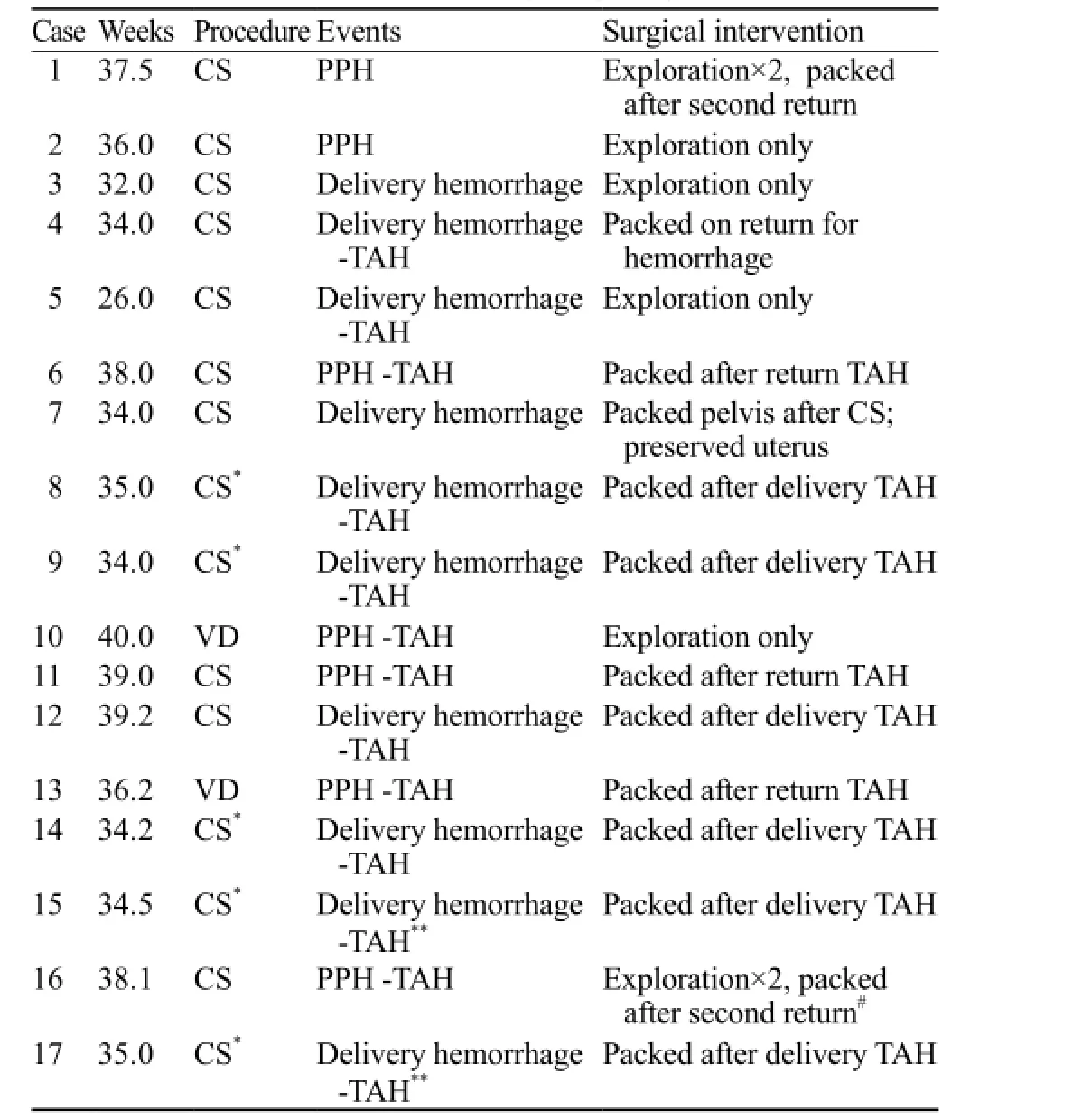
Table 1. OBCAT cases with hemorrhage requiring intervention
There were seven additional cases of OB/GYN patients requiring surgical evaluation post routine OB/ GYN procedure. The most common reason was for severe wound complications which required surgical assessment/management.
There were a total of three deaths during this time in the total population. Hemorrhage cases had a 17.6% mortality. Two deaths were from hemorrhage and intraoperative cardiac arrest after an attempt to pack during an intrapartum hysterectomy. The third patient died after massive hemorrhage and multi-organ failure in the intensive care unit (ICU) (Table 1).
DISCUSSION
Hemorrhage during complex obstetrical cases has been increasing in incidence and is attributed to uterine atony or placental abnormalities associated with increased cesarean rates.[4,5]In addition, physiologic changes in the postpartum state puts patients at risk for continued hemorrhage and coagulopathy, especially following massive transfusion and resuscitation.[6]As more complex and high risk obstetrical cases are identified prenatally, the need for preparation and a multidisciplinary approach has recently been recommended.[7,8]In order to address this need, our institution developed a hospital alert system (OBCAT) with Acute Care/Trauma Services designed to coordinate hospital resources in cases of overwhelming hemorrhage.
To our knowledge, this is one of the largest descriptions of surgical damage control application for hemorrhage associated with obstetrical complications. Previous case reports of damage control techniques included use of packing with and without attempted internal iliac artery ligation or embolization.[5,9,10]Delivery with hemorrhage requiring an emergency hysterectomy was the most common occasion requiring Acute Care/Trauma surgical intervention. In our cases, packing and abbreviated laparotomy was utilized after peripartum hysterectomy or for pelvic packing around a preserved uterus. The decision to perform packing was made at the time of the operation in coordination with the Obstetrician and Acute Care/Trauma Surgeon.
The descriptive nature of our series does not allow conclusions regarding the specific techniques used for hemorrhage control. However, the group of patients who required a return to the OR after a routine delivery and were packed all survived without further complications (Figure 1). This group had standard application of damage control packing and a subsequent return to the OR for closure after a period of resuscitation in the ICU. Unfortunately, despite the combined efforts, there were still three deaths related to overwhelming hemorrhage. Two occurred during delivery with overwhelming hemorrhage and cardiac arrest. The other death occurred after a routine delivery with subsequent postpartum hemorrhage, but was not packed on the first return trip to the OR. This case required a subsequent return to the OR due to continued hemorrhage. Although difficult to determine, the outcome may have been more favorable if you consider the other cases of take-backs with packing.
Following our analysis, several limitations were identifi ed. The focus of this review was on the involvement of Acute Care/Trauma Services; as a result, data was not collected or reported on total births, all peripartum hysterectomies, or use of transfusion in all deliveries during this time period. Consequently, the described mortality in our series is higher than previous reports[4]and reflects only the rate in the few overall cases of uncontrollable hemorrhage which required Acute Care/ Trauma surgical intervention. In addition there was no formal algorithm for determining if a patient required packing beyond the general criteria utilized in trauma patients when they become hypothermic, acidotic, and coagulopathic. Therefore, there may have been some selection bias in this descriptive study by including only the most severe cases of hemorrhage that required Acute Care/Trauma Surgeon involvement.
In summary, Acute Care/Trauma Surgeons have a role in complex OB/GYN cases to help prevent further morbidity in cases of overwhelming hemorrhage and to apply our skill set in other non-hemorrhagic surgical emergencies. Ongoing hemorrhage during an obstetrical case should prompt early Acute Care/Trauma surgical intervention, especially when proceeding with a hysterectomy for overwhelming hemorrhage. The skill sets utilizing general and vascular techniques as well as post-operative critical care experience make the Acute Care/Trauma Surgeon well equipped to manage complex post-hemorrhage OB/GYN patients. In takebacks for hemorrhage, empiric packing and abbreviated laparotomy should be considered. This series should encourage continued development and implementation of protocols to manage overwhelming hemorrhage in complex obstetrical cases in a multi-disciplinary fashion.
ACKNOWLEDGEMENTS
We would like to acknowledge the Obstetrics and GynecologyDepartment at MRH; LeAnn Young, RN and Rachele Solomon, MPH for their assistance with the preparation of the manuscript; and Evelio Velis, MD, PhD for his assistance with the statistical analysis.
Funding: None.
Ethical approval: This retrospective review was approved by the Memorial Health System Institutional Review Board.
Conflicts of interest: The authors declare there is no competing interest related to the study, authors, other individuals or organizations.
Contributors: Lee SK proposed the study and wrote the first draft. All authors read and approved the fi nal version of the paper.
REFERENCES
1 Callaghan WM, Kuklina EV, Berg CJ. Trends in postpartum hemorrhage: United States, 1994–2006. Am J Obstet Gynecol 2010; 202: 353.e1–6.
2 Kramer MS, Berg C, Abenhaim H, Dahhou M, Rouleau J, Mehrabadi A, et al. Incidence, risk factors, and temporal trends in severe postpartum hemorrhage. Am J Obstet Gynecol 2013; 209: 449.e1–7.
3 Callaghan WM, Creanga AA, Kuklina EV. Severe maternal morbidity among delivery and postpartum hospitalizations in the United States. Obstet Gynecol 2012; 120: 1029–1036.
4 Garmi G, Salim R. Epidemiology, etiology, diagnosis, and management of placenta accreta. Obstet Gynecol Int 2012; 2012: 873929.
5 Fawcus S, Moodley J. Postpartum haemorrhage associated with caesarean section and caesarean hysterectomy. Best Pract Res Clin Obstet Gynaecol 2013; 27: 233–249.
6 Pacheco LD, Saade GR, Costantine MM, Clark SL, Hankins G. The role of massive transfusion protocols in obstetrics. Am J Perinatol 2013; 30: 1–4.
7 American College of Obstetricians and Gynecologists Committee on Patient Safety and Quality Improvement. Committee opinion no. 590: preparing for clinical emergencies in obstetrics and gynecology. Obstet Gynecol 2014; 123: 722–725.
8 Weisbrod AB, Sheppard FR, Chernofsky MR, Blankenship CL, Gage F, Wind G, et al. Emergent management of postpartum hemorrhage for the general and acute care surgeon. World J Emerg Surg 2009; 4: 43.
9 Michel P, Jarry J, Guinaudeau F, Nguyen V, Bourilhon N, Imperato M. Damage control to control a severe obstetrical hemorrhage. J Visc Surg 2012; 149: e364–365.
10 Awonga A, Merhi Z, Khulpateea N. Abdominal packing for intractable obstetrical and gynecologic hemorrhage. Int J Gynecol Obstet 2006; 93: 160–163.
Accepted after revision June 9, 2016
10.5847/wjem.j.1920–8642.2016.04.006
Original Article
February 19, 2016
 World journal of emergency medicine2016年4期
World journal of emergency medicine2016年4期
- World journal of emergency medicine的其它文章
- The state and future of emergency medicine in Macedonia
- Amiodaron in atrial fi brillation: post coronary artery bypass graft
- Short lessons in basic life support improve self-assurance in performing cardiopulmonary resuscitation
- Is current training in basic and advanced cardiac life support (BLS & ACLS) effective? A study of BLS & ACLS knowledge amongst healthcare professionals of North-Kerala
- Effects of a general practitioner cooperative co-located with an emergency department on patient throughput
- The Buffering analysis to identify common geographical factors within the vicinity of severe injury related to motor vehicle crash in Malaysia
