紧急剖胸术在严重胸部创伤中的应用价值及手术指征探讨
刘宗志+霍承瑜+牛磊
(民航總医院心胸外科,北京 100123)
[摘 要] 目的:分析紧急剖胸术(Emergency thoracotomy,ET)在严重胸部创伤中的应用价值,探讨其手术指征。方法:分析行ET的120例严重胸部创伤患者资料,将接受急诊室ET的42例患者纳入急诊室组,将接受手术室ET的78例患者纳入手术室组。比较两组患者手术情况及预后,总结ET的临床价值及手术指征。结果:急诊室组ISS评分、术后死亡率高于手术室组,差异有统计学意义(P<0.05);穿透伤患者死亡率组间比较,差异无统计学意义(P>0.05)。急诊室组存活患者术后并发症发生率为39.13%,与手术室组的41.38%比较,差异无统计学意义(P>0.05)。随访期间4例患者(均接受全肺切除)遗留中度肺功能障碍、右心功能不全,11例患者遗留轻度肺功能障碍,2例患者心电图复查可见心肌损害表现,其余64例患者均未见明显异常。结论:急诊室ET对钝性伤所致严重胸部创伤的治疗价值有限;严重胸部创伤患者ET术后死亡原因以严重心包压塞、失血性休克为主,对于符合上述手术指征或合并主要支气管损伤、空气栓塞者,应及时实施ET。
[关键词] 紧急剖胸术;胸部创伤;手术指征
中图分类号:R655 文献标识码:A 文章编号:2095-5200(2017)04-021-03
DOI:10.11876/mimt201704009
Application value and surgical indications of emergency thoracotomy in severe thoracic trauma LIU Zongzhi,HUO Chengyu,NIU Lei. (Department of thoracicsurgery,Civil Aviation General Hospital,Beijing 100123 China)
[Abstract] Objective: This study was designed to analyse the application value of emergency thoracotomy (ET) in severe thoracic trauma, and to explore its indications of operation. Methods: A total sample of 120 patients with severe thoracic trauma were analyzed. 42 patients who received ET of emergency department were included in the emergency room group, and 78 patients who received ET of operating room were included in the operating room group. The surgical conditions and prognosis of the two groups were compared, and the clinical value of ET and surgical indications were summed up. Results: The ISS score and postoperative mortality in the emergency room group were higher than those in the operating room group, the difference was statistically significant (P<0.05); and there was no statistically significant difference in the mortality for penetrating between the two groups (P>0.05). The incidence of postoperative complications was 39.13% in the survivors of the emergency room group and 41.38% in the operating room group, the difference was not statistically significant (P>0.05). During the follow-up period, 4 patients (all undergoing pneumonectomy) had moderate pulmonary dysfunction, right ventricular dysfunction, 11 patients with mild pulmonary dysfunction, 2 patients with myocardial damage showed by ECG, the remaining 64 patients were no obvious exception. Conclusions: The effect of ET in treatment of severe thoracic trauma caused by blunt trauma is limited. The cause of death in patients with severe thoracic trauma after ET is mainly due to severe pericardial tamponade and hemorrhagic shock. For patients who meet the above surgical indications or complicated with severe bronchial injury and air embolism, should be timely implementation of ET.
[Key words] emergency thoracotomy; thoracic trauma; surgical indications
胸部创伤约占创伤的6%~10%,占交通事故伤的44%以上,患者死亡率仅次于颅脑损伤,约有半数创伤患者死亡原因与胸部创伤及其并发症有关[1]。严重胸部创伤以肋骨骨折、胸壁心肺损伤所致气胸、血胸或张力性气胸为主要表现,患者常伴有呼吸和循环功能障碍,病情凶险、死亡率高[2]。作为初期复苏的重要环节,近年来紧急剖胸术(Emergency thoracotomy,ET)在严重胸部创伤的治疗中得到了广泛应用,但目前临床关于ET应用价值及手术指征的探讨缺乏病例对照,无法为临床实践提供充足的依据[3]。本研究对120例患者进行了对照分析。
1 资料与方法
1.1 一般资料
回顾性分析我院2000年5月~2016年5月行ET 120例严重胸部创伤[4]患者资料。患者受伤至入院时间≤72 h,排除合并溺水、爆炸伤、中毒者。按照患者ET实施时机,将接受急诊室ET的42例患者纳入急诊室组,将接受手术室ET的78例患者纳入手术室组。
1.2 手术方案
42例患者于到达医院即刻接受急诊室ET治疗,治疗方案:14例接受心包减压术,18例接受心脏按压术,10例接受胸腔穿刺减压、心包穿刺减压与心脏修补术;78例患者入院时生命体征稳定,行急诊胸部平片或(和)CT检查后,送至手术室实施ET,治疗方案:16例行心脏修补后开窗引流,5例行肺门血管探查修补,5例行全肺切除,5例行主支气管修补,3例行前上纵隔血肿探查及左锁骨下动脉修补,3例行右无名静脉修补,20例行肋间动脉/胸廓内动脉结扎,8例行肺深裂伤修补,13例行肺局部切除。ET术中或术后处理其他合并伤。
1.3 分析指标及方法
对比两组手术情况、存活率及术后并发症发生情况,其中临床资料包括年龄、性别、损伤严重度评分(ISS)[5]、受伤类型等。根据术后随访资料,分析手术时机对患者预后转归的影响。
对本临床研究的所有数据采用SPSS18.0进行分析,以P<0.05为差异有统计学意义。
2 结果
2.1 临床资料
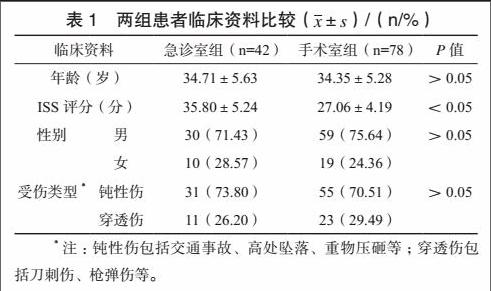
急诊室组ISS评分高于手术室组,差异有统计学意义(P<0.05),两组患者年龄、性别、受伤类型等其他临床资料比较,差异無统计学意义(P>0.05)。见表1。
2.2 手术情况
急诊室组入院至手术时间为(28.16±4.52)min,低于手术室组的(40.45±9.48)min,差异有统计学意义(P<0.05),两组患者术中出血量分别为(2315.81±194.65)mL、(2267.40±201.58)mL,组间比较差异无统计学意义(P>0.05)。
2.3 死亡率与并发症
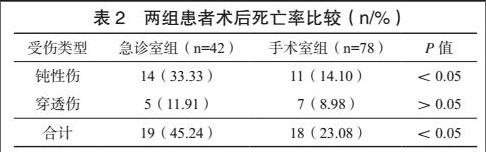
急诊室组患者术后死亡率为45.24%,高于手术室组的23.08%,差异有统计学意义(P<0.05),但穿透伤患者死亡率组间比较,差异无统计学意义(P>0.05)。见表2。急诊室组患者死亡原因:心脏压塞13例,心脏延迟破裂5例,术后多器官功能障碍综合征1例;手术室组患者死亡原因:心脏压塞8例,肺门血管大出血3例,肋间损伤伴不可逆休克2例,主支气管断裂3例,急性右心衰2例。
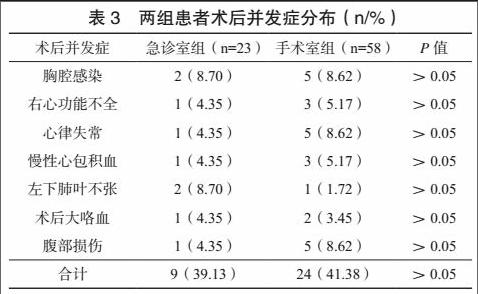
急诊室组存活患者术后并发症发生率为39.13%,与手术室组的41.38%比较,差异无统计学意义(P>0.05)。两组患者术后并发症分布见表3,除右心功能不全患者未得到明显改善外,其余29例发生术后并发症患者均获治愈。
2.4 随访结果
81例存活患者均获得有效随访,平均随访时间(9.25±2.79)个月,其中4例患者(均接受全肺切除)遗留中度肺功能障碍、右心功能不全,11例患者遗留轻度肺功能障碍,2例患者心电图复查可见心肌损害表现,其余64例患者均未见明显异常。
3 讨论
严重胸部创伤是创伤致死的主要原因,在紧急情况下,诊断与复苏往往需同时进行,加之辅助检查时间缺乏,如何根据体征、诊断性胸穿及影像学资料判断ET指征,为争取时间、挽救患者生命的关键[6]。由于手术室条件远优于急诊室条件,但在中转过程中可能造成治疗贻误,故ET实施时机不可一概而论[7-8]。
我们统计显示急诊室组患者入院时ISS评分更高,该类患者病情更为严重,甚至入院时存在心跳、呼吸停止,极度呼吸困难、进行性血压下降等表现,需立即实施复苏救治。由于患者生命体征极不稳定,即便实施完善外科干预,致命性心肺损伤引发的心跳、呼吸停止仍可对患者生存造成明显影响[9-10]。因此,急诊室组患者死亡率高达45.24%。
因急诊室ET难于处理钝性伤所致心脏压塞、心脏延迟破裂,应尽量避免对钝性伤患者实施急诊室手术。总结急诊室ET的手术指征:1)穿透伤所致严重胸部创伤并伴有心跳或呼吸停止;2)出现胸腔内进行性出血,且已发生重度失血性休克[11];3)因心脏压塞或空气栓塞所致严重低血压;4)颈部、上肢根部因穿刺伤所致大出血,需及时实施主动脉钳夹[12-13]。
对于院前指数(PHI)超过4分且血流动力学不稳定者,应考虑ET[14]。Struck等[15]认为,在最初的数分钟内实施手术救治,对于避免神经损伤甚至功能损失也有着重要意义。近年来,院前急救技术的进展,使部分严重胸部创伤患者可获得手术室复苏机会[16]。笔者认为,在急诊ET指征的基础上,对于入院时生命体征仍存在且短暂心肺复苏无效的严重胸部创伤患者[17],均可考虑手术室ET救治。但是,对于颈部穿透伤、上肢根部大出血而言,盲目实施ET可能因交通支的存在导致止血效果受限[18]。因此,ET术前应评估患者创伤状态,若患者存在胸骨旁穿透伤,应注重术中封闭止血,必要时中转腔内支架,保证止血效果。
综上所述,ET在严重胸部创伤中的救治中有着确切的应用价值,急诊室ET对钝性伤所致严重胸部创伤的治疗价值有限。。
参 考 文 献
[1] Wyrick D L, Dassinger M S, Bozeman A P, et al. Hemodynamic variables predict outcome of emergency thoracotomy in the pediatric trauma population[J]. J Pediatr Surg, 2014, 49(9): 1382-1384.
[2] Flaris A N, Simms E R, Prat N, et al. Clamshell incision versus left anterolateral thoracotomy. Which one is faster when performing a resuscitative thoracotomy? The tortoise and the hare revisited[J]. World J Surg, 2015, 39(5): 1306-1311.
[3] 都定元. 重视复苏性剖胸探查术在濒死创伤患者救治中的应用[J]. 中华创伤杂志, 2016, 32(7): 577-581.
[4] Flynn-OBrien K T, Stewart B T, Fallat M E, et al. Mortality after emergency department thoracotomy for pediatric blunt trauma: Analysis of the National Trauma Data Bank 2007–2012[J]. J Pediatr Surg, 2016, 51(1): 163-167.
[5] Seamon M J, Haut E R, Van Arendonk K, et al. An evidence-based approach to patient selection for emergency department thoracotomy: A practice management guideline from the Eastern Association for the Surgery of Trauma[J]. J Trauma Acute Care Surg, 2015, 79(1): 159-173.
[6] 王云, 何勇, 胡杨杨. 胸部创伤250例临床诊治[J]. 中国急救医学, 2014, 34(7): 55-56.
[7] Dayama A, Sugano D, Spielman D, et al. Basic data underlying clinical decision‐making and outcomes in emergency department thoracotomy: tabular review[J]. ANZ J Surg, 2016, 86(1-2): 21-26.
[8] Manz E, Nofz L, Norman A N, et al. Incidence of clotted haemopericardium in traumatic cardiac arrest in 152 thoracotomy patients[J]. Scand J Trauma Resusc Emerg Med, 2014, 22(1): 1.
[9] 黃一. 严重胸部撞击伤后肺组织NIX表达与肺泡细胞凋亡的关系及意义[D].重庆:第三军医大学, 2012.
[10] Bradley M J, Bonds B W, Chang L, et al. Open chest cardiac massage offers no benefit over closed chest compressions in patients with traumatic cardiac arrest[J]. J Trauma Acute Care Surg, 2016, 81(5): 849-854.
[11] Voiglio E J, Simms E R, Flaris A N, et al. Bilateral anterior thoracotomy (clamshell incision) is the ideal emergency thoracotomy incision: an anatomical study: reply[J]. World J Surg, 2014, 38(4): 1003.
[12] Vassiliu P, Yilmaz T, Degiannis E. On the ideal emergency thoracotomy incision[J]. World J Surg, 2014, 38(4): 1001-1002.
[13] 赵兴吉. 严重胸部创伤早期救治的几个重要问题[C]// 中华医学会急诊医学分会第十三次全国急诊医学学术年会大会论文集. 2010:565-566.
[14] Kleber C, Giesecke M T, Lindner T, et al. Requirement for a structured algorithm in cardiac arrest following major trauma: epidemiology, management errors, and preventability of traumatic deaths in Berlin[J]. Resuscitation, 2014, 85(3): 405-410.
[15] Struck M F, Staab H, Schummer W, et al. Traumatic cardiac arrest: central venous cannulation under direct vision following rescue thoracotomy[J]. Eur J Emerg Med, 2016, 23(1):74-75.
[16] 中华医学会创伤学分会创伤危重症与感染学组, 创伤急救与多发伤学组. 胸部创伤院前急救专家共识[J]. 中华创伤杂志, 2014, 30(9):861-864.
[17] Ohrt-Nissen S, Colville-Ebeling B, Kandler K, et al. Indication for resuscitative thoracotomy in thoracic injuries-Adherence to the ATLS guidelines. A forensic autopsy based evaluation[J]. Injury, 2016, 47(5):1019-1024.
[18] Inaba K, Chouliaras K, Zakaluzny S, et al. FAST ultrasound examination as a predictor of outcomes after resuscitative thoracotomy: a prospective evaluation[J]. Ann Surg, 2015, 262(3):512-518.
第一作者:刘宗志,硕士,主治医师,研究方向:危重胸部创伤的救治、晚期肺癌的综合治疗,Email:caaclzzz@163.com。