Clinical Study on the Treatment of Neonatal Jaundice with Lidan Tuihuang Formula Combined with Bifid Lriple Viable and Blue Ray Irradiation
Wu Qinglin (吴青林), Wng Weny (王文雅), Xun Xingyun (宣相云),Gu Ruiyu (谷瑞瑜), Yn Ynn (闫雅男)
a. Department of Pediatrics, the Second Hospital of Fengrun District, Tangshan, 063030, China
b. Department of Gynecology and Obstetrics, the Second Hospital of Fengrun District, Tangshan, 063030, China
ABSTRACT OBJECTIVE: To observe the clinical efficacy of Lidan Tuihuang formula combined with Peifeikang and blue light irradiation in the treatment of neonatal jaundice. METHODS: a total of 140 cases of neonatal jaundice were randomly divided into the observation group and the control group, with 70 cases in each group. The control group was treated with blue light irradiation and oral Bifid Lriple Viable, on the basis of conventional clinical interventions. The observation group was treated with Lidan Tuihuang formula on the basis of the control group. After 7 days of treatment,the scores of clinical symptom (skin yellowness, reduced milk volume, constipation, abdominal distension) and level of serum bilirubin before and after treatment were compared between the two groups, and the adverse reactions and clinical recurrence of the 2 groups were statistically analyzed. RESULTS: After treatment, the effective rate was 94.3%in the observation group which was significantly higher than that in the control group (77.1%) (P < 0.05). The degree of yellowing of the skin, the reduction of the amount of milk, the concentration of constipation and the distension of bloating were all significantly reduced in the 2 groups after treatment (P < 0.05), and the improvement of the above indexes in the observation group was significantly better than that in the control group (P < 0.05). The level of serum bilirubin was significantly lower in the 2 groups after treatment and even for 2 weeks after treatment (P < 0.05). The improvement level of serum bilirubin in the observation group after treatment and even for 2 weeks after treatment were significantly better than that in the control group (P < 0.05). The recurrence rate in the observation group was 8.7%,which was significantly lower than that in the control group 22.2 % (P < 0.05); No serious adverse reactions occurred in both groups. CONCLUSION: The combination of Lidan Tuihuang Formular, Bifid Lriple Viable, blue light irradiation for neonatal jaundice can rapidly improve the clinical symptoms of children, reduce the level of serum bilirubin and shorten the treatment time, with no obvious adverse reactions and high clinical safety.
KEYWORDS: Neonatal jaundice; Lidan Tuihuang Fomular; Bifid Lriple Viable; Blue light irradiation; Serum bilirubin
Neonatal jaundice refers to a pathological state, in which the blood bilirubin level of newborns under 28d is significantly increased, and then yellow staining of the skin mucosa and sclera occurs as the main clinical manifestation[1]The disease is clinically divided into physiological jaundice and pathological jaundice. The former can naturally fade in a certain period of time while the latter is more serious. The level of bilirubin in children is much higher than normal, if it is not promptly treated. The bilirubin easily penetrates into brain tissue,causing irreversible damage to the brain tissue, which in turn causes hearing, mental and motor dysfunction, and severe cases can lead to death[2].
At present, the treatment of neonatal jaundice by western medicine mainly includes drug therapy, blood exchange transfusion and blue light therapy. Although certain effect was achieved, there are shortcomings of the treatment, such as side effects, high cost , single treatment etc.[3]. In recent years, in-depth research on neonatal jaundice has been conducted by Chinese medicine and Rich unique treatment experience has been accumulated.It can conduct treatment of syndrome differentiation,according to the children's own conditions, and is supplemented with conventional western medicine treatment. It can not only rapidly reduce the level of serum bilirubin, shorten the course of the disease, but also can effectively reduce the occurrence of serious complications and sequelae, with a significant efficacy.From May 2016 to May 2017, the authors observed the clinical efficacy of Lidan Tuihuang formular and Bifid Lriple Viable in the treatment of neonatal jaundice. The results are as follows:
CLINICAL MATERIAL
General information
A total of 140 cases of neonatal jaundice admitted in our hospital during the above period were selected.The diagnostic criteria of neonatal jaundice in diagnosis of western medicine were based on the "Practical Neonatal Studies"[4]. The rules Neonatal jaundice occurs within 24 hours after birth, and serum bilirubin is higher than 102umol/L; ② Serum bilirubin in preterm infants is highe than 255umol/L, and full term infants are higher than 220.6umol/L serum bilirubin. ③ Neonatal serum bilirubin increases more than 85umol/L daily;④ The direct bilirubin of neonatal serum is higher than 26umo/L, and jaundice lasts more than 2-4 weeks or progressive aggravation occurs. The diagnosis of TCM was based on the "TCM syndrome diagnosis and treatment criteria and prescription selection"[5]in which there is rules for the yellow and hot fumigation of the fetus: the skin is yellow, the appearance of the skin is yellow; the color is bright; the shape is orange; the abdomen is full; the baby is the irritated and is crying;constipation is gray; the baby is with yellow urine, red tongue, greasy yellow coating and fingerprints lag.
All children, with breast feeding, had various degrees of yellowing on the face or other parts of the skin. The Apgar's score was 8 points. The mother of the child had no special medication history during pregnancy.All parents of all children signed informed consent form.Neonates with neonatal hepatitis, neonatal immune hemolysis, congenital inherited metabolic diseases,critical newborns, children with congenital malformation,with a history of family history and with drug allergy were excluded in this study They were randomly divided into 2 groups with 70 cases in each. In the observation group: 42 males and 28 females; age 3-14 (7.3±0.8)days; body weight 2500-4120 (2976.8±273.6) days;52 full-term, 12 premature and 6 late-born infants. The control group was consisted of 48 males and 22 females.The age ranged from 4 to 13 (7.5±0.7) days, and the body weight was from 2480 to 4200 (2913.7±268.5) g.There were 50 full-term, 16 premature, and 4 late-term infants. There was no statistically significant difference in gender and age between the 2 groups (P > 0.05).
Treatment method
The control group was given warmth, feeding,the routine clinical intervention to prevent infection,and the treatment of blue light irradiation. After 8 h of irradiation,it stopped for 12-16h, with continuous treatment for 7d. Oral Bifid Lriple Viable (Shanghai Xinyi Pharmaceutical Co., Ltd., The Chinese medicine accurate character 21390S050, specification: 210mg*24s) was given to the control group, 1 grain/time, 3 times/d, with continuous treatment 7d. The observation group was given oral Lidan Tuihuang Formula, on the basis of treatment in the control group: Semen Coicis 12g, Rhizoma Imperatae 12g, Medulla Junci 3g, Radix et Rhizoma Glycyrrhizae 2g, Cortex Phellodendri Amurensis 1.5g, Rhizoma Coptis 1.5g, Radix Scutellariae 1.5g and Herba Artemisiae Scopariae 1.5g. The above herbs were decocted in 500 ml of water, and the dection was collected into 150 ml,and the residue was removed. The decoction was given twice a day in the morning and evening before meal. One dose a day and 1 weak was a course of treatment.
Observation index ① Clinical efficacy: Based on the "TCM syndrome diagnosis treatment criteria and prescription selection"[6], it is divided into 4 treatment criteria: Cured: after treatment, jaundice in children is completely subsided and the level of serum bilirubin is less than 102.6umol/L or TCB is less than 6mg/dl; Improved: after treatment, jaundice is subsiding significantly and the level of serum bilirubin decreases by more than 50%; Invalid: after treatment, there is no significant improvement in children skin and scleral yellow stain and no obvious reducing level of serum bilirubin. Cured + improvedr = effective. ② Clinical symptom scores: the degree of skin yellowing, milk volume reduction, constipation, and abdominal distension improvement of children before and after treatment were observed and recorded. The higher the score, the more severe the symptoms are. ③ Serum bilirubin: The changes of serum bilirubin level were compared before and after treatment and after 2 weeks. ④ Recurrence:After treatment, 2 groups of cured children were followed up for 2 weeks, and 2 groups of relapse were compared.⑤ Adverse reactions: statistics on the adverse reactions occurred during treatment of 2 groups of children.
Statistical methods: SSPS 22.0 statistical software was used for statistical analysis. The measurement data is represented by (x–±S), and the t-test is used for comparison. The count data is represented by n (%) and x2test is used for comparison. P < 0.05 was considered statistically significant for the diference.
RESULTS
Comparison of clinical efficacy after treatment of the 2 groups:
After treatment, the effective rate was 94.3% in the observation group and 77.1% in the control group.The difference between the 2 groups was statistically significant (P < 0.05). See Table 1.
Comparison of the score of clinical symptom before and after treatment of the 2 groups.
Before treatment, there was no significant difference in the degree of skin yellowing, the reduction of milk volume, constipation, and abdominal distension score between the two groups (P < 0.05). After treatment, the scores of the degree of yellowing of the skin, reduction of milk volume, constipation, and abdominal distension were significantly reduced in both groups (P < 0.05), and the improvement of the above symptom scores in the observation group was significantly better than that in the control group (P < 0.05). See Table 2.
Comparison of the level of serum bilirubin before and after treatment of the 2 groups
Before treatment, there was no significant difference in the level of serum bilirubin between the two groups(P < 0.05). The level of serum bilirubin were significantly lower in the 2 groups after treatment and 2 weeks after treatment (P < 0.05), and the improvement of the level of serum bilirubin in the observation group after treatment and 2 weeks after treatment was significantly better than that in the control group (P < 0.05). See Table 3.
Comparison of recurrence of the 2 groups:
The recurrence rate in the observation group was 8.7% of the cured children, and 22.2% in the control group. The difference between the 2 groups was statistically significant different (P < 0.05). See Table 4.
Comparison of adverse reactions between the 2 groups:
During the treatment period, 2 patients of the observation group had a slight eczema. 1 patient in the control group had a slight eczema. No treatment wasgiven to them and they faded away spontaneously after 24 hours. No serious adverse reactions such as fever and diarrhea occurred in the two groups of children. There were adverse reactions in blood routine, urine routine,and liver and kidney function during the treatment of all the babies.
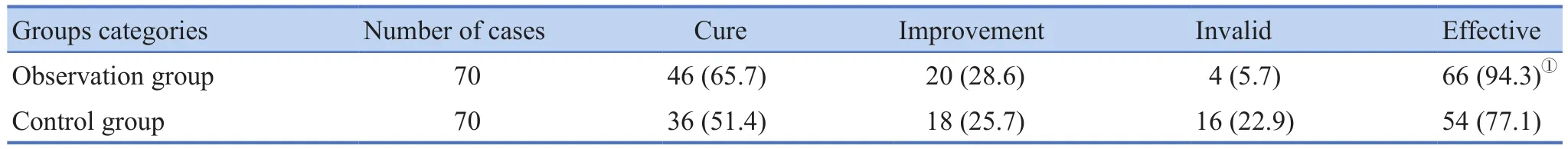
Table 1. Comparison of the Clinical Efficacy of the Two Groups n (%)
Table 2. Comparison of the scores of clinical symptom before and after treatment of the 2 groups ((±S), Score )
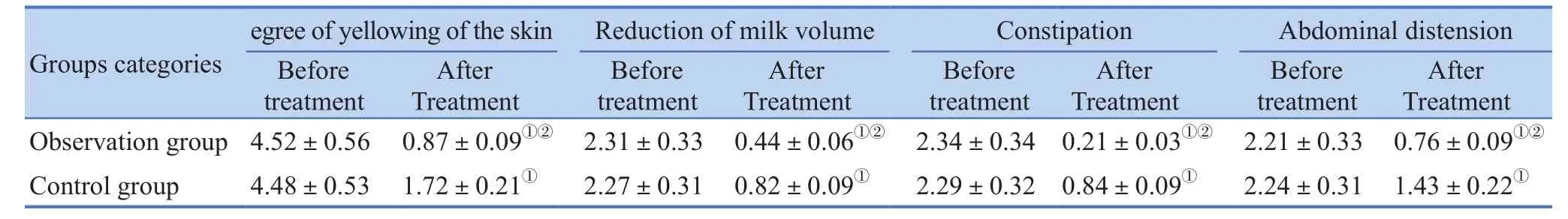
Table 2. Comparison of the scores of clinical symptom before and after treatment of the 2 groups ((±S), Score )
Note: compared with that before treatment, P < 0.05; 2 compared with the control group, P < 0.05.
Groups categories After Treatment Observation group 4.52±0.56 0.87±0.09①② 2.31±0.33 0.44±0.06①② 2.34±0.34 0.21±0.03①② 2.21±0.33 0.76±0.09①②Control group 4.48±0.53 1.72±0.21① 2.27±0.31 0.82±0.09① 2.29±0.32 0.84±0.09① 2.24±0.31 1.43±0.22①Before treatment After Treatment Before treatment After Treatment Before treatment After Treatment Before treatment
Table 3. Comparison of of serum bilirubin (±S, μmol/L)

Table 3. Comparison of of serum bilirubin (±S, μmol/L)
Note: 1 compared with that before treatment, P < 0.05; 2 compared with the control group, P < 0.05.
observation group 70 355.02±33.62 171.47±18.26①② 102.31±11.71①②Control group 70 352.78±35.18 241.34±24.31① 131.46±14.59①
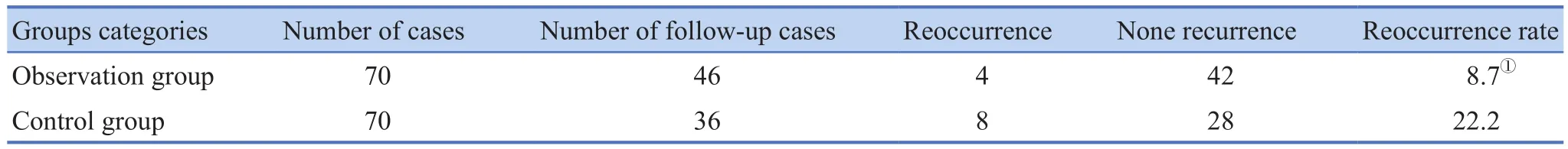
Table 4. Comparison of recurrence n (%)
DISCUSSION
Neonatal jaundice is neonatal hyperbilirubinemia,which is mainly due to abnormalities of bilirubin metabolism that increase bilirubin of neonatal body,resulting in yellowing of the skin mucous membrane and sclera. Clinically, it occurs frequently in neonates ,2 to 3 days after birth.[6]. Newborns have poor resistance of blood-brain barrier, low level of plasma protein, and imperfect immune function. After jaundice develops in babies, they can easily lead to a series of jaundice syndromes, such as infection and poisoning, even bilirubin encephalopathy[7], causing severe sequelae and even endangering the safety of newborns[8].
The pathogenesis of neonatal jaundice is comparatively complicated. The main cause of neonatal jaundice is the immature development of various organs of newborns and the relatively low function of various systems. The lower threshold of blood-brain barrier function through bilirubin is found in babies. Bilirubin is easily accumulated in the body through the bloodbrain screen, causing elevated bilirubin in the body[9].Additionally, some neonates have less intestinal flora after birth due to late milking or less milking, which means that bilirubin cannot be excreted intostercobilinogen and urobilinogen by intestinal flora in intestine. It can aggravate jaundice[10]. In addition, the activity of neonatal intestinal β-glucuronidase (β-GD) is high, which is easy to decompose conjugated bilirubin into non-conjugated bilirubin, and then through the enterohepatic circulation back into the body to lead to hyperbilirubinemia[11].Therefore, reducing the intestinal reabsorption of bilirubin and promoting the excretion of intestinal bilirubin is one of the most effective measures for the clinical treatment of neonatal jaundice.
Neonatal jaundice belongs to the category of"fetal yellow" in traditional Chinese medicine, and it is believed by Chinese medicine that the disease is caused by exogenous wetness during conception, which transferred into hyperthermia. Then it transmitted into neonatal birth, which instantly infects external pathogen,entering inside of the body, transferred into heat, and then accumulating in the middle Jiao. Damp-heat steams liver and gallbladder, so that the liver qi could not smoothly drain and then invading gallbladder, resulting in bile leakage, overflowing the skin and resulting madding newborn yellow. It can be seen that liver leakage and bile leakage are the main causes of neonatal jaundice.Therefore, treatment should be based on the principles of liver-soothing, gallbladder and jaundice leakage.In this study, Lidan Tuihuang Formula is consisted of Semen Coicis, Rhizoma Imperatae, Medulla Junci 3g,Radix et Rhizoma Glycyrrhizae, Cortex Phellodendri Amurensis, Rhizoma Coptis , Radix Scutellariae and Herba Artemisiae Scopariae, in which, Herba Artemisiae Scopariae is chief medicinal, and it could clear heat and drain dampness,and is beneficial to gallbladder and yellow fading. Cortex Phellodendri Amurensis, Rhizoma Coptis, Radix Scutellariae are all chief medicinal, which has the function of clearing heat, drying dampness,draining fire and resolving toxins. Semen Coicis,Rhizoma Imperatae, Medulla Junci are all assistant medicinal, among which Semen Coicis, which has the function of fortifying the spleen, draining dampness,clearing heat and expelling toxin. Rhizoma Imperatae has the function of clearing heat being diuresis, cooling blood and stop bleeding. Medulla Junci can clear heat and resolve toxins, and it can also eliminate wetness. Radix et Rhizoma Glycyrrhizae has the function of clearing heat and resolving toxins. Mixing the medicinal above means envoy medicinal.All chief, deputy, assistant and envoy the above-mentioned properly complemented with each other and have the function of eliminating dampness and yellowness. Modern pharmacological studies have shown that Herba Artemisiae Scopariae can effectively relax the biliary sphincter, promote biliary secretion and bilirubin excretion, and can enhance the liver's ability to uptake, bind and excrete bilirubin by inducing the liver enzyme system. It can also reduce the harm of the bacterial metabolites to liver, so as it can achieve the purpose of treating jaundice[12]; Radix Scutellariae is mainly consisted of Astragalus, Astragalus and lutein,promoting urinary excretion, and significantly improving the permeability of capillaries; Rhizoma Coptis has a broad-spectrum antibacterial antiviral effect and can effectively inhibit the increase of serum bilirubin and protect the liver. Cortex Phellodendri Amurensis has a good broad-spectrum antibacterial effect, especially for staphylococcus aureus, streptococcus pneumoniae,and pseudomonas aeruginosa. Therefore it has certain effect on jaundice.[13]. Semen Coicis has effects as follows: such as antioxidant, scavenging free radicals,antibacterial, antiviral, immune regulation etc.[14].Rhizoma Imperatae has the obviously anti-inflammatory,antibacterial effect, and can effectively enhance the body's non-specific immune function[15]. Medulla Junci is beneficial to liver, anti-inflammatory, antibacterial,sedative etc. Liquor ice root has the function of anti-virus and immune regulation.
The results of the study showed that the effective rate in the observation group after treatment was significantly higher than that in the control group. The recurrence rate was significantly lower than that in the control group after 2 weeks of discontinuation. The improvement of the scores of the clinical symptom and the level of serum bilirubin in the observation group were significantly better than that in the control group. No serious adverse reactions occurred during the treatment of both groups. It is suggested that the treatment of neonatal jaundice with the combination of gallbladder and jaundice combined with Bifid Lriple Viable and blue light irradiation can rapidly improve the clinical symptoms of babies, reduce the level of serum bilirubin and shorten the treatment time. It has no obvious adverse reactions, is of high clinical safety. It is a new direction for the treatment of neonatal jaundice.
REFERENCE
1. Wang ZH. Analysis of the efficacy of Bifid Lriple Viable and blue light irradiation in the treatment of neonatal jaundice.Journal of Clinical Medicine Research, 2016,1(20):141,143.
2. Huang YC, Peng YH. Comparison of efficacy of blue light intermittent irradiation and continuous irradiation by blue light with Huangqi Yinchen Granules for the Treatment of Neonatal Jaundice. Modern Journal of Integrated Traditional Chinese and Western Medicine, 2014, 23(35):3944-3946, 3974.
3. Wu XN, Fei JL, Chen YY. Research development of neonatal jaundice treated by Chinese and Western medicine. Journal of Pediatrics of Traditional Chinese Medicine, 2013,9(3):52-55.
4. Shao XM, Ye HY, Qiu XY. Practical neonatal studies. 4.Beijing: People's Medical Publishing House, 201l:273-274.
5. Shen S, Xue JG, Yue PP, et al. Standard of TCM syndrome diagnosis and prescription selection. Beijing: People's Medical Publishing House, 2001:205.
6. Zhou Q. Clinical efficacy of Yinzhihuang oral liquid combined with blue light irradiation in the treatment of neonatal jaundice.Chinese Journal of Clinical Medicine, 2015,8(12C): 20-21.
7. Qian JW. Comparison of the clinical efficacy of Mammy love and Bifid Lriple Viable in the treatment of neonatal jaundice.Journal of Pediatrics of Traditional Chinese Medicine, 2011,7(6): 27-29.
8. Zhang CH. Therapeutic effect of Yinzhihuang oral liquid combined with Bifid Lriple Viable and Smecta on treating pathological neonatal jaundice.Contemporary Medicine,2016,22(13):151-152.
9. Zhang CL, Zhang J, Liu YH, et al. Clinical efficacy of Bifidobacterium triple live bacteria tablets in the treatment of neonatal jaundice. Clinical Rational Drug Usage, 2015,8(9A): 98-99.
10. Meng WF. Observation of the effects of blue light irradiation combined with Bifid Lriple Viable on neonatal jaundice.Journal of Qiqihar Medical College, 2015,36(7): 1004-1005.
11. Yao JH, Li XY, Zhang XH, et al. Randomized multicenter clinical efficacy of clostridium butyricum in the treatment of neonatal jaundice . Chinese Journal of Micro ecology, 2016,28(10): 1178-1180.
12. Cao JH. Research development of chemical constituents and pharmacological effects of Artemisia capillaris. Journal of Shenyang Pharmaceutical University, 2013, 30(6): 489-494.
13. Xiong M. Analysis of chemical composition and pharmacological effects of Phellodendron chinense. Asia-Pacific Traditional Medicine, 2014, 10(14): 34-35.
14. Guo Y, Cao BL. The pharmacological effects of the seed of job's tear and its application in dermatology. Journal of Clinical Medicine, 2015, 2(15): 3145-3146.
15. Liu J. Chemical constituents, pharmacological effects and clinical application of woolly grass. Shandong Journal of Traditional Chinese Medicine, 2014, 33(12): 1021-1024.
 World Journal of Integrated Traditional and Western Medicine2018年3期
World Journal of Integrated Traditional and Western Medicine2018年3期
- World Journal of Integrated Traditional and Western Medicine的其它文章
- World Integrated Medicine Master Han Jisheng
- Consensus on Epigastralgia Diagnosis and Treatment of Chinese Medicine (2017)
- Effect of Qiangli Dingxuan Tablet on Cerebral Hemodynamics and Brainstem Auditory Evoked Potentials in Vertigo Patients with Posterior Circulation Ischemia
- Quality Evaluation on Traditional Chinese Medicine Nursing Plan for Stroke in Acute and Recovery Phases
- Enlightenment from WHO Pharmacovigilance in Construction of Chinese Materia Medica Pharmacovigilance System
- Profiling the Change of Key Chemical Ingredients in Combination of Aconitum carmichaeli Debx. and Bletilla striata (Thunb.)Reichb.f. by UPLC-QTOF/MS with Multivariate Statistical Analysis
