Intravitreal bevacizumab versus bevacizumab and 1 mg triamcinolone acetonide in eyes with bilateral diabetic macular edema
Sever Ozkan1, Horozoglu Fatih1,Celik Erkan2,Topcu Birol
1Department of Ophthalmology, Namik Kemal University School of Medicine, Namik Kemal University, Tekirdag 59000, Turkey2Department of Ophthalmology, Sakarya Education and Research Hospital, Sakarya 54100, Turkey3Department of Biostatistics, Namik Kemal University School of Medicine, Namik Kemal University, Tekirdag 59000, Turkey
Abstract
•AIM: To compare of intravitreal bevacizumab and intravitreal bevacizumab and triamcinolone acetonide in eyes with bilateral diabetic macular edema.
•METHODS: In this retrospective comparative-randomized study, 42 eyes of 21 diabetic patients with bilateral macular edema were evaluated. In one eye intravitreal injection of 1.25 mg bevacizumab (IVB group) was performed and in the fellow eye intravitreal injection of combined 1.25 mg bevacizumab and 1 mg triamcinolone acetonide (IVTA-IVB group) was performed. Main outcomes were the central macular thickness (CMT) measured with optical coherence tomography (OCT), ETDRS visual acuity (VA) and intraocular pressure (IOP).
•RESULTS: Mean follow-up time was 4.7±1.5mo. In the IVB and IVTA-IVB groups, mean CMT was 494.7±114.4 μm and 546.8±165.6 μm before injections; 430.4±133.2 μm and 363.7±105.3 μm in first month; 484.8±167.4 μm and 407.3±108.7 μm in 3rd month; 550.4±191.5 μm and 516.8±158 μm after 6mo respectively. Differences were significant in first and 3rd months (P<0.05). In the IVB and IVTA-IVB groups, mean ETDRS VA score was 57.1±13.5 and 48.9±13.9 before injections; 62.2±14 and 58.8±12.1 in first month; 59±13.7 and 59.3±13.6 in 3rd month; 55.6±14.9 and 55.5±8.7 after 6mo respectively. Differences were significant in first and 3rd and 6mo (P<0.05). There was no IOP difference. IVTA-IVB group gains best VA in 3rd month after the first injection and maintains it for 6mo whereas IVB group gains best VA at first month and can be able to maintain for 3mo.
•CONCLUSION: Injection of 1 mg IVTA-IVB seems to be better than IVB alone in improving VA for 6mo without any steroid dependent complications.
•KEYWORDS:diabetic retinopathy; triamcinolone acetonide; bevacizumab
INTRODUCTION
Diabetic macular edema (DME) is the most common cause of visual impairment in patients with diabetic retinopathy[1]. Laser photocoagulation has been the standard-of-care treatment for DME for decades, based on the Early Treatment Diabetic Retinopathy Study (ETDRS) and other more recent clinical trials[2-3]. Later it was reported that the improvement in visual acuity (VA) occurs in only about 17% of treated eyes and laser treatment causes many complications such as laser scars that can enlarge postoperatively, leading to decreased vision[2-4]. Intravitreal triamcinolone (IVT) showed to have a beneficial effect on macular thickness and VA in eyes with DME, with a probable mechanism of increase in tight junction proteins, which diminish vessel leakage by a local vasoconstrictive effect and angiostatic properties through inhibition of vascular endothelial growth factor (VEGF). Corticosteroids block the arachidonic acid pathwayviaphospholipase A2 inhibition. This inhibits the synthesis of thromboxanes, leukotrienes and prostaglandins and prevents vasodilation and increased capillary permeability. Corticosteroids also stabilize lysozymes, reduce synthesis of inflammatory mediators and VEGF, inhibit cell proliferation, stabilize the BRB, enhance the density and activity of tight junctions in the retinal capillary endothelium, and improve retinal oxygenation[5]. However, its effect is temporary and side effects such as cataract formation and intraocular pressure (IOP) elevation have been reported in a significant percentage of cases[6-7]. VEGF plays as an important factor in the breakdown of the blood-retinal barrier and increased vascular permeability in diabetic eyes and recent studies have revealed elevated VEGF levels in the vitreous of patients[9-10]. There is an increasing trend for use of intravitreal bevacizumab (IVB) (a humanized full-length monoclonal antibody that inhibits all isoforms of VEGF) for DME[11-13].
Various modalities of treatment are currently being tried in the management of DME such as supplemental laser, intravitreal steroids, anti-VEGF drugs and combination of these procedures. The aim of this study was to compare the effectiveness and safety of only IVB versus combination of IVB and IVT in eyes with bilateral DME.
SUBJECTS AND METHODS
SubjectsThe study protocol adhered to the tenets of the Declaration of Helsinki and was approved by the local Institutional Review Board and all participants gave written informed consent before injections.
PatientEligibilityandBaselineEvaluationTwenty-one consecutive diabetic patients with bilateral DME, whose foveal thickness was more than 300 μm in both eyes were recruited in this study. All the patients were among those without any health insurance and could not afford repeated therapies and novel drugs. Exclusion criteria were: 1) vitreoretinal traction on spectral-domain optical coherence tomography (OCT); 2) history of glaucoma or ocular hypertension; 3) an ocular condition that, in the opinion of the investigator, might affect macular edema or alter VA during the course of the study (eg. uveitis, retinal vein occlusion, epiretinal membrane, age-related macular degeneration, recently performed cataract surgery, macular laseretc.); 4) systemic corticosteroid therapy; 5) any condition that, in the opinion of the investigator, might preclude follow-up throughout the study period such as high blood sugar levels and high blood pressure levels.
IntravitrealInjectionForty two eyes of 21 diabetic patients with bilateral DME were randomly assigned. In each patient, 1.25 mg of bevacizumab (Avastin; Genetech, Inc, South San Francisco, California, USA) was injected into the vitreous in one eye, and combination of 1.25 mg bevacizumab and 1 mg of triamcinolone acetonide (Kenacort; Bristol-Myers Squibb, Tokyo, Japan) was injected in the other eye. Injections to each eye was made separately at different times using different drape sets. Both drugs were prepared in different injectors and first we administered intravitreal triamcinolone and than we removed the injector but not the needle from the eye and second injection was applied thorough the same needle. All injections were performed using topical proparacaine drops under sterile conditions (eyelid speculum, povidone-iodine and draping). Before the injection was performed, the eyelids Independent samplettestP<0.05, Pearson correlation test. IVTA: Intravitreal triamcinolon+bevacizumab; IVB: Intravitreal bevacizumab.
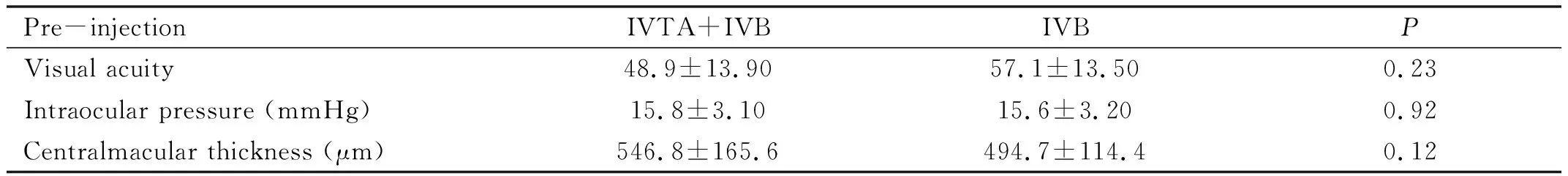
Table 1 Pre-injection demographic featuresmean±SD
were scrubbed with 10% povidone-iodine, and 5% povidone-iodine drops were applied to the conjunctiva. The time between application of 5% povidone-iodine solution to the conjunctiva and administration of the intravitreal injection was 2min. Povidone-iodine was applied to the conjunctiva directly over the intended injection site. Care was taken in all cases to insure that the needle did not touch the lids or lashes. Afterwards, 0.05 mL volume containing 1.25 mg of bevacizumab or 0.1 mL volume containing the combination of 1.25 mg of bevacizumab and 1 mg of triamcinolone acetonide was injected into the vitreous cavity using a sharp 27-gauge needle through the superotemporal quadrant at a distance of 3.5-4 mm from the limbus. Central retinal artery perfusion was confirmed with indirect ophthalmoscopy and right after the injections their IOP were measured with air tonometry (Canon Tx10, non-contact tonometry). IOP till 25 mmHg were accepted as normal. Patients were instructed to instill one drop of 0.5% moxifloxacin hydrochloride (Vigamox, Alcon Lab., Fort Worth, USA) into the injected eye 4 times daily for 1wk after the procedure.
Follow-upExaminationsandOutcomeMeasuresAfter the injections 1stday, 1stweek, 1stmonth, 3rdmonth and 3mo intervals thereafter were the time points for examination. At these visits, patients’ VA was determined after ETDRS refraction, and they underwent complete ophthalmic examination using the same procedures as at baseline. Main outcome measures were the changes in the ETDRS VA and central macular thickness (CMT) measured with OCT, and IOP and occurence of complications.
StatisticalAnalysisOne-Way ANOVA, Independent samplet, Mann-WhitneyU, Paired samplettest and Wilcoxon tests were used for statistical analysis (SPSS for Windows, version 18.0, SPSS, Chicago, IL, USA). APvalue of less than 0.05 was considered to be statistically significant.
RESULTS
Forty two eyes of 21 patients (11 females, 10 males) with bilateral DME were studied. The ages of patients ranged from 46-89y with a mean of 65.4±8.9y. The mean follow-up period was 4.7±1.5mo (range: 3-6mo, 6mo for 12 patients, 3mo for 9 patients). The duration of diabetes ranged from 20.5±9.77 (8-30)y and the mean level of HbA1c was 9.1±2.2 mg/dL. Fifteen patients had hypertension as accompanying systemic disease. Five eyes had proliferative diabetic retinopathy and 18 patients had a history of focal and panretinal photocoagulation treatment.
Before the administration of the drugs, CMT obtained by OCT was 494.7±114.4 μm in the IVB group, and 546.8±165.6 μm in the IVB + IVTA group, and there was no significant difference between them (P=0.243). Also, there was no significant difference in initial VAs (57.1±13.50 in IVB, 48.9±13.90 in IVTA + IVB,P=0.59) and IOPs (15.6±3.20 mmHg in IVB, 15.8±3.10 mmHg in IVTA + IVB,P=0.779) between two groups (Table 1).
OutcomeMeasures
秀容月明屡战屡胜,收复十一座城池;雁门关外,以千余牛羊引诱胡人,再以一万秀容兵大破胡人七万精骑;阴山大捷,活捉左贤王、斩杀右贤王……皇上御笔亲书“秀容月明”帅旗,赐秀容月明衣甲、锦缎、玉带、田宅;秀容月明破敌有功,封为渔阳、上谷等七城节度使……只要秀容月明的捷报传来,只要秀容月明又升官了,京城内外必然流言四起,说什么的都有。
VisualacuityAt baseline, mean ETDRS scores were 57.1±13.5 and 48.9±13.90 in the IVB and IVTA + IVB groups, respectively. After the injections 1stday, 1stweek, 1stmonth, 3rdmonth and 6thmonth mean ETDRS scores were 49.8±13.07, 54.7±12.7 and 57.5±12.6, 60.4±12.05 and 58.8±12.1, 62.2±14 and 59.3±13.60, 59±13.70 and 55.5±8.7, 55.6±14.9 in the IVTA + IVB and IVB groups, respectively. We observed that IVTA-IVB group gains best VA at 3rdmonth after the first injection and maintains it for 6mo; whereas, IVB group gains best VA at first month and can be able to maintain for 3mo.
Intragroup VA improvement in IVB alone group was statistically significant in 1stweek (P<0.01) and 1stmonth (P<0.04). However, 3rdmonth (P<0.23) and 6thmonth (P<0.875) improvements were not statistically significant. Intragroup VA improvement in IVTA + IVB group was statistically significant in 1stweek (P<0.01), 1stmonth (P<0.04), 3rdmonth (P<0.01) and 6thmonth (P<0.03). Between these two groups, there was a statistically significant difference of VA at the time of all visits (1stday, 1stweek, 1stmonth, 3rdmonth and 6thmonth). VA changes are summarized in the Table 2, Figures 1 and 2.
CentralmacularthicknessAt baseline, mean CMT was 494.7±114.4 μm and 546.8±165.6 μm in the IVB and IVTA+IVB groups, respectively (P=0.243) and 430.4±133.2 μm and 363.7±105.3 μm at first month, 484.8±167.4 μm and 407.3±108.7 μm at 3rdmonth, 550.4±191.5 μm and 516.8±158 μm after 6mo respectively. Comparison of differences between the two groups was significant at first 3mo (P<0.05). CMT changes are summarized in the Table 3 and Figures 3, 4 and 5.
For the eyes treated with IVTA + IVB, intragroup statistically significant reduction in CMT, compared with baseline, was observed at 1stweek (P<0.05), 1stmonth (P<0.05) and 3rdmonth (P<0.05) follow-up visits. However, 6thmonth CMT change was not statistically significant (P<0.556). For the eyes treated with IVB, intragroup statistically significant
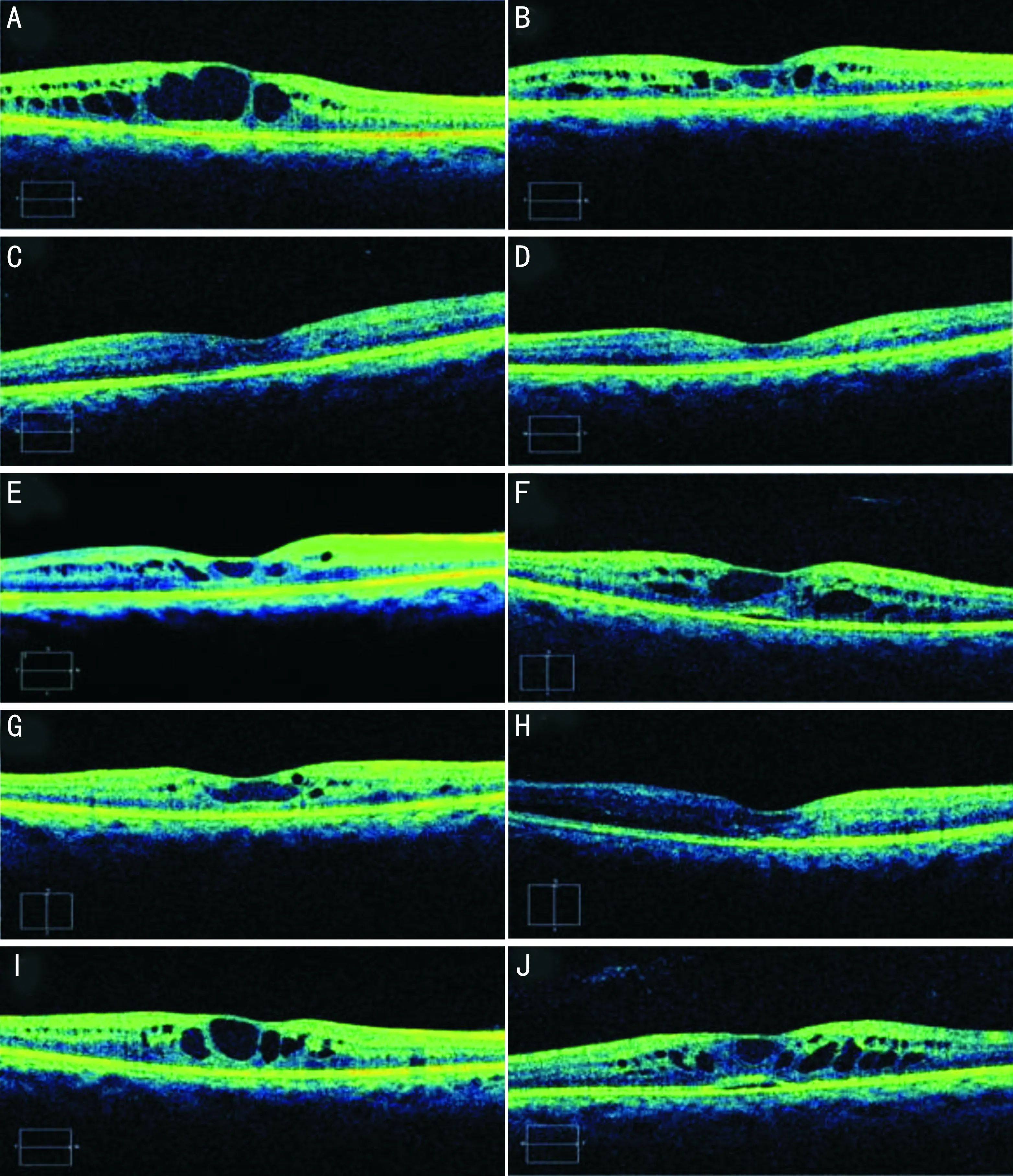
Figure1Pre-injection,post-injection1stweek,1stmonth,3rdmonthand6thmonthmacularopticalcoherencetomographychangesforcombinedintravitrealbevacizumabandtriamcinolone(Ontheleftcolumn)andonlybevacizumab(Ontherightcolumn)group.
Table2ComparisonofBCVAalterationsforcombinedIVTA+IVBgroupandonlyIVBgroup
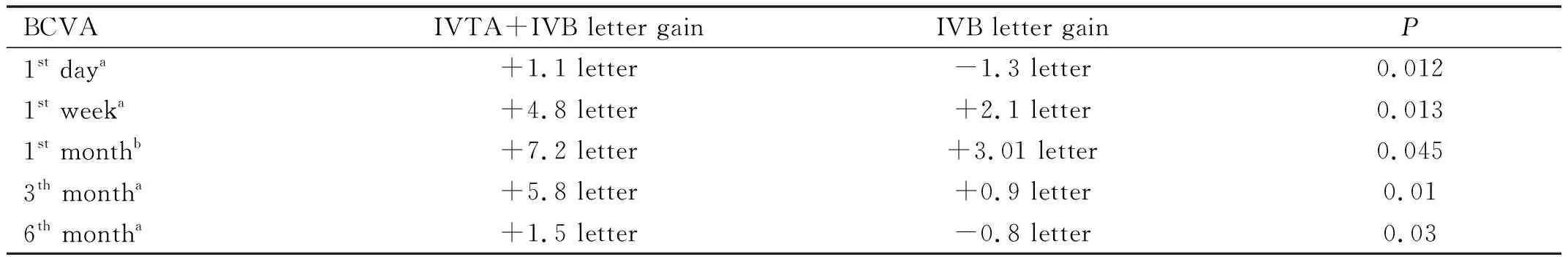
BCVAIVTA+IVB letter gainIVB letter gainP1st daya+1.1 letter-1.3 letter0.0121st weeka+4.8 letter+2.1 letter0.0131st monthb+7.2 letter+3.01 letter0.0453th montha+5.8 letter+0.9 letter0.016th montha+1.5 letter-0.8 letter0.03
aMann Whitney-UtestP<0.05;bIndependent SamplettestP<0.05. IVTA: Intravitreal triamcinolon+bevacizumab; IVB: Intravitreal bevacizumab; BCVA:Best-corrected visual acuity.
Table3ComparisonofCMTalterationsforcombinedIVTA+IVBgroupandonlyIVBgroup
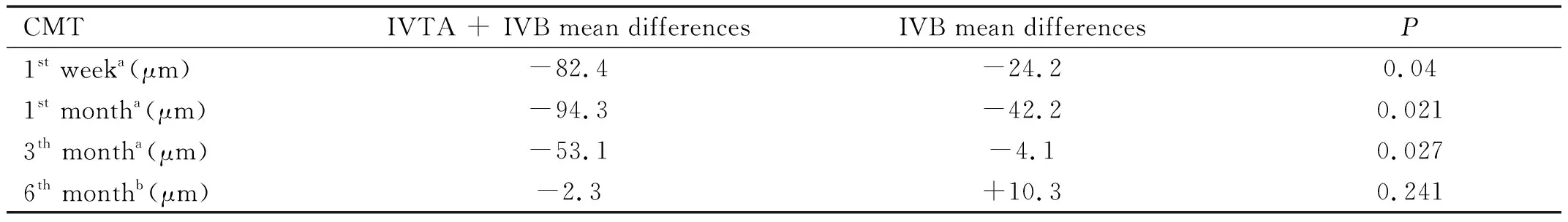
CMTIVTA + IVB mean differencesIVB mean differencesP1st weeka (μm)-82.4-24.20.041st montha (μm)-94.3-42.20.0213th montha (μm)-53.1-4.10.0276th monthb (μm)-2.3+10.30.241
aMann Whitney-UtestP<0.05.bIndependent SamplettestP<0.05. IVTA: Intravitreal triamcinolon+bevacizumab; IVB: Intravitreal bevacizumab; CMT: Central macular thickness.
Table4ComparisonofIOPalterationsforcombinedIVTA+IVBgroupandonlyIVBgroup
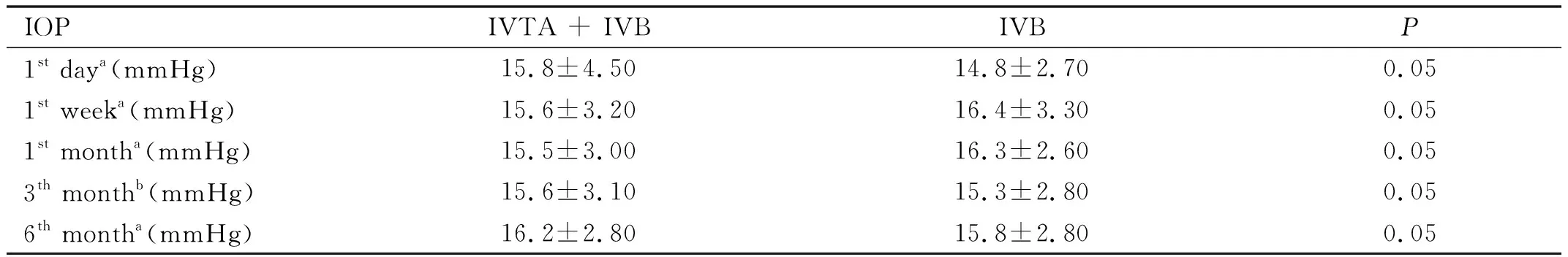
IOPIVTA + IVBIVBP1st daya (mmHg)15.8±4.5014.8±2.700.051st weeka (mmHg)15.6±3.2016.4±3.300.051st montha (mmHg)15.5±3.0016.3±2.600.053th monthb (mmHg)15.6±3.1015.3±2.800.056th montha (mmHg)16.2±2.8015.8±2.800.05
aMann Whitney-UtestP<0.05.bIndependent SamplettestP<0.05. IVTA: Intravitreal triamcinolon+bevacizumab; IVB: Intravitreal bevacizumab; IOP: Intraocular pressure.
reduction in CMT, compared with baseline, was observed only at 1stweek (P<0.031) and 1stmonth (P<0.034). However, 3rdand 6thmonth CMT changes were not statistically significant (P<0.366). We observed that IVTA-IVB group gains best VA at 3rdmonth after the first injection and maintains it for 6mo; whereas, IVB group gains best VA at first month and can be able to maintain for 3mo.
IntraocularpressureAt the initial examination, average baseline IOP was 15.6±3.2 mmHg and 15.8±3.1 mmHg in the IVB and IVTA + IVB groups, respectively. There was no statistically significant difference between the two groups initially (P=0.779). There was no significant change in mean IOP compared with baseline at any of the study follow-up visits in either group (P>0.05) (Table 4).
DISCUSSION
Although the molecular mechanisms of DME development are not completely understood, DME has been characterized by inflammation, including intravitreous induction of proinflammatory cytokine, intraretinal expression of proinflammatory caspases and mediators, therefore, many clinical investigators have found that intravitreal injection of a corticosteroid of triamcinolone acetonide may reduce macular edema[6,9]. And also, VEGF is a well-known potent angiogenic factor that is involved in the increased vascular permeability leading to macular edema and induces retinal neovascularization[13]. Since recent studies have shown that VEGF plays a major role in the pathogenesis of diabetic retinopathy, studies with anti-VEGF therapy showed dramatic reductions of DME[12,14-15].
Among recent treatments available for DME, intravitreal injections of triamcinolone acetonide and of bevacizumab have been shown to be safe, effective, visually and anatomically beneficial in most patients with DME[2,14]. Nonetheless, the exact mechanisms of these treatments and reasons for response to the treatment still remain unknown. In this study, we compared the effectiveness and safety of IVB alone versus combination of IVB and IVT in eyes with bilateral DME.
We observed that IVTA-IVB group gains best VA at 3rdmonth after the first injection and maintains it for 6mo; whereas, IVB group gains best VA at first month and can be able to maintain for 3mo. After the injections intragroup VA improvement in IVB alone group was statistically significant in 1stweek and 1stmonth . However, 3rdmonth and 6thmonth improvements were not statistically significant. Intragroup VA improvement in IVTA + IVB group was statistically significant in 1stweek, 1stmonth, 3rdmonth and 6thmonth. Between these two groups, there was a statistically significant difference of VA at the time of all visits (1stday, 1stweek, 1stmonth, 3rdmonth and 6thmonth).
There are so many studies comparing treatment modalities with IVB and IVTA on DME reporting different results. Treatment with IVB has been reported to be associated with favorable anatomic effects in patients with DME; the BOLT study reported a mean CMT reduction at 1y of 130 μm and improvement in VA, which is similar to a recent report from the Pan-American Collaborative Retina Study Group showing a dramatic decrease of DME[10,14]. In the study by Chakrabartietal[16], the response to therapy with bevacizumab showed superiority compared with TA for DME. In a study designed by and Mareyetal[17], comparing the efficacy of IVB alone and IVB-IVTA combination for primary treatment of DME, they concluded that IVB is an effective drug for DME, and has a long lasting effect compared with IVTA and also combined IVTA/IVB; they reported that, adding IVT does not affect the outcome measures except for elevating the IOP in treated patients in the early post-injection period. However, these studies differed from that of Shimuraetal[18], Paccolaetal[19], Isaacetal[20]and Limetal[21], who demonstrated that IVTA was more efficient in reducing DME relative to bevacizumab. And in the other study by Renschetal[22], IVTA and IVB did not differ markedly on VA and CMT. Soheilianetal[23]found that combination therapy with IVB and IVTA demonstrated no additional benefit in patients with DME when compared with IVB alone. Which treatment is more effective remains controversial.
In a Meta-analysis, including 6 studies comparing IVT versus IVB alone or IVB combined with IVT, they reported that the IVT group had a statistically significant improvement in vision over the IVB group, and this difference persisted to 3mo[24]. However, reduction in CMT was not significant during the earlier follow-up period (1mo and 3mo). At later visit (6mo), eyes that received IVT had a significant decrease in CMT while no siginificant improvement in VA was observed. With regards to IVT versus IVB combined with IVT, due to the inadequate data of VA, the Meta-analysis could not be assessed but there were no significant differences in CMT at 1mo and 3mo. The results of this study showed a favorable response to IVT compared with IVB in improvement of VA at 1mo and 3mo[24]. This Meta-analysis and other previous studies pointed out that there was no absolute correlation between anatomical change (CMT) and functional change (VA). Browningetal[26]indicated that not only CMT, but age, hemoglobin A1c, and severity of leakage in the center and inner subfields were responsible for change in VA. In another study managed by Kamoietal[27], they concluded the varying degree of macular ischemia may explain why some patients do not show a marked improvement in vision despite a regression of CMT.
In our study, the IVB+IVTA group demonstrated better improvements of VA and CMT, compared with IVB alone group. These results may be explained by the edema formation hypothesized by two theories: 1) increased permeability of vessels; 2) increased water flux from vascular to the tissue compartment[28]. VEGF is well known to increase vascular permeability; however, no report is available indicating that VEGF affects water flux through the vascular wall[29]. In contrast, TA reduces the expression of VEGF and thereby prevents the accumulation of fluid in the extracellular space[30-31]. In addition, DME is related with not only VEGF, but also IL-6, ICAM-1 and other cytokines[32-33]. TA affects a number of different cytokine including VEGF, thus it may be necessary to reduce more than one cytokine to make an effective reduction in DME[34]. From these aspects, TA is a multipotent drug, and therefore may have more advantages for regression of DME when compared with bevacizumab, which only reduces the amount of circulating free VEGF in the eye[6,18].
As in the previous clinical data, intravitreal application of bevacizumab or bevacizumab combined with TA are both tolerated well in most of patients[35-36]. Among the complications of IVTA, IOP elevation is the most common[37-40]. Ohetal[41]reported that 5 of 40 eyes developed temporary IOP elevation after IVTA injection and required temporary treatment. Gilliesetal[42]reported that over half of the eyes receiving IVTA injections for DME required cataract surgery within 3y. Chanetal[43]reported that, even if the ocular hypertensive effects were similar between the injection types, the cumulative effects of the intraocular steroids would lead to increased cataractogenesis, and each injection exposes the eye to the small but serious risk of infective endophthalmitis. Retrospective reports indicate a per-injection endophthalmitis risk between 0 and 0.87% for IVTA injection and 0.019% to 0.16% for IVB injection[44-47]. Neither severe complications such as infectious endophthalmitis/retinal detachment nor IOP elevation were observed in the present study. There was no significant change in mean IOP compared with baseline at any of the study follow-up visits in either group in our study. Our results of IOP may be explained by the use of a lower dose of TA. When compared to DRCR, net protocol, in which cataract formation was 23% prior to the 2y visit, we didn’t meet with any significant cataracts after single dose injection[48].
The present study has some limitations because of the retrospective nature of the work, limited patient number. There may be an interaction of bevacizumab and triamcinolone agents in combination group.
In conclusion, our results suggest that injection of combined IVTA-IVB seems to have better results than IVB alone. We decided that the use of a lower dose of TA combined with bevacizumab resulted in almost no IOP and cataract-like complications. Among patients who did not have any health insurance and could not effort repeated therapies and novel drugs, receiving a single combined treatment may still be beneficial up to 3mo-6mo. Additional prospective and larger studies are needed to further investigate optimal interventions.