Serotonin transporter and cholecystokinin in diarrhea-predominant irritable bowel syndrome:Associations with abdominal pain,visceral hypersensitivity and psychological performance
Geng Qin, Yu Zhang, Shu-Kun Yao
Geng Qin, Yu Zhang, Graduate School, Peking Union Medical College and Chinese Academy of Medical Sciences, Beijing 100730, China
Geng Qin, Shu-Kun Yao, Department of Gastroenterology, China-Japan Friendship Hospital,Beijing 100029, China
Abstract
Key words: Irritable bowel syndrome;Abdominal pain;Visceral hypersensitivity;Psychological performance;Serotonin transporter;Cholecystokinin
INTRODUCTION
Irritable bowel syndrome (IBS) is the most common gastrointestinal condition[1]and mainly manifests as bloating, chronic or recurrent abdominal pain and a change in frequency or appearance of stool[2,3].The prevalence of IBS varies from 1.1% to 45.0%among studies in different countries, and a meta-analysis showed that the pooled worldwide prevalence was 11.2%[4].It is a multifaceted abnormality in neurogastroenterology and regulation of the gut-brain axis[5,6].
The newest diagnostic criterion is Rome IV, which was promulgated in 2016[7].It defines IBS as recurrent abdominal pain on average at least 1 d/wk in the last 3 mo,associated with two or more of the following criteria:(1) Related to defecation;(2)Associated with a change in frequency of stool;and (3) Associated with a change in form (appearance) of stool.IBS was divided into four subtypes based on the predominant stool form,i.e., constipation-predominant IBS (IBS-C), diarrheapredominant (IBS-D), mixed stool pattern (IBS-M) and (IBS-U)[4], of which IBS-D refers to > 25% of bowel movements with Bristol stool types 6 or 7 and < 25% of bowel movements with Bristol stool types 1 or 2.
Studies focused on IBS and related health problems have been extensively reported.There was no consistency in the etiology and pathogenesis of IBS, and the various factors involved, such as gastrointestinal dysmotility, visceral hypersensitivity,changes in gut barrier function, intestinal microbial dysbiosis, and brain-gut axis dysfunction[8-10].Depression and anxiety are two of the possible reasons for functional gastrointestinal disorders[11].A meta-analysis found that patients with IBS had more severe and frequent depressive symptoms than healthy controls[12], which suggests that there were interactions between IBS and psychological factors.
Enterochromaffin cells (ECs) were the first endocrine cells of the gastrointestinal tract to be chemically distinguished[13].Previous animal studies have shown that 5-hydroxytryptamine (5-HT) and cholecystokinin (CCK) co-expressing EC cells can be seen in the small intestine and large intestine[14,15].Previous studies have found that 5-HT can inhibit gastric emptying, trigger and enhance the propulsion of the small and large intestine, promote secretion, aggravate intestinal inflammation and regulate appetite[13,16,17].The function of the serotonin transporter (SERT) is to rapidly re-uptake 5-HT in the effective site, and to regulate the action time and intensity of 5-HT.5-HT is also found in the limbic system.The study found that patients with lower SERT expression were more likely to have negative emotions (such as somatization, anxiety,depression).CCK can contract smooth muscle in the gallbladder and gastrointestinal tract, and stimulate gland secretion in the pancreas, liver, small intestine and other organs.A previous study showed that exogenous CCK injection did not affect rectal movement or sensation.However, it can increase abdominal pain in IBS patients during rapid intermittent expansion[18].It has been found that CCK-8 peptide can enhance colonic motility and induce abdominal pain in IBS patients, but the mechanism is unclear.
Previous studies reported that mucosal 5-HT, SERT immunoreactivity and SERT messenger RNA (SERT-mRNA) were all significantly reduced in IBS-C and IBS-D patients[19,20].
This study focused on the pathogenesis of IBS-D from the aspects of abnormal regulation of the gut-brain axis and mental disorders.We aimed to compare IBS-D patients, who met the diagnostic criteria of Rome IV, to healthy controls with regard to clinical characteristics, SERT and CCK levels in plasma and mucous membrane and then to examine the correlations between SERT, CCK and abdominal pain, visceral hypersensitivity and psychological performance.
MATERIALS AND METHODS
Study population
A total of 40 IBS-D patients, who were treated at the Department of Gastroenterology of the China-Japan Friendship Hospital from September 2017 to April 2018, and 18 age- and sex-matched healthy controls were recruited for the study.All IBS-D patients were diagnosed based on the Rome IV criteria.Healthy controls consisted of patient spouses, medical examiners and volunteers.The patients and healthy controls were included if they did not take the following drugs within 2 wk of the study:Antispasmodics, analgesics, microecological preparations, antidepressants, antiinflammatory drugs, antibiotics, other drugs and antacids that can affect gastrointestinal motility.The exclusion criteria were as follows:(1) Gastrointestinal organic diseases, endocrine system diseases, metabolic diseases, connective tissue diseases and other organ diseases;(2) A history of gastrointestinal or abdominal surgery;and (3) A previous or current diagnosis of mental illness.
All subjects were informed of the study details and provided written informed consent.This study was conducted in accordance with the Declaration of Helsinki and approved by the Ethics Committee of China-Japan Friendship Hospital.
Study procedures
Clinical symptoms and psychosocial assessment:The severity of clinical symptoms was evaluated using the IBS symptom severity scale[3], the VAS pain scale and the frequency course scale.The visceral sensitivity index was used to evaluate visceral sensitivity and gastrointestinal-specific anxiety.Psychiatric symptoms were assessed using the validated Hospital Anxiety and Depression Scale[21].The IBS-specific quality of life was used to evaluate the quality of life of IBS patients in this disease state.
Visceral sensitivity test:The visceral sensitivity test was performed in the Gastroenterology Kinetic Laboratory by the same investigator.Before the examination, the subjects were given glycerin to eliminate feces.The subjects were placed in the left lateral decubitus position and were asked to relax.After the mass was eliminated by digital rectal examination, the lubricating pressure measuring catheter was slowly inserted into the rectum, with an insertion depth of 15 cm and a balloon placed above the anal margin of 8 cm.After the subject had adapted for 3 min,the examination began.Air was slowly injected (at a rate of 10 mL/5 s) into the balloon by a 100 mL syringe.The subject's feeling after every 10 mL gas injected was recorded.When the subject felt the initial swelling, continuous defecation sensation,pain discomfort or intolerance, the amount of gas injected (in mL) was recorded,which reflected the initial feeling threshold, continuous defecation threshold and maximum tolerance threshold, respectively.
Specimen collection:Participants were not allowed to take gastrointestinal motility drugs, laxatives, antidiarrheal drugs, microecological agents, antidepressants or other drugs that affect gastrointestinal motility one week prior to the examination.The participants underwent colonoscopy after standard bowel preparation with polyethylene glycol electrolyte powder (Fortrans, BEAUFOUR IPSEN Industrie,Dreux, France), and four mucosal pinch biopsies were taken from the rectosigmoid junction.Two specimens were immediately fixed in 10% formalin for at least 72 h,embedded in paraffin and sectioned (4 μm) for routine hematoxylin and eosin staining and immunohistochemistry.The other specimens were immediately immersed in storage reagent (RNA-Be-Locker A;Sangon, Shanghai, China) and stored at -80 °C for quantitative real-time polymerase chain reaction (qRT-PCR) analysis.Venous blood was centrifuged at 2000 r/min for 10 min within 30 min after collection,and the supernatant was taken for analysis.
Histology and immunohistochemistry:Paraffin sections were stained with hematoxylin eosin and processed for immunohistochemistry.The latter section was incubated with primary antibody (rabbit polyclonal anti-SERT antibody, 1:400,Affinity Biosciences, United States;rat monoclonal anti-serotonin antibody, 1:100,Santa, United States;rabbit polyclonal anti-CCK antibody, 1:100, Abcam, United Kingdom) overnight at 4 °C after dewaxing, antigen retrieval, endogenous peroxidase inhibition, and nonspecific antigen blocking.After washing with phosphate buffered saline, the sections were incubated with anti-rat and anti-rabbit secondary antibodies(1/200, Zhongshan Golden Bridge, Beijing, China) combined with horseradish peroxidase at room temperature for 1 h and then visualized using diaminobenzidine.Finally, the sections were counterstained with hematoxylin and observed under a light microscope to examine the average optical density (OD value) of positive expression of the stain.
Quantitative real-time PCR detection:The expression of CCK and SERT was analyzed by real-time quantitative PCR.Total RNA in the tissue was extracted by TRIzol Reagent (Invitrogen Life Technologies, Waltham, MA, United States) and reverse transcribed into cDNA.Real-time quantitative PCR was then carried out in a StepOnePlus Real-Time PCR system (Applied Biosystems, Waltham, MA, United States) using the FastStart Universal SYBR Green Master Rox Kit (Roche, Shanghai,China).Finally, the mRNA of glyceraldehyde-3-phosphate dehydrogenase (GAPDH)was used as an internal reference.The primers were designed and synthesized by Beijing Aoke Biotechnology Co., Ltd.The upstream region of SERT was 5'-CAGCGTGTGAAGATGGAGAAG-3', and the downstream region of SERT was 5'-TGGGATAGAGTGCCGTGTGT-3'.The upstream region of CCK was 5'-CAGAGGAGGCAGAATAAGAA-3', and the downstream region of CCK was 5'-CAGGAGTCACAGATGAAGAA-3'.The upstream housekeeping gene GAPDH(internal reference) was 5'-GGAAGCTTGTCATCAATGGAAATC-3', and the downstream housekeeping gene GAPDH was 5'-TGATGACCCTTTTGGCTCCC-3'.
The above were used for quantitative real-time PCR.The total reaction volume was 10 μL, including 5 μL of SYBR master mix (Bio-Rad, United States), 0.2 μL of upstream and downstream primers, 1 μL of template cDNA and 3.6 μL of ddH2O.The reaction conditions consisted of 5 min at 95 °C, 10 s at 94 °C, 10 s at 59 °C, 10 s at 72 °C for 40 cycles, and the temperature change rate was 20 °C/s, followed by 10 s at 95 °C, 15 s at 65 °C and then increased to 95 °C/10 s at a rate of 0.1 °C/s.
The fluorescence signal was continuously monitored for dissolution curve analysis,and GAPDH was used as an internal reference for relative quantitative analysis.The 2-ΔCt method was used to determine the expression level of the SERT gene relative to the internal reference (ΔCt = Ct target gene - Ct internal reference).
Plasma SERT and CCK levels:The levels of SERT and CCK in plasma were determined by double antibody sandwich ELISA (SERT/CCK kit).
Statistical analyses
Data were analyzed using SPSS version 24.0 (SPSS Inc, Chicago, IL, United States),and the significance level was set atP< 0.05 (two-tailed).The Shapiro-Wilk test was used to test the normal distribution of continuous variables.Comparisons between IBS patients and healthy controls regarding sociodemographic and clinical characteristics were examined using the independent samplet-test, Mann-WhitneyUtest, andχ2test as appropriate.The correlations between continuous variables were examined using Pearson correlation analyses if normally distributed;otherwise,Spearman correlation analyses were conducted.
RESULTS
Basic characteristics
The 40 IBS-D patients had a mean age of 44.50 ± 9.27 years, and 75% (n= 30) of these patients were male.The mean age of the 18 healthy controls was 42.33 ± 12.81 years,and 72.2% (n= 13) were male.The comparisons between IBS-D patients and healthy controls with regard to clinical characteristics are shown in Table 1.There were significant differences in the visceral sensitivity index (75.78 ± 9.31vs53.39 ± 4.49,P<0.001), initial sensation threshold (31.00 ± 8.41 mLvs52.22 ± 8.09 mL,P< 0.001),defecating sensation threshold (51.75 ± 13.57 mLvs89.44 ± 8.73 mL,P< 0.001) and maximum tolerable threshold (97.25 ± 23.64 mLvs171.11 ± 20.83 mL,P< 0.001)between patients and healthy controls.Anxiety (7.78 ± 2.62vs2.89 ± 1.02,P< 0.001)and depressive (6.38 ± 2.43vs2.06 ± 0.73,P< 0.001) symptoms were also significantly different between IBS-D patients and healthy controls.
The levels of CCK and SERT in the mucosal membrane and plasma
The levels of SERT and CCK in plasma were determined by ELISA.CCK and SERTmRNA expression in colonic mucosa was quantified by qRT-PCR.Immunohistochemistry showed that the cytoplasm of cholecystokinin immunoreactive (CCK-IR)cells contained brown granules with a clear background (Figure 1).SERT-positive products were brownish yellow and observed on the membrane (Figure 1).The levels of CCK in the mucosal membrane and plasma were significantly higher in IBS-D patients than in healthy controls, and SERT showed the opposite trend (Table 2).
Correlations between CCK, SERT and other parameters
Spearman correlations between key continuous variables in IBS-D patients are shown in Table 3, Table 4 and Table 5.In IBS-D patients, CCK expression was positively correlated with the severity of abdominal pain.Furthermore, the level of SERT was negatively correlated with the severity of abdominal pain and visceral sensitivity(Table 3, Table 4 and Table 5).
DISCUSSION
In this case-control study, we aimed to evaluate psychological and clinical characteristics and visceral sensitivity in IBS-D patients and determine the roles of SERT and CCK in IBS-D patients.
Depressive and anxiety symptoms were more likely to be experienced by IBS-D patients compared to healthy controls, which agreed with previous studies[22].Mental disorders, such as depression, anxiety and sleep disorders, are commonly reported in gastrointestinal disorders[23,24].For example, one cohort study showed that anxiety increased the hazard for postinfectious IBS, and the study also indicated that the mechanism was partly due to the enhancement of susceptibility to develop infectious gastroenteritis[25].Several studies have demonstrated the effectiveness of psychological treatments on lessening and relieving bowel symptoms in IBS patients, such as cognitive behavioral therapy, mindfulness-based therapies and hypnosis[26-29].Therefore, psychotherapy should be simultaneously included in clinically IBS-specific treatment to improve IBS patients’ conditions in a timely manner.
Higher visceral sensitivity index, lower initial sensation threshold, lower defecating sensation threshold and lower maximum tolerable threshold were found in IBS-D patients compared with healthy controls.There have been inconsistent reports on the association between visceral sensitivity and functional gastrointestinal (GI)disorders[30].Some previous studies showed that there were no relationships between hypersensitivity and GI disorder symptoms[31,32], which likely explain our results.In contrast, a large number of studies have identified that IBS patients have higher visceral sensitivity than controls[33]and visceral hypersensitivity is associated with the severity of GI symptoms[30].The existing discrepancies could be partly due to the various patient-related or research-related factors, such as selection bias in patients or healthy controls and different assessment tools[30].
Mucosa and plasma CCK were significantly higher in IBS patients than in controls.Abdominal pain was reported as a dominant symptom in IBS patients[30], and we identified positive correlations between pain rulers, pain symptoms, pain frequency and mucosa and plasma CCK.Simultaneously, we observed that mucosa and plasma SERT were significantly lower in the IBS-D patients.There were negative correlations between abdominal pain and mucosa and plasma SERT.Negative correlations between psychological performance and mucosa and plasma SERT were also observed.
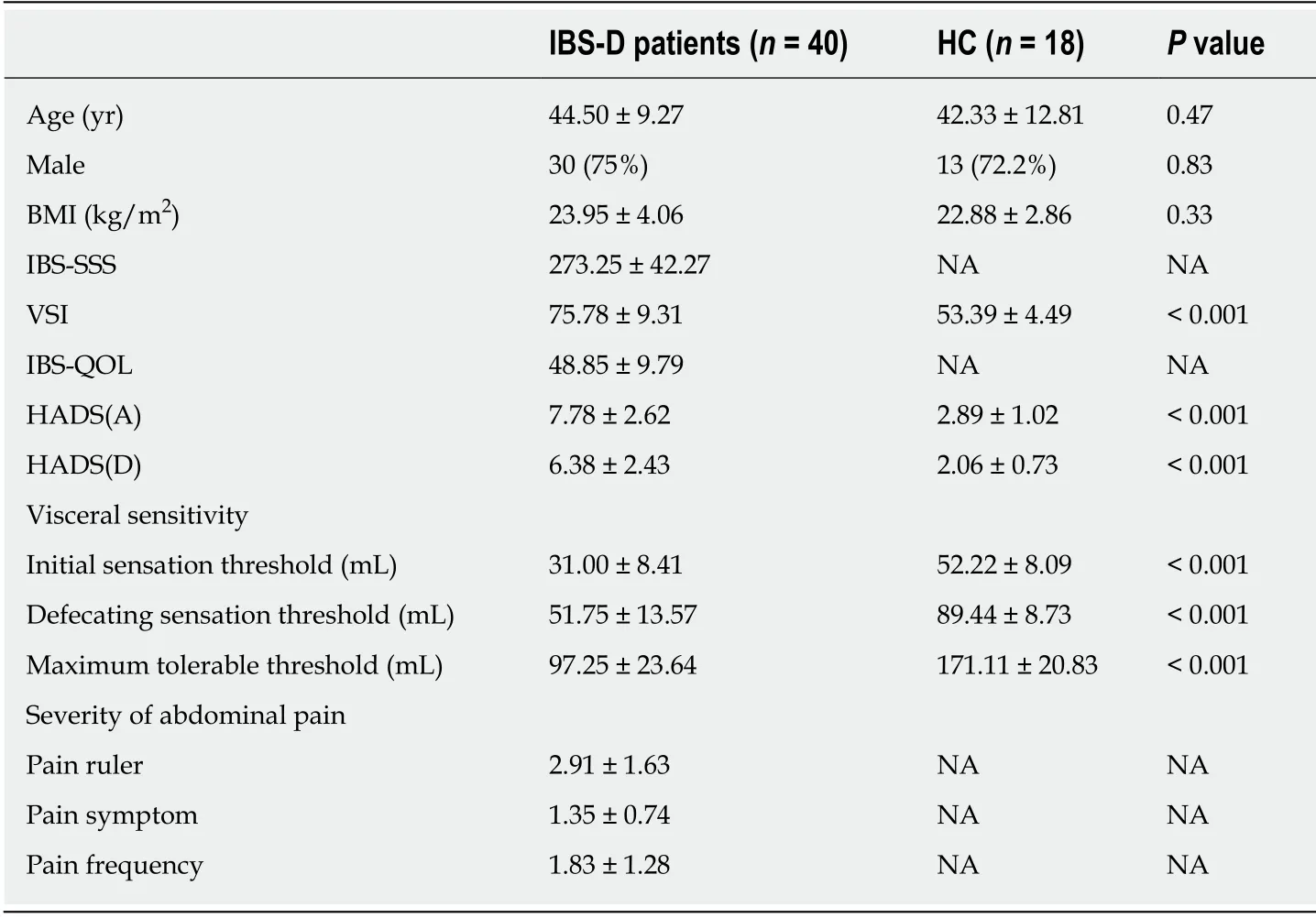
Table 1 Sociodemographic and clinical characteristics in irritable bowel syndrome patients and healthy controls
This study compared the clinical characteristics and biomarker levels between IBSD patients and healthy controls and the correlation between patients’ GI severity level and biomarker levels.There are some limitations in our study.First, only IBS-D patients were included, and the selection bias could limit the generalization to other types of IBS patients.Second, only patients from one hospital were recruited.Third,the sample size was small.In addition, the disadvantages of a cross-sectional study design lead to the impossibility of identifying causality.
In conclusion, IBS patients had poorer mental health status and visceral hypersensitivity than healthy controls but higher mucous membrane CCK and lower SERT levels.Psychotherapy should be simultaneously included in clinically IBSspecific treatment to improve IBS patients’ conditions in a timely manner, and further large-scale perspective studies are needed to explore the correlation between patients’GI severity level and biomarker levels.
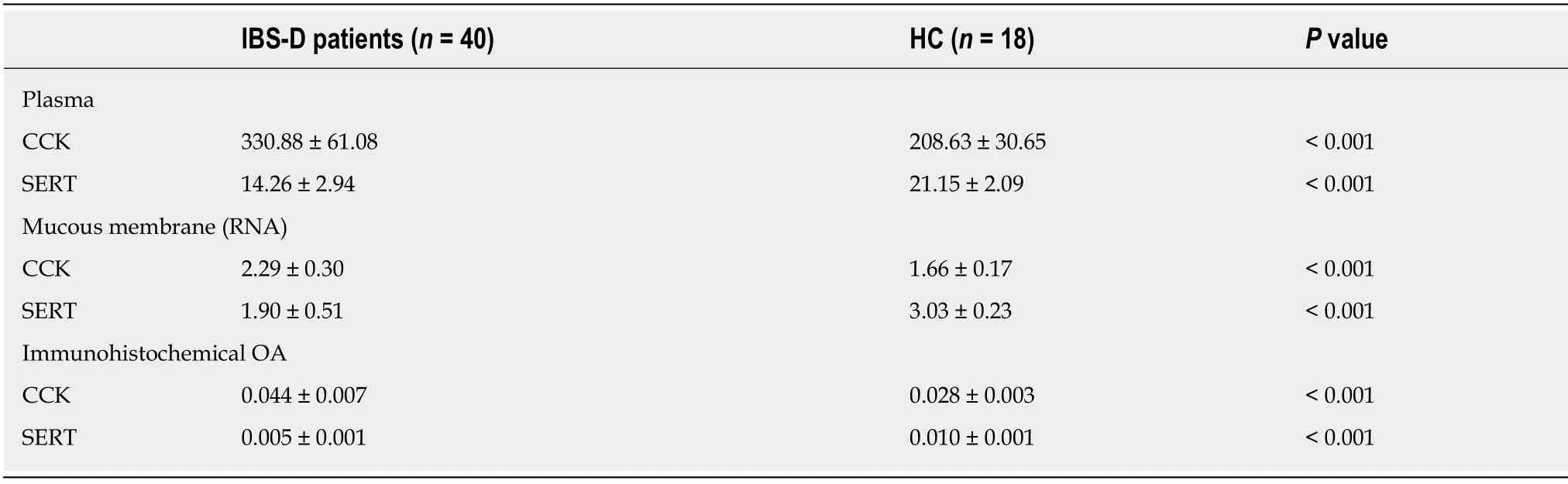
Table 2 The level of cholecystokinin and serotonin transporter in mucosa membrane and plasma
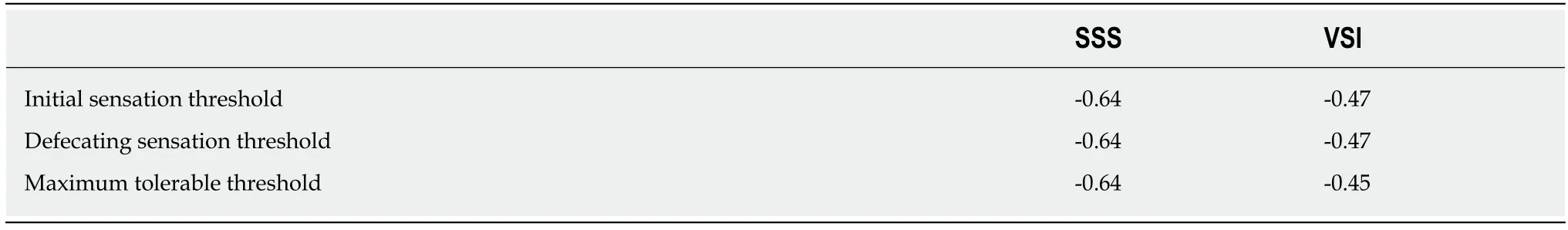
Table 3 The correlations between visceral sensitivity and symptom severity scale, and visceral sensitivity index in diarrhea-predominant irritable bowel syndrome patients

Table 4 The correlations between abdominal pain and the level of cholecystokinin in mucosa membrane and plasma
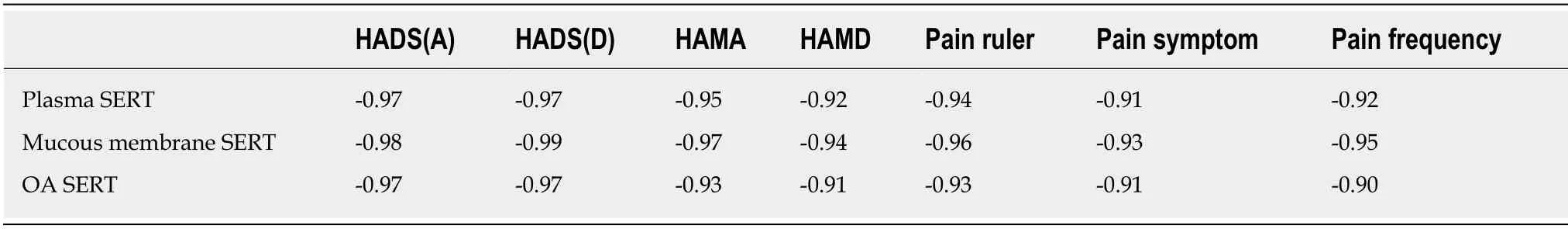
Table 5 The correlations between abdominal pain, psychological performance and the level of serotonin transporter in mucosa membrane and plasma

Figure 1 Mucosal histology and immunohistochemistry in patients with diarrhea-predominant irritable bowel syndrome.
ARTICLE HIGHLIGHTS
Research background
Diarrhea-predominant irritable bowel syndrome (IBS-D) patients have psychosomatic disorders and visceral hypersensitivity.Preclinical studies have shown that the expression of serotonin transporter (SERT) in the gut can affect the mental and psychological symptoms of IBS patients.Patients with lower expression of SERT are more likely to have negative emotions (somatization,anxiety, depression, hostility).An injection of cholecystokinin (CCK) can enhance and induce colonic motility, resulting in abdominal pain.Few studies have reported the relationship between mucous SERT, CCK levels and symptom severity, anxiety, depression and visceral hypersensitivity in patients.It has been suggested that SERT and CCK may be involved in the pathogenesis of IBS-D.
Research motivation
The present research includes three aspects:(1) General demographic characteristics, symptoms,psychological factors and visceral sensitivity;(2) The expression of SERT and CCK in colonic mucosa of IBS-D patients;and (3) Correlations between CCK, SERT and other parameters.Similar to preclinical studies in IBS-D patients, SERT and CCK may be involved in the pathogenesis of IBS-D, which provides a new potential method for identifying a more specific and effective therapeutic target.
Research objectives
The purpose of this study was to determine the expression of SERT and CCK in colonic mucosa of IBS-D patients, and analyze the relationship between SERT, CCK and general demographic characteristics, symptoms, psychological factors and visceral hypersensitivity.
Research methods
The participants were evaluated by questionnaires (IBS symptom severity scale, visceral sensitivity index, hospital anxiety and Depression Scale) to obtain clinical and psychological characteristics, and underwent colonoscopy and mucosal biopsies.Visceral sensitivity was detected by a high-resolution manometric system, and the expression of SERT and CCK were detected by immunohistochemistry.Mucosal SERT and CCK mRNA levels were measured by real-time quantitative PCR.These parameters were statistically analyzed using SPSS version 24.0.
Research results
The results showed that the anxiety and depression symptoms and visceral sensitivity in IBS-D patients were significantly increased.The levels of CCK in the mucosal membrane and plasma were significantly higher in IBS-D patients than in healthy controls, and SERT showed the opposite trend.The expression of CCK was positively correlated with the severity of abdominal pain, and the level of SERT was negatively correlated with the severity of abdominal pain and visceral sensitivity.
Research conclusions
IBS-D patients had psychosomatic disorders and visceral hypersensitivity.SERT and CCK might be involved in the pathogenesis of IBS-D by regulating the brain-gut axis and affecting visceral sensitivity.This provides a new potential method for identifying a more specific and effective therapeutic target.
Research perspectives
Our study determined the role of SERT and CCK in the pathogenesis of IBS-D.There are some limitations in our study.First, only IBS-D patients were included, and selection bias could limit the generalization to other types of IBS patients.Second, only patients from one hospital were recruited.Third, the sample size was small.According to the existing research results, no causal inferences can be made.Therefore, more carefully designed clinical studies are needed.
ACKNOWLEDGEMENTS
We thank Dr.Du S and Dr.Zhang M for enrollment of participants, and Dr.Gao C,Dr.Liu J and Dr.Liu F for assistance with the colonoscopy tests.
 World Journal of Clinical Cases2020年9期
World Journal of Clinical Cases2020年9期
- World Journal of Clinical Cases的其它文章
- Nutrition management in acute pancreatitis:Clinical practice consideration
- Bone disease in chronic pancreatitis
- Role of microRNAs in the predisposition to gastrointestinal malignancies
- Recurrent anal fistulas:When, why, and how to manage?
- Removal of biofilm is essential for long-term ventilation tube retention
- Neutrophil gelatinase-associated lipocalin does not predict acute kidney injury in heart failure
