Factors affecting outcomes of surgically treated patients with cranial extradural hematoma: A cross-sectional study
Ghazwan A. Lafta, Ali A. Dolachee, Alyaa K. Al-ZubaidiDepartment of Surgery, Faculty of Medicine, University of Al-Ameed, Iraq
2Department of Surgery, College of Medicine, University of Al-Qadisiyah, Iraq
3Ministry of Health, Baghdad, Iraq
ABSTRACT
KEYWORDS: Extradural hematoma; Glasgow coma scale; Head injury; Outcome
1. Introduction
Extradural hematoma (EDH), a blood accumulation between the dura matter and the skull’s inner table, is an infrequent sequela of head injury. It occurs in less than 2% of the patients admitted with craniocerebral trauma and in up to 15% of fatal head injuries. In 85%-95% of the patients, EDH is associated with an overlying skull fracture. Blood vessels closed to the fracture are the usual sources of the bleeding forming EDH[1,2].
When the hematoma is deeper than 1 cm or larger than 25 mL, EDH is usually clinically significant. It is reported that the hemorrhage volume is at least 100 mL in death cases[3,4,5].
Associated intracranial lesions such as subdural hematoma, intracerebral hematoma, and cerebral contusion result in an increased mortality rate[6,7]. Other factors affecting the outcomes and prognosis include increased age, poor neurological condition according to the Glasgow coma scale (GCS), large hematoma volume, delay in an operative evacuation, large midline shift, and postoperative elevation in intracranial pressure[8,9]. Glasgow outcome scale (GOS) is widely accepted as a standard method to assess the outcomes of the patients with head trauma[10]. Our study aims to evaluate the risk factors of poor outcomes of EDH patients in the middle and south of Iraq.
2. Materials and methods
2.1. Ethical approval
This study was approved by the local Ethical Committee in the Neurosurgery Department of the Neurosurgery Teaching Hospital in Baghdad (291 on 30/1/2018).
2.2. Subjects
It was a cross-sectional study conducted at the Neurosurgery Teaching Hospital in Baghdad and was carried prospectively from February 1st, 2015 to May 1st, 2017.
One hundred patients with head injury and surgically treated EDH had been selected and included in this study after taking oral and written consent. They were transferred from the middle and south of Iraq, and categorized according to the age, gender, occupation, initial GCS, the chief complaint at presentation, the consciousness throughout the course of the hematoma, physical signs at presentation, type of injury, the time interval between injury and reception, the time between reception and surgery, site (frontal, parietal, etc.), thickness, side of hematoma, radiological finding apart from EDH, surgical procedure, associated injuries, intraoperative findings, source of bleeding, and outcomes.
All the patients had been received at the emergency department where they were fully evaluated. Then, GCS was adopted for an initial assessment in all of the patients. This scale can measure the severity of the injury, and patients with GCS from 13-15 are considered with mild injury, 9-12 with moderate injury, and 3-8 with severe injury[5]. The patients with GCS less than 8 were transferred to the ICU for specific resuscitation. A full history was taken either from the patients or from their relatives in cases of loss of consciousness or the presence of amnesia. A full neurological examination was performed for each patient. Brain CT scans were done as the radiological investigation of choice for all of the patients. Definitive management was done for all patients including craniotomy and craniectomy.
The follow-up was done at 1st month, 3rd months, 6th months after discharge through regular visits.
2.3. Statistical analysis
Statistical analysis was performed by SPSS version 17. Categorical data were expressed as percentage. Chi-square was used to analyze categorical data. Regression models were used to determine which variable independently affects functional recovery, disability, and mortality. The significant level of the test was expressed at α=0.05.
3. Results
A total of 100 cases of EDH (80% males and 20% females) were included in this study, among which 19% cases were ≤9 years old, 54% cases between 10-29 years old, 25% cases between 30-59 years old, and 2% patients >60. The causes of injury were different, with fall from height accounting for 51%, road traffic accidents for 37%, and assault injuries for 12%. A total of 46% of patients had the time interval between injury and reception less than 3 h, while 54% had more than 3 h. The patients arrived at the emergency room with different conscious conditions, of whom 19% had GCS of 3-8, and 43% had GCS of 9-12, while 38% had GCS of 13-15. Altogether, 26% of the patients complained of headache and vomiting, and 9% had convulsions. On examination, there were 23 patients had ear bleeding, 20 with scalp wounds, 15 with subgaleal hematoma, and 15 with epistaxis. There were 3 hemiplegic patients, 13 cases of hemiparesis, 8 cases of facial palsy, and 6 cases with olfactory nerve palsy. In addition, 30 patients were with unilateral pupil dilation and 9 patients with bilateral dilation. CT scan was done for all patients, and the results showed that 87% of the patients had a hematoma in the thickness of 1-3 cm, while 11% had 3.5-5.0 cm in thickness. In addition, only 2% of the patients showed a hematoma more than 5 cm in thickness. There were associated intracranial lesions in some patients, as 5 of them had an acute subdural hematoma, and 3 of them had an intracerebral hemorrhage, while 2 of them with brain stem contusion. Surgery was done for all patients, and follow-up was carried out at 1 month, 3 months, 6 months after discharge through regular visits. There were 78% of the patients with good functional recovery, 10% with residual disability, and 12 % were dead.
GCS scores had affected the outcomes (P=0.01) (Table 1). When GCS (3-8) changed to (13-15), the coefficient factor (B) was 6.18 (P=0.001) i.e. functional recovery improved by six times when GCS scores increased especially equally or higher than 13, which had no effect on the disability of the patients, but inversely related to the death (P=0.005) (Table 2). The time interval between injury and reception also had an effect on the outcomes (P=0.02), as patients with a shorter time interval showed better functional recovery (≤3 h) (P=0.001), while the longer time interval (>3 h) increased the residual disability (P=0.005), but the time interval had no effect on the death (Table 1).
4. Discussion
Our study showed that 78% of patients had a good functional recovery, 10% had residual disability, and 12% were dead, which is similar to the study of Kiboi et al.[11].
Age between 10 and 29 years old (54%) was one of the risk factors of EDH in our study. Similarly, Chowdhury et al. found that 57.07% of the patients were between 11 and 30 years old[12]. The reason may be this age group has more daily activities than the others (especially school-age). Regarding gender, 80% of the patients were males, and 20% were females. The high incidence of EDH in males is attributed to their activities. Males are more prone to trauma as they are more mobile and travel more for their day-to-day activities than females. Islam et al. also found that 92.2% of the patients were males and 7.8% were females[13], and Chowdhury et al. showed that 86.32 % of the patients were males and 13.78 % were females in their studies concerning EDH[12].
Depth of hematoma was considered as a risk factor for poor outcomes. Hematoma thickness higher than 5 cm is fatal. With the expansion of the space-occupying lesion, uncal herniation and brain stem injury will be unavoidable and consequently lead to death. This perspective was consistent with that of Rehman et al. and Satapathy et al.[14,15].

Table 1. Patients' demographic and baseline characteristics.
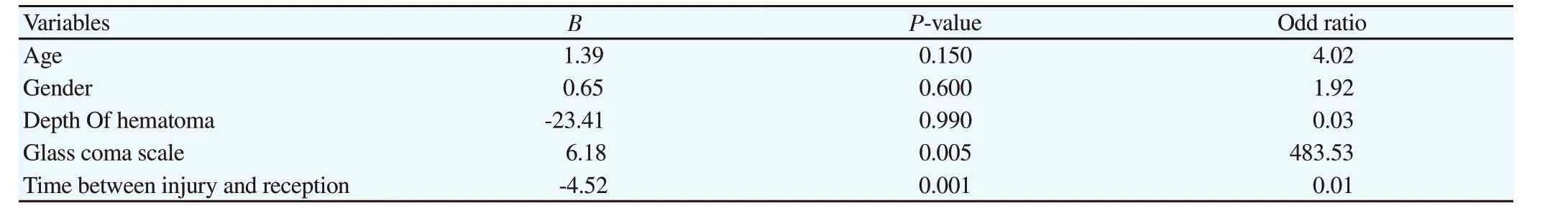
Table 2. Effect of each studied variable on the outcomes (functional recovery, residual disability, and death) after adjustment of other independent variables.
GCS is efficient in predicting the outcomes of EDH. In the present study, functional recovery increased six times with higher GCS, and inversely related to the mortality, but had no effect on the disability of the patients. This was attributed to the fact that GCS is an important prognostic factor to reflect the brain condition, hence it can be used to predict the probability of survival or death[16].
The study of Islam et al. showed that 73.5% of their patients had initial GCS of 9-15, while 26.5% had GCS of 3-8[13]. The study of Rehman et al. showed that 54% of the patients were presented with CGS of 13-15, 26% of 9-12, 20% of 3-8. This study compared the GCS with the corresponding outcomes depending on the GOS, and they founded that GCS of 3-8 was associated with unfavorable outcomes while patients with GCS of 13-15 and 9-12 associated with favorable outcomes[12]. Haltmeier et al. mentioned that there was a strong correlation of the outcomes of EDH with GCS. In conclusion, higher GCS scores indicate better outcomes, while lower scores imply worse outcomes[17].
The time interval between injury and reception also showed a great significance for EDH outcomes. Better functional recovery was found among patients with a shorter time interval (≤3 h) (P=0.001), while the longer time interval (>3 h) increased the residual disability, but the time interval had no effect on the mortality. The reason is that the shortest time can maintain the viability of brain tissue and lower the degree of brain injury, and vice versa.
Korinth et al. mentioned that delayed EDH treatment would result in a poor outcome[18]. Royal College of Surgeons of England recommended that surgical decompression should be carried out within 4 h after the onset of significant symptoms to get good recovery[19]. We recommend an establishment of more neurosurgery centers especially in Baghdad and at least one center in each other governorate in order to provide optimum neurosurgical care and adequate management at the initial time of injury. A proper schedule and plan of management should be well informed to the residents in emergency departments of the general hospitals and general practitioners in rural areas. For head-injured patients, a special neurological examination record form can be used for such purposes. Hard efforts should be made to shorten the time between injury and receiving the patient, as well as reaching the victims in high ways should be as quick as possible. Resuscitation and life-saving measures must be provided to the patients at the accident location and should be reviewed at the first receiving healthcare center and continue until reaching the neurosurgical center, to ensure adequate hemodynamic state to minimize the possibilities of secondary brain injuries. Safety measures should be applied during driving motorcycles including wearing helmets, to minimize head injury due to road traffic accidents as much as possible. More attention should be given to the children and closely watching their activities and decorating the houses with the safety walls around the roves and along the stairs.
5. Conclusion
Age between 10 and 29 years, male gender and depth of hematoma more than 5 cm are at increased risk of poor outcomes in patients with surgically treated EDH. GCS on admission and time between injury and reception are important factors influencing the outcomes.
Conflict of interest statement
The authors report no conflict of interest.
Authors’ contribution
G.A.L.: Corresponding author, study designer, and writing the manuscript; A.A.D.: Data collector, interpreter, and writing the introduction; A.K.A: Data analysis, writing the results.
 Journal of Acute Disease2020年3期
Journal of Acute Disease2020年3期
- Journal of Acute Disease的其它文章
- Knowledge, attitude, and practice towards coronavirus disease 2019 (COVID-19) among medical students: A cross-sectional study
- Clinical characteristics and treatment of acute epiglottitis: A retrospective study of 28 cases
- Aberration detection of pertussis from the Mazandaran province, Iran, from 2012 to 2018: Application of discrete wavelet transform
- Identification of Panton-Valentine leukocidin virulence gene in methicillinresistant Staphylococcus aureus isolated from clinical specimens of burn patients in Zare Hospitals of Sari, Iran
- Successful treatment of hepatic hydrothorax: A case report
- Suicide attempt of an overt hypothyroid patient with levothyroxine: A case report
