肺移植患者术后急性肾损伤影响因素分析
杜雯雯 王晓星 陈文倩 张丹 刘慧芳 张相林 李朋梅

摘 要 目的:分析肺移植患者術后急性肾损伤(AKI)的发生情况及可能的影响因素。方法:回顾性收集2017年4月-2018年6月于我院接受肺移植术64例患者的病历资料,按术后是否发生AKI分为AKI组(44例)和无AKI组(20例)。根据我院肺移植诊疗规范,所有患者均给予注射用甲泼尼龙琥珀酸钠或注射用甲泼尼龙琥珀酸钠联合注射用巴利昔单抗诱导治疗,并于术后行他克莫司胶囊+吗替麦考酚酯分散片或吗替麦考酚酯胶囊或麦考酚钠肠溶片+甲泼尼龙片或醋酸泼尼松片三联免疫抑制治疗方案。记录AKI组患者术后1周内AKI发生情况,并观察两组患者术中[手术类型、手术时间、体外膜肺氧合(ECMO)支持、免疫抑制剂使用情况、术中出血量]、术后影响因素[重症加强护理病房(ICU)天数、机械通气天数、ECMO支持天数、术后1周内血清肌酐(Scr)中位值,他克莫司全血浓度中位值、潜在肾毒性药物使用种类(≥4种)、住院天数]及术后1年生存率。结果:肺移植术后1周内,64例患者有中44例(68.8%)至少发生过1次AKI,其中1期19例(29.7%)、2期17例(26.5%)、3期8例(12.5%);术后第4天AKI发生率最高(57.4%);在肺移植术后1周内3期AKI发生率总体呈上升趋势,并在术后第5天达到最高(8.7%)。无AKI组患者的手术时间、术后1周内Scr中位值、他克莫司全血浓度中位值均显著短于或低于AKI组(P<0.05);两组患者手术类型、ECMO支持使用情况、免疫抑制剂使用情况、术中失血量、ICU天数、机械通气天数、ECMO支持天数、潜在肾毒性药物(≥4种)使用率、住院天数比较,差异均无统计学意义(P>0.05)。1期和2期AKI患者术后1年生存率与无AKI组比较,差异均无统计学意义(P>0.05);3期AKI患者术后1年生存率显著低于无AKI组(P<0.05)。结论:肺移植术后AKI的发生率较高。手术时间、术后1周内Scr中位值、他克莫司全血浓度中位值均为术后发生AKI的可能影响因素。
关键词 急性肾损伤;肺移植;术后;影响因素
中图分类号 R563 文献标志码 A 文章编号 1001-0408(2020)18-2247-06
DOI 10.6039/j.issn.1001-0408.2020.18.13
ABSTRACT OBJECTIVE: To analyze the occurrence of acute kidney injury (AKI) after lung transplantation and its possible influential factors. METHODS: Medical records of 64 patients who received lung transplantation in our hospital from April 2017 to June 2018 were included in this retrospective study. Patients were divided into AKI group (44 cases) and non-AKI group (20 cases), according to whether AKI occurred after operation. According to diagnostic criteria for lung transplantation in our hospital, all patients were given Methylprednisolone sodium succinate for injection or Methylprednisolone sodium succinate for injection combined with Basiliximab for injection, and triple immunosuppressive therapy of Tacrolimus capsules+Mycophenolate mofetil dispersible tablets or Mycophenolate mofetil capsules or Mycophenolate sodium enteric-coated tablets+Methylprednisolone tablets or Prednisone acetate tablets were given after operation. The occurrence of AKI in AKI group within a week after operation were recorded. Intraoperative influential factors (operation type, operation duration, ECMO support, immune inhibitor use, intraoperative blood loss), postoperative influential factors [days of ICU, mechanical ventilation and ECMO support, median value of Scr within one week after operation, median tacrolimus concentration and the use of potential nephrotoxic drugs (≥4 kinds), hospitalization days] and survival rate one year after operation were observed in 2 groups. RESULTS: Within one week after lung transplantation, 44 patients (68.8%) had experienced at least one episode of AKI, among which 19 cases (29.7%) were stage 1, 17 cases (26.5%) were stage 2 and 8 cases (12.5%) were stage 3. The incidence of AKI was the highest on post-operative day 4 (57.4%). The incidence of AKI at stage 3 exhibited growth trend within the first week after operation, and reached the highest on median post-operative day 5 (8.7%). Operation duration, median value of Scr within one week after operation, median tacrolimus concentration in non-AKI group were significantly shorter or lower than AKI group; there was no significant difference in operation type, ECMO support, use of immunosuppressive agents, intraoperative blood loss, ICU days, mechanical ventilation days, ECMO support days, the utilization rate of potential nephrotoxic drugs (≥4 kinds) and hospitalization days between 2 groups (P>0.05). There was no statistical significance in the survival rate at stage 1 and 2 one year after operation between AKI group and non-AKI group (P>0.05). One year after operation, survival rate of AKI group at stage 3 was significantly lower than that of non-AKI group(P<0.05). CONCLUSIONS: The incidence of AKI is high after lung transplantation. Operation duration, median value of Scr within one week after operation, median tacrolimus concentration were possible factors for the occurrence of AKI after operation.
1.4.2 术中影响因素 术中影响因素包括手术类型、手术时间、ECMO支持情况、免疫抑制剂使用情况和术中失血量。
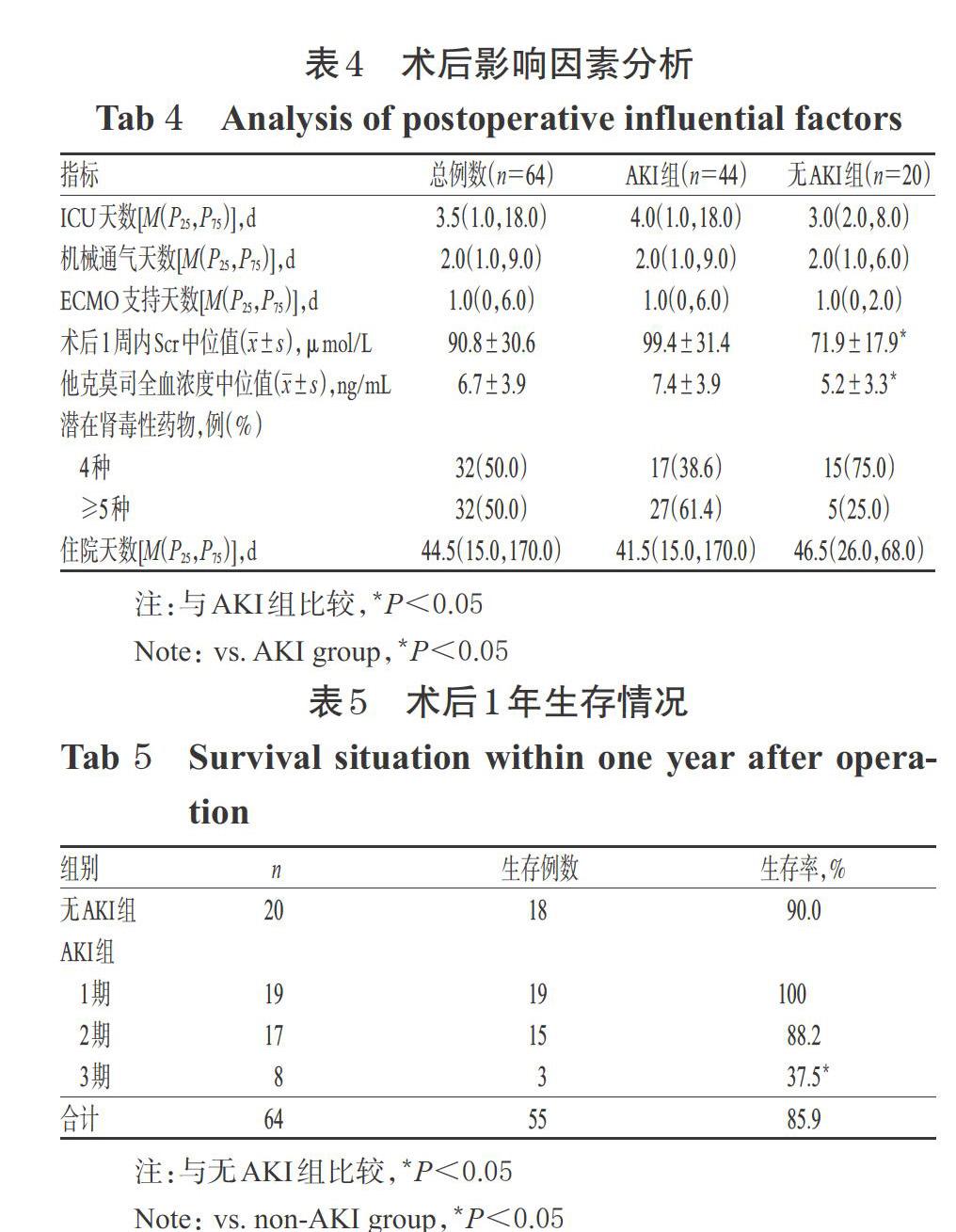
1.4.3 术后影响因素 术后影响因素包括患者重症加强护理病房(ICU)天数、机械通气天数、ECMO支持天数、术后1周内Scr中位值、他克莫司全血浓度中位值、潜在肾毒性药物种类(≥4种)、住院天数。
1.4.4 临床结局 观察两组患者术后1年的生存情况。
1.5 统计学方法
采用SPSS 23.0软件对数据进行统计分析。采用Shapiro-Wilk检验数据是否符合正态分布,对于符合正态分布的计量资料以x±s表示,两组间比较采用两独立样本t检验;非正态分布的计量资料以M(P25,P75)表示,两组间比较采用Mann-Whitney U检验;计数资料以例数或率表示,采用χ2检验或Fisher精确检验。P<0.05为差异有统计学意义。
2 结果
2.1 肺移植术后AKI发生情况
肺移植术后1周内,64例患者中有44例(68.8%)至少发生过1次AKI,其中1期19例(29.7%)、2期17例(26.5%)、3期8例(12.5%)。术后第4天AKI发生率最高(57.4%),肺移植术后1周内3期AKI发生率总体呈上升趋势,并在术后第5天达到最高(8.7%),详见表2(因术后并非每天都会检测患者肾功能,因此Scr值不是每天都可获得;此外,通常在术后前3 d会每天测Scr值,从第4天起医师根据患者病情决定是否检测肾功能,故表中“n”表示实际测定肾功能的患者例数)。
2.2 术中影响因素分析
无AKI组患者的手术时间显著短于AKI组(P<0.05);而两组患者手术类型、ECMO支持情况、免疫抑制剂使用例数、术中失血量比较,差异均无统计学意义(P>0.05),详见表3。
2.3 术后影响因素分析
所有患者术后均在ICU实施有创呼吸机和/或ECMO辅助通气。无AKI组患者术后1周内Scr中位值、他克莫司全血浓度中位值均显著低于AKI组(P<0.05)。而两组患者ICU天数、机械通气天数、ECMO支持天数、潜在肾毒性药物(≥4种)使用率、住院天数比较,差异均无统计学意义(P>0.05),详见表4。
2.4 术后1年生存情况
1期和2期AKI患者术后1年生存率与无AKI组比较,差异均无统计学意义(P>0.05);而3期AKI患者术后1年生存率显著低于无AKI组(P=0.009),详见表5。
3 讨论
随着器官移植医学伦理的完善和终末期肺疾病患病人数的增加,行肺移植术的患者也在逐年增多,尽管我国在外科手术和免疫抑制治疗等方面取得了进展,大大提高了患者的生存率,但部分患者术后仍伴有严重的并发症,尤其是AKI[2,12]。据国际心肺移植学会(ISHLT)统计数据显示,肺移植术后1年内肾功能不全较糖尿病和闭塞性细支气管炎等并发症更为常见,且与患者死亡显著相关[13-14]。
有研究认为,应用不同的AKI诊断标准可能会影响AKI发生的判断结果[15]。近年来研究大多采用2012年KDIGO指南[4,10,16]、2005年急性肾损伤网络(AKIN)标准[17-18]或2002年急性透析质量指导组(ADQI)提出的风险、损伤、衰竭、失功能、终末期肾病(RIFLE)分层标准[19-20]。Lertjitbanjong P等[21]进行的Meta分析结果显示,根据KDIGO指南、AKIN标准和RIFLE分层标准,肺移植术后AKI的合并估计发病率分别为53.0%[95%置信区间(CI)(38.2%,67.3%)]、55.5%[95%CI(45.2%,65.4%)]和49%[95%CI(38.3%,59.8%)]。本研究采用KDIGO指南的AKI诊断标准得到的结果显示,肺移植术后1周内,AKI发生率为68.8%,其中1期占29.7%、2期占26.5%、3期占12.5%,术后AKI以1期和2期为主,该结果与相关研究[4,11]结论一致。
本研究结果显示,无AKI组患者的手术时间显著短于AKI组,提示接受手术时间越长,患者发生AKI的风险越高,该结果目前尚未有相关文献报道。肺部手术会通过释放炎症介质而致肾上皮细胞凋亡,从而引发AKI[22]。由此笔者推测,手术时间延长可能会加重上述过程,进而增加AKI发生的可能性。有研究报道,肺移植术中影响AKI的发生因素为双肺移植和ECMO支持等[2,22-24]。而本研究发现,虽然AKI组中双肺移植患者比例(34.1%)虽略高于无AKI组(25.0%),但差异无统计学意义,这可能与本研究中纳入的双肺移植患者较少有关[2,25]。同时,本研究还发现,单肺移植患者的手术时间短于双肺移植手术时间,笔者推测手术类型可能会间接影响手术时间与术后AKI的相关性[22-23]。术中使用ECMO支持而导致AKI的机制可能与血液持续暴露于ECMO界面而使促炎介质激活有关[26]。虽然我院肺移植手术中ECMO支持总体率较高(73.4%),但并未发现ECMO支持是患者术后发生AKI的影响因素,该结论与相关文献[2,25]结论一致。此外,虽然两组患者术中失血量比较差异无统计学意义。也有研究认为,1~3期AKI患者的术中失血量虽然高于无AKI组,但组间比较差异无统计学意义(P=0.054)[15]。但由于本研究纳入的样本量较小,因此,术中出血量是否为患者术后发生AKI的可能影响因素,仍需后续研究进一步证实。
免疫抑制剂可能在AKI的发生中发挥重要作用[27]。他克莫司是肺移植术后常用的免疫抑制剂,其潜在的肾毒性已在多項研究中被提及[11,28]。他克莫司的肾毒性可能是由于其浓度偏高时,引起肾小球入球小动脉血管收缩而造成的[29]。本研究结果显示,AKI组患者术后他克莫司全血浓度中位值显著高于无AKI组,这与文献报道[4,30]结果一致。但值得注意的是,AKI组患者体内他克莫司的全血浓度[(7.4±3.9)ng/mL]并未超出目标浓度范围(8~12 ng/mL),提示常规测定的他克莫司全血浓度即使位于目标浓度范围内,可能也会造成肾毒性[4]。Sikma MA等[4]研究认为,在肾毒性方面,他克莫司游离血浆浓度可能比全血浓度更具相关性,但由于游离血浆浓度不能通过常规分析测量,因此该相关性仍需后续研究验证。
本研究中,所有患者的1年生存率为85.9%,该结果与文献报道[31]一致。1期和2期AKI患者术后1年生存率与无AKI组比较,差异均无统计学意义;3期AKI患者术后1年生存率显著低于无AKI组,这与Bennett D等[25]研究结果一致,提示术后发生严重AKI患者的死亡风险可能更高。
综上所述,肺移植术后AKI的发生率较高。手术时间、术后1周内Scr中位值、他克莫司全血浓度中位值均为术后发生AKI的可能影响因素。尽管目前未有确切可行的预防术后AKI发生的相关方案,但对上述影响因素进行干预,可能会有助于减少AKI的发生、改善患者预后。由于本研究为回顾性分析,且纳入的样本量较小,故此结论可能会存在偏倚,后续仍需扩大样本量进一步证实。
参考文献
[ 1 ] 田普训,敖建华,李宁,等.器官移植免疫抑制剂临床应用技术规范:2019版[J].器官移植,2019,10(3):213-226.
[ 2 ] ATCHADE E,BAROUR S,TRAN-DINH A,et al. Acute kidney injury after lung transplantation:perioperative risk factors and outcome[J]. Transplant Proc,2020,52(3):967-976.
[ 3 ] CHAWLA LS,BELLOMO R,BIHORAC A,et al. Acute kidney disease and renal recovery:consensus report of the acute disease quality initiative(ADQI)16 workgroup[J]. Nat Rev Nephrol,2017,13(4):241-257.
[ 4 ] SIKMA MA,HUNAULT CC,VAN DE GRAAF EA,et al. High tacrolimus blood concentrations early after lung transplantation and the risk of kidney injury[J]. Eur J Clin Pharmacol,2017,73(5):573-580.
[ 5 ] ROCHA PN,ROCHA AT,PALMER SM,et al. Acute renal failure after lung transplantation:incidence,predictors and impact on perioperative morbidity and mortality[J]. Am J Transplant,2005,5(6):1469-1476.
[ 6 ] TJAHJONO R,CONNELLAN M,GRANGER E. Predictors of acute kidney injury in cardiac transplantation[J]. Transplantation Proc,2016,48(1):167-172.
[ 7 ] 陳彩妹,王凉,薛婧,等.肺移植术后急性肾损伤的危险因素及预后分析[J].中国血液净化,2015,14(3):155-158.
[ 8 ] KHWAJA A. KDIGO clinical practice guidelines for acute kidney injury[J]. Nephron Clin Pract,2012,120(4):c179- c184.
[ 9 ] 薛婧,孙铸兴.肺移植后急性肾损伤的研究进展[J].实用医学杂志,2012,28(18):3149-3151.
[10] STEVENS LA,CORESH J,GREENE T,et al. Assessing kidney function-measured and estimated glomerular filtration rate[J]. N Engl J Med,2006,354(23):2743-2483.
[11] MIANO TA,FLESCH JD,FENG R,et al. Early tacrolimus concentrations after lung transplant are predicted by combined clinical and genetic factors and associated with acute kidney injury[J]. Clin Pharmacol Ther,2020,107(2):462-470.
[12] CHAMBERS DC,CHERIKH WS,GOLDFARB SB,et al. The international thoracic organ transplant registry of the international society for heart and lung transplantation:thirty-fifth adult lung and heart-lung transplant report- 2018:focus theme:multiorgan transplantation[J]. J Heart Lung Transplant,2018,37(10):1169-1183.
[13] WEHBE E,DUNCAN AE,DAR G,et al. Recovery from AKI and short and long-term outcomes after lung transplantation[J]. Clin J Am Soc Nephrol,2013,8(1):19-25.
[14] CHAMBERS DC,YUSEN RD,CHERIKH WS,et al. The registry of the international society for heart and lung transplantation:thirty-fourth adult heart transplantation report:2017:focus theme:allograft ischemic time[J]. J Heart Lung Transplant,2017,36(10):1047-1059.
[15] XUE J,WANG L,CHEN CM,et al. Acute kidney injury influences mortality in lung transplantation[J]. Ren Fail,2014,36(4):541-545.
[16] SHASHATY MGS,FORKER CM,MIANO TA,et al. The association of post-lung transplant acute kidney injury with mortality is independent of primary graft dysfunction:a cohort study[J]. Clin Transplant,2019. DOI:10.1111/ctr.13678.
[17] BALCI MK,VAYVADA M,SALTURK C,et al. Incidence of early acute kidney injury in lung transplant patients:a single-center experience[J]. Transplant Proc,2017,49(3):593-598.
[18] RI HS,SON HJ,OH HB,et al. Inhaled nitric oxide therapy was not associated with postoperative acute kidney injury in patients undergoing lung transplantation:a retrospective pilot study[J]. Medicine:Baltimore,2018. DOI:10.1097/MD.0000000000010915.
[19] NGUYEN AP,GABRIEL RA,GOLTS E,et al. Severity of acute kidney injury in the post-lung transplant patient is associated with higher healthcare resources and cost[J]. J Cardiothorac Vasc Anesth,2017,31(4):1361-1369.
[20] AHMAD O,SHAFII AE,MANNINO DM,et al. Impact of donor lung pathogenic bacteria on patient outcomes in the immediate post-transplant period[J]. Transpl Infect Dis,2018. DOI:10.1111/tid.12986.
[21] LERTJITBANJONG P,THONGPRAYOON C,CHEUN- GPASITPORN W,et al. Acute kidney injury after lung transplantation:a systematic review and meta-analysis[J]. J Clin Med,2019,8(10):1713-1731.
[22] GEORGE TJ,ARNAOUTAKIS GJ,BEATY CA,et al. Acute kidney injury increases mortality after lung transplantation[J]. Ann Thorac Surg,2012,94(1):185-192.
[23] JACQUES F,EL-HAMAMSY I,FORTIER A,et al. Acute renal failure following lung transplantation:risk factors,mortality,and long-term consequences[J]. Eur J Cardiothorac Surg,2012,41(1):193-199.
[24] ISHIKAWA S,GRIESDALE DE,LOHSER J. Acute kidney injury within 72 hours after lung transplantation:incidence and perioperative risk factors[J]. J Cardiothorac Vasc Anesth,2014,28(4):931-935.
[25] BENNETT D,FOSSI A,MARCHETTI L,et al. Postoperative acute kidney injury in lung transplant recipients[J].Interact Cardiovasc Thorac Surg,2019,28(6):929-935.
[26] THONGPRAYOON C,CHEUNGPASITPORN W,LERTJITBANJONG P,et al. Incidence and impact of acute kidney injury in patients receiving extracorporeal membrane oxygenation:a meta-analysis[J]. J Clin Med,2019,8(7):981-1005.
[27] PUTTARAJAPPA CM,BERNARDO JF,KELLUM JA. Renal complications following lung transplantation and heart transplantation[J]. Critical Care Clinics,2019,35(1):61-73.
[28] CALABRESE DR,FLOREZ R,DEWEY K,et al. Genotypes associated with tacrolimus pharmacokinetics impact clinical outcomes in lung transplant recipients[J]. Clin Transplant,2018. DOI:10.1111/ctr.13332.
[29] NAESENS M,KUYPERS DR,SARWAL M. Calcineurin inhibitor nephrotoxicity[J]. Clin J Am Soc Nephrol,2009,4(2):481-508.
[30] SIKMA MA,HUNAULT CC,KIRKELS JH,et al. Association of whole blood tacrolimus concentrations with kidney injury in heart transplantation patients[J]. Eur J Drug Metab Pharmacokinet,2018,43(3):311-320.
[31] FIDALGO P,AHMED M,MEYER SR,et al. Incidence and outcomes of acute kidney injury following orthotopic lung transplantation: a population-based cohort study[J]. Nephrol Dial Transplant,2014,29(9):1702-1709.
(收稿日期:2020-05-13 修回日期:2020-08-01)
(編辑:陈 宏)