侧脑室引流术与小脑血肿微创穿刺术治疗小脑出血的临床效果
饶辉
【关键词】 侧脑室引流术 小脑血肿微创穿刺术 小脑出血
[Abstract] Objective: To analyze the clinical effect of lateral ventricle drainage and minimally invasive puncture of cerebellar hematoma in the treatment of cerebellar hemorrhage. Method: A total of 64 patients with cerebellar hemorrhage in our hospital from June 2018 to June 2020 were selected and randomly divided into the control group and the observation group according to random number table, 32 cases in each group. The observation group was treated with minimally invasive puncture of cerebellar hematoma, while the control group was treated with lateral ventricle drainage. The incidence of postoperative complications were compared between two groups, GCS, SSS scores before and after treatment, hs-CRP and NSE before and 1, 3 and 7 d after treatment were compared between two groups. Result: Before treatment, there were no significant differences in GCS and SSS scores between two groups (P>0.05); after treatment, the GCS and SSS scores of the observation group were higher than those of the control group, the differences were statistically significant (P<0.05). Before and 1 d after treatment, there were no significant differences in serum hs-CRP between two groups (P>0.05); 3 and 7 d after treatment, serum hs-CRP of two groups were lower than those of before treatment, and the observation group were lower than those of the control group, the differences were statistically significant (P<0.05). There were no significant differences in serum NSE between two groups before treatment and 1 and 3 d after treatment (P>0.05); 7 d after treatment, serum NSE of two groups were lower than those of before treatment, and the observation group was lower than that of the control group, the differences were statistically significant (P<0.05). The incidence of complications of the observation group was lower than that of the control group, the differences was statistically significant (P<0.05). Conclusion: Minimally invasive puncture of cerebellar hematoma is superior than lateral ventricle drainage in the treatment of cerebellar hemorrhage, which is worthy of popularization and application.
[Key words] Lateral ventricle drainage Minimally invasive puncture of cerebellar hematoma Cerebellar hemorrhage
First-author’s address: Xiaogan Hospital Affiliated to Wuhan University of Science and Technology (Xiaogan Central Hospital), Xiaogan 432000, China
doi:10.3969/j.issn.1674-4985.2021.21.019
小脑出血主要症状为四肢协调性变差、眼球震动等,严重者会出现昏迷等情况,给患者生命安全造成很大威胁[1]。目前临床常用治疗手段为侧脑室引流术及小脑血肿微创穿刺术,临床应用中发现小脑血肿微创穿刺术效果更佳,在治疗小脑出血方面更具优势[2]。对本院64例小脑出血患者分别采用侧脑室引流术及小脑血肿微创穿刺术进行治疗,比较其疗效。现报道如下。
1 资料与方法
1.1 一般资料 选取2018年6月-2020年6月本院收治的64例小脑出血患者。纳入标准:(1)经过影像学检查均确诊为小脑出血;(2)血肿量>10 mL以上;(3)血肿量虽<10 mL,但破入或是邻近第四脑室,导致其出现移位、变形,引发脑脊液循环障碍,出现颅内压上升;(4)年龄40岁以上;(5)出血时间小于72 h。排除标准:(1)合并凝血障碍;(2)合并颅内或全身感染;(3)合并心、肺、肝、肾等严重疾病。根据随机数字表法将其分为对照组和观察组,每组32例。本研究经医院伦理委员会批准通过,患者均知情同意。
1.2 方法 观察组给予微创穿刺术治疗,首先选择合适穿刺点(正中矢状线旁开2.5 cm与横窦线下1.5 cm交点),利用CT测量穿刺点至靶心的距离,根据距离选择合适长度的针。然后进行穿刺,主要根据颅中线、上项线、基线进行穿刺,穿刺时注意穿刺方向与基线及正中矢状线平行,穿刺后将患者颅内血肿彻底清除。对照组给予侧脑室引流术,指导患者取平卧位,选择合适穿刺点(矢状线自眉间向上9 cm,中线旁开2 cm交点),并进行常规消毒以及浸润麻醉。然后由脑膜针进行穿刺,再通过引流管将脑脊液移出。
1.3 观察指标与判定标准 (1)比较两组治疗前后格斯拉哥昏迷量表(GCS)评分。GCS主要对患者昏迷程度进行测定,该量表包括四个级别:15分为正常,12~14分为轻度意识障碍,9~11分为中度意识障碍,8分以下为昏迷[3]。(2)比较两组治疗前后斯堪地纳维亚卒中量表(SSS)评分:采用SSS主要对患者神经功能进行测定,其测定主要包括:意识状态、眼球运动、上肢肌力、语言、面瘫等方面,总分58分,<26分为神经功能重度缺损,≥26分为轻、中度缺损,分数越高,说明神经功能缺损程度越轻[4]。(3)比较两组治疗前及治疗后1、3、7 d的NSE和hs-CRP水平。采取两组清晨空腹静脉血5 mL,采用酶联免疫吸附法方法测定NSE和hs-CRP水平。(4)比较两组术后并发症,包括脑积水和共济失调。
1.4 统计学处理 本研究采用SPSS 20.0软件对所得数据进行统计分析,计量资料用(x±s)表示,组间比较采用独立样本t检验,组内比较采用配对t检验;计数资料以率(%)表示,比较采用字2检验。以P<0.05为差异有统计学意义。
2 结果
2.1 两组一般资料比较 观察组男17例,女15例;年龄48~78岁,平均(62.56±5.74)岁;单侧脑室扩大20例,双侧脑室扩大12例;出血量10~25 mL,平均(17.65±2.15)mL。对照组男18例,女14例;年龄49~79岁,平均(62.97±5.65)岁;单侧脑室扩大21例,双侧脑室扩大11例;出血量11~25 mL,平均(17.89±2.34)mL。两组一般资料比较,差异均无统计学意义(P>0.05),具有可比性。
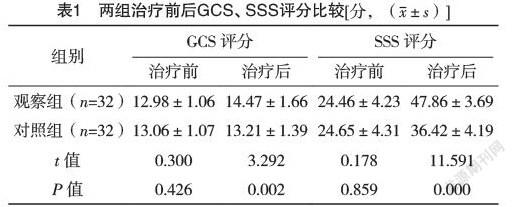
2.2 两组治疗前后GCS、SSS评分比较 治疗前,两组GCS、SSS评分比较,差异均无统计学意义(P>0.05);治疗后,观察组GCS、SSS评分均高于对照组,差异均有统计学意义(P<0.05)。见表1。
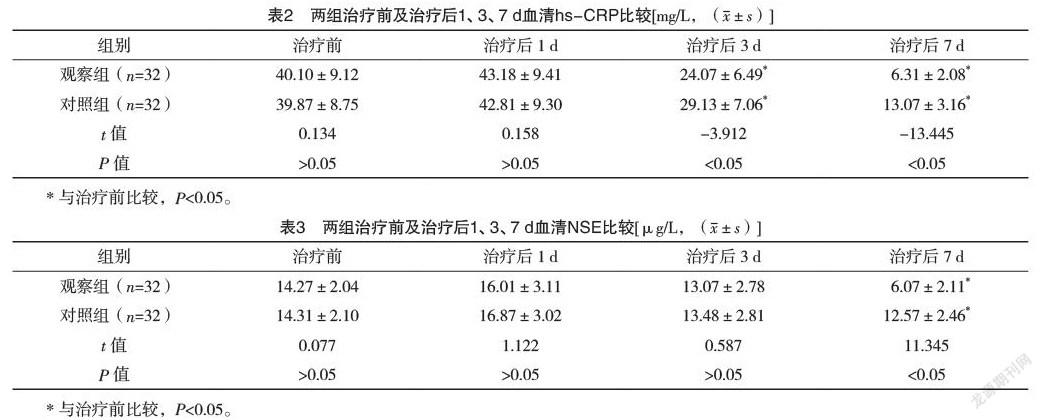
2.4 两组治疗前及治疗后1、3、7 d血清NSE比较 治疗前及治疗后1、3 d,两组血清NSE比较,差异均无统计学意义(P>0.05);治疗后7 d,两组血清NSE均低于治疗前,且观察组低于对照组,差异均有统计学意义(P<0.05)。见表3。
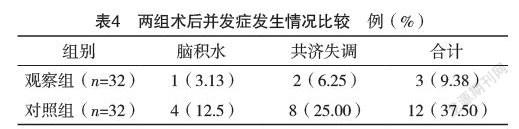
2.5 两组术后并发症发生情况比较 观察组并发症发生率低于对照组,差异有统计学意义(字2=7.053,P<0.05),见表4。
小脑出血的原因以高血压较为常见,出血后易导致患者残疾,甚至死亡[5]。小脑出血的好发部位为齿状核区域。出血的位置(靠近中线或位于两侧)影响患者的症状和临床过程,这可能比血肿大小对预后的影响更为重要[6-7]。一般而言,血肿越靠两侧、体积越小,越可能避免脑干受累,预后越好;而位于小脑蚓部的出血则是导致患者早期死亡的重要风险因素[8-9]。小脑出血是由于脑干受到血肿影响,阻碍脑脊液循环,使患者出现出血的情況,临床死亡率较高,因此需尽早进行治疗,以降低患者致残率,保障其生命安全[10-11]。
脑室外引流术简便易行,手术难度不大,在基层医院可实施[12]。手术过程中适当抽吸脑室内积血、术后持续引流,可以促使脑室系统尽早恢复通畅;脑室内血液及其分解产物被引流出后,可以减少其在蛛网膜下腔的聚集,减轻对颅底血管神经及脑膜的刺激,但此手术常见的风险在于引流感染[13-14]。微创穿刺术主要是通过血肿清除术进一步将血液引流至脑室外。该方式相比较侧脑室引流术安全性更高,效果更好,可有效降低死亡率,改善患者预后[15-16]。有研究表明,血肿微创穿刺术可有效将患者颅内血肿进行清除,从而避免再次出血及颅内感染情况,进一步降低颅内压,可有效降低患者的致残率[17-18]。本研究采用侧脑室引流术与小脑血肿微创穿刺术对患者进行治疗,得出结果:治疗前,两组GCS、SSS评分比较,差异均无统计学意义(P>0.05);治疗后,观察组GCS、SSS评分高于对照组,差异均有统计学意义(P<0.05)。治疗后3、7 d,观察组血清hs-CRP、NSE均低于对照组,差异均有统计学意义(P<0.05)。这提示该手术方式可以有效将患者脑部血肿及血液清除,并且对患者造成的伤害较小,很大程度上减轻对脑干的伤害,从而避免术后并发症的发生,进一步降低患者死亡率,提高治疗效果[19-20]。
综上所述,小脑血肿微创穿刺术治疗小脑出血效果优于侧脑室引流术,值得推广应用。
参考文献
[1]郭亚辉,任二朋.微创穿刺联合侧脑室外引流术治疗高血压性小脑出血并脑积水患者的近期随访研究[J].齐齐哈尔医学院学报,2019,40(5):600-601.
[2]许峰,陶英群,孙霄,等.ROSA辅助与传统幕下开颅术治疗小脑出血的临床研究[J].中国微侵袭神经外科杂志,2017,22(2):57-59.
[3]陈苑新,黄鹏,徐财文,等.小脑出血破入脑室行枕大池引流的临床效果[J].深圳中西医结合杂志,2020,30(8):187-188.
[4] Parazzini F,Di Cintio E,Chatenoud L,et al.Estroprogestin vs.gonadotropin agonists plus estroprogestin in the treatment of endometriosis-related pelvic pain:a randomized trial[J].European Journal Of Obstetrics And Gynecology And Reproductive Biology,2000,88(1):11.
[5] Dmowski W P,Pry M,Ding J,et al.Cycle-specific and cumulative fecundity in pstients with endometriosis who are undergoing controlled ovarian hyperstimulation-intrauterine insemination or vitro fertilization-embryo transfer[J].Eertility Sterility,2017,78(4):750-756.
[6]陈祎招,徐如祥.高血压脑出血神经内镜微创手术与开颅血肿清除术的临床比较分析[J].中国神经精神疾病杂志,2015,36(10):616-619.
[7]许小兵,林发牧,李子坚.神经内镜治疗高血压脑出血术后早期再出血的原因与对策[J].广东医学,2015,36(22):3462-3465.
[8]蔡康,郑宽,李卫.“梯度减压”对高血压脑出血术中急性脑膨出的预防作用[J].实用医学杂志,2016,32(3):417-420.
[9]范学政,游潮.国内高血压脑出血微创血肿清除手术治疗现状及趋势[J].中华神经医学杂志,2017,16(9):956-961.
[10]蒋荣宽,程远.早期小骨窗手术治疗幕上高血压脑出血的临床疗效分析[J].激光杂志,2015,32(3):63-64.
[11]张文超,杨雪辉,郭昊.高血压脑出血患者立体定向微创颅内血肿清除术的最佳时机分析[J].山东医药,2017,57(20):92-95.
[12] Chang J H,Au H K,Lee W C,et al.Expression of the pluripotent transcription factor OCT4 promotes cell migration in endometriosis[J].Fertility & Sterility,2013,99(5):656-657.
[13] Jowicz A P,Brown J K,McDonald E S,et al.Characterization of the temporal and spatial expression of a disintegrin and metalloprotease 17 in the human endometrium and fallopian tube[J].Reproductive Sciences,2016,20(11):592-593
[14]刘慧权,张建宁,尹悦.抗血小板治疗对中老年轻型颅脑损伤患者预后的影响[J].中华创伤杂志,2017,33(1):47-50.
[15]李洋阳,吴卫娟,孟然.脑梗死并发丘脑综合征的研究进展[J/OL].中华临床医师杂志:电子版,2017,11(1):91-94.
[16]杨学,陈劲草,张雪梅,等.小骨窗开颅与立体定向置管抽吸治疗基底节区高血压脑出血的临床研究[J].中西医结合心脑血管病杂志,2016,14(13):1472-1474.
[17]杨海峰,孙跃春,崔刚,等.神经内镜技术在基底节区高血压脑出血治疗中的应用[J].中国临床医生杂志,2015,43(7):63-64.
[18]王武祥.小骨窗开颅手术治疗基底节区高血压脑出血[J].安徽医学,2013,34(6):775-776.
[19]王浩,郑德宇,秦书俭,等.高血压脑出血临床特点与微创治疗优势临床观察[J].山东医药,2011,51(32):76-77.
[20]常鹏飞,邬巍,左程,等.单双管微创穿刺引流术治疗大量基底节区高血压脑出血的疗效比较[J].中华实验外科杂志,2015,32(9):2258-2260.
(收稿日期:2020-10-14) (本文編辑:张明澜)