Effectiveness of herb-partitioned moxibustion combined with electroacupuncture on polycystic ovary syndrome in patients with symptom pattern of kidney deficiency and phlegm-dampness
ZHAO Qingyi,SUN Yi,ZHOU Jing,GAO Yanling,MA Guizhi,HU Zhihai,WANG Yi,SHI Yin
ZHAO Qingyi,SUN Yi,GAO Yanling,Graduate School,Shanghai University of Traditional Chinese Medicine,Shanghai 201203,China
ZHOU Jing,MA Guizhi,HU Zhihai,WANG Yi,Department of Acupuncture and Moxibustion,Shanghai TCM-Integrated Hospital,Shanghai University of Traditional Chinese Medicine,Shanghai 200082,China
SHI Yin,Key Laboratory of Acupuncture and Immunological Effects,Yueyang Hospital of Integrated Traditional Chinese and Western Medicine Affiliated to Shanghai University of Traditional Chinese Medicine,Shanghai 200437,China;Outpatient Department,Shanghai Research Institute of Acupuncture and Meridian,Shanghai 200030,China
Abstract OBJECTIVE:To observe the effect of herb-partitioned moxibustion combined with electroacupuncture on polycystic ovary syndrome (PCOS) in patients with symptom pattern of kidney deficiency and phlegm-dampness.METHODS:Totally 62 PCOS patients who met the inclusion criteria were randomly divided into intervention group and control group.In the intervention group,acupoints were subjected to(43±1)℃herb-partitioned moxibustion and electroacupuncture treatment.In the control group,acupoints were subjected to(37±1)℃herb-partitioned moxibustion and sham electroacupuncture treatment.Treatment was provided 3 times per week for 12 weeks,and the treatment was stopped during menstruation.After the treatment,the clinical efficacy,the Traditional Chinese Medicine (TCM) symptom pattern score,basal body temperature (BBT) levels,menstrual cycle,and related sex hormone levels of the two groups were evaluated.RESULTS:Sixty patients were eventually included in the study(30 in the intervention group and 30 in the control group).There were not obvious between-group differences in the baseline efficacy parameters (all P >0.05).(a) After treatment,the two groups have improved in terms of clinical efficacy,TCM symptom pattern score,menstrual cycle and,BBT (P < 0.01, < 0.05),and the intervention group was better than the control group(P<0.01,<0.05).(b)In the intervention group,the estradiol(E2)and P450 aromatase (P450arom) levels were increased(all P < 0.05),the testosterone (T) level was decreased (P < 0.05),and the luteotropic hormone(LH)and anti-Müllerian hormone(AMH)levels were significantly decreased (P < 0.01).In the control group,E2 level was increased(P<0.05),and LH level was decreased (P <0.05).After treatment,the T,LH,and AMH levels of the intervention group were decreased compared with those of the control group (all P < 0.05),and the P450arom level was increased(P<0.05).CONCLUSIONS:Herb-partitioned moxibustion combined with electroacupuncture can effectively improve the related clinical symptoms of PCOS patients with kidney deficiency and phlegm-dampness.Herb-partitioned moxibustion combined with electroacupuncture may inhibit the overexpression of AMH to increase the expression level of P450arom in ovarian granulosa cells,thereby reconstructing the dependence of follicular development on FSH,and finally improving abnormal follicular development and hyperandrogenism in PCOS patients with kidney deficiency and phlegmdampness.Trial registration number:ChiCTR1900024182.
Keywords:moxibustion;electroacupuncture;polycystic ovary syndrome;kidney deficiency and phlegm-dampness
INTRODUCTION
Polycystic ovary syndrome (PCOS) is characterized by abnormal follicular development or anovulation and hyperandrogenism,and the clinical manifestations include changes in the menstrual cycle,reproductive disorders,etc.1A total of 5%to 18%of reproductive-age women have PCOS,and the figure in China is 5.6%.2In addition,30 % to 60 % of these patients are affected by an ovulation disorder or by non-ovulation.3Because the disease involves many factors,PCOS presents with a high degree of heterogeneity in pathogenesis,biochemical changes,and clinical manifestations.2In western medicine,the disease is treated with estrogen and progestin drugs,aromatase,or steroid hormone drugs.4However,long-term use of hormonal drugs is likely to cause a series of adverse reactions.For patients of childbearing age,this disease can lead to long-term anovulation and infertility.5As such,it is important to investigate the etiology and pathogenesis of PCOS and find a safe and effective method to prevent and cure the disease.
According to previous studies,anti-Müllerian hormone(AMH),which is secreted by follicular granulosa cells,and not only can inhibit the initial recruitment of primordial follicles but also can reduce the sensitivity of follicles to follicle-stimulating hormone (FSH) during development,thereby inhibiting the development of growing follicles and the formation of dominant follicles.6,7AMH is closely related to the hyperandrogenism of PCOS because it can also decrease the expression or activity of P450 aromatase (P450arom) (also known as CYP19,a key enzyme in follicular granulosa cells that can convert androgens into estrogens)in follicular granulosa cells.8In recent years,traditional Chinese medical electroacupuncture techniques have attracted greater interest due to their clinical effectiveness and negligible side effects.9,10Clinical studies have shown that acupuncture treatment of PCOS can reduce a patient's body mass index (BMI),11and it can reduce fasting insulin (FINS) and testosterone (T) levels.12Animal experiments have also shown that electroacupuncture intervention in PCOS rat models can restore the estrous cycle and ovarian morphology,reduce T levels in peripheral blood and ovaries,and increase estradiol (E2)and P450arom levels;these data suggest that electroacupuncture can promote the normal conversion of androgens into estrogen in PCOS rat models to regulate the high androgen levels that are found in the ovarian microenvironment and to promote follicle development.13,14In addition,electroacupuncture can downregulate the abnormal overexpression of AMH in PCOS rat models,reduce cystic follicular expansion,and significantly increase the number of follicular granulosa cells,thereby improving sex hormone disorders and follicular development disorders associated with PCOS.15Based on our previous study,kidney deficiency and phlegm-dampness are the most common Traditional Chinese Medicine (TCM) symptoms in PCOS patients,16,17and the purpose of this study was to observe the effect of herb-partitioned moxibustion combined with electroacupuncture on PCOS in patients with symptom pattern of kidney deficiency and phlegm-dampness.
MATERIALS AND METHODS
Participants
This randomized single-blinded,placebo-controlled trial was registered on the Chinese website for registration of clinical trials (http://www.chictr.org.cn/:ChiCTR1900024182) and followed the Declaration of Helsinki and Good Clinical Practice guidelines.A total of 62 subjects were enrolled from the medical outpatient department of Shanghai Institute of Acupuncture and Meridian and the PCOS special outpatient clinic of Shanghai Integrated Chinese and Western Medicine Hospital.The study was approved by the ethics committee of Yueyang Hospital of Integrated Traditional Chinese and Shanghai TCM-Integrated Hospital,Shanghai University of Traditional Chinese Medicine.Written informed consent was obtained from all participants prior to the treatment.
Randomization and blinding
A simple random method was adopted,and IBM SPSS Statistics (Version 26.0,IBM Corp,Armonk,NY,USA) software was used to generate random numbers.62 patients with kidney deficiency and phlegm-dampness PCOS who met the inclusion criteria were randomly divided into intervention group(31 patients) and control group (31 patients).In this study,a single-blind method (patients did not know the group they were in) was used to ensure the treatment,evaluation,and analysis are independent of each other.
Diagnostic criteria
Diagnostic standards in Western Medicine:PCOS was diagnosed according to the Rotterdam criteria issued by the European Human Reproduction and Embryology Research Center and the American Society for Reproductive Medicine in 2003.18Patients who suffered the two of the following indexes were diagnosed with PCOS:(a) slight ovulation or no ovulation;(b) clinical manifestations of hyperandrogenemia and (or) hyperandrogenism (such as hirsutism and acne);(c) ≥12 small follicles,2-9 mm in diameter,in both ovaries,and (or) ovarian volume ≥10 mL.Patients with congenital adrenal hyperplasia,thyroid disease,androgen-secreting tumors,or Cushing's syndrome were excluded.
Symptom pattern identification in TCM:all patients have kidney deficiency and phlegm-dampness.The main symptoms are oligomenorrhea,low volume or even amenorrhea or dripping,lassitude in the loin and knee,cold limbs,obesity,hirsutism,acne,infertility,a pale and fat tongue with thick and white coating,and a sunken,thready,and slippery pulse.19
Inclusion and exclusion criteria
The inclusion criteria were listed as follows:(a) patients who met PCOS diagnostic criteria in western medicine and symptom pattern identification in TCM;(b) patients with no secondary PCOS,namely,no other systemic diseases;(c) female patients 14-49 years old;(d) patients accepting no other treatments during treatment;(e) the patient's TCM symptom pattern identification is of kidney deficiency with phlegm-dampness;(f) patients voluntarily participating in the study and signing a participation release agreement.
The exclusion criteria were as follows:(a) patients with congenital adrenal hyperplasia,thyroid disease,androgen-secreting tumors,and Cushing's syndrome;(b) patients suffering from other serious diseases;(c)patients taking hormonal and metabolic drugs affecting the judgment of results;(d) patients have fertility requirement for 12 weeks during treatment.
Treatments
In the intervention group,the acupoints of Guanyuan(CV4),Zhongji (CV3),Zigong (EX-CA1) (bilateral),Zusanli (ST36) (bilateral),Fenglong (ST40) (bilateral),Xuehai (SP10) (bilateral),Sanyinjiao (SP6) (bilateral),and Taixi (KI3) (bilateral) were used.These acupoints were based on the national standard (GB/T12346-2006) of the People's Republic of China for the name and location of acupoints.After routine disinfection of the acupoint area,Guanyuan (CV4),Zhongji (CV3) and Zigong (EX-CA1) were applied with herb-partitioned moxibustion,and moxa cones(0.5 cm in diameter,0.3 cm in length,and 90 mg in weight,"Hanyi Brand",Nanyang Hanyi moxa Co.,Ltd,Nanyang,China) made of refined mugwort floss were ignited after being placed on an herbal cake that was made of yellow rice wine and powdered herbs(monkshood,cinnamon,Radix Salvia Miltiorrhiza,safflower,and wormwood).Two moxa cones were applied once daily at each acupoint per single treatment with a temperature of (43 ± 1) ℃,which was measured by a far-infrared thermometer (Fluke 62,Fluke Corporation,Everett,Washington state,USA).Bilateral Zusanli(ST36),Fenglong(ST40),Xuehai(SP10),Sanyinjiao(SP6),and Taixi(KI3)points were stimulated with disposable sterile acupuncture needle(0.30 mm in diameter and 40mm in length,"Huatuo Brand",Suzhou Medical Supplies Co,Ltd.,Suzhou,China).Then,Zusanli(ST36)and Sanyinjiao(SP6)points were connected to Han's acupoint nerve stimulator (HANS-200A,Wuxi Yulong Electronic Technology Co.,Ltd.,Wuxi,China) for 30 min once every other day for 12 weeks,and the treatment was stopped during menstruation.
In the control group,acupoint selection and the treatment course were applied the same as that in the intervention group.Control group patients were subjected to sham electroacupuncture and herb-partitioned moxibustion with a temperature of (37 ± 1) ℃.After routine disinfection of the acupoint area,Guanyuan(CV4),Zhongji (CV3),and Zigong (EX-CA1) were applied with sham herb-partitioned moxibustion;the sham was a piece of cardboard between moxa cones and herbal cake that let patients feel warm.For sham electroacupuncture,the same points were used as those in the intervention group.The disposable external cannula-type flat needles (0.35 mm in diameter and 50 mm in length,"Huatuo Brand",Suzhou Medical Supplies Co.,Ltd.,Suzhou,China) was placed on the skin surface of the acupuncture point,and the trocar needles were performed without penetrating the skin.In other words,the cannula containing the flat needle was inserted into the base on the fixed surface of the acupoint.The skin was not punctured,and the patient only felt slight pain.And there was no electricity in Han's Acupoint Nerve Stimulator(Figure 1).
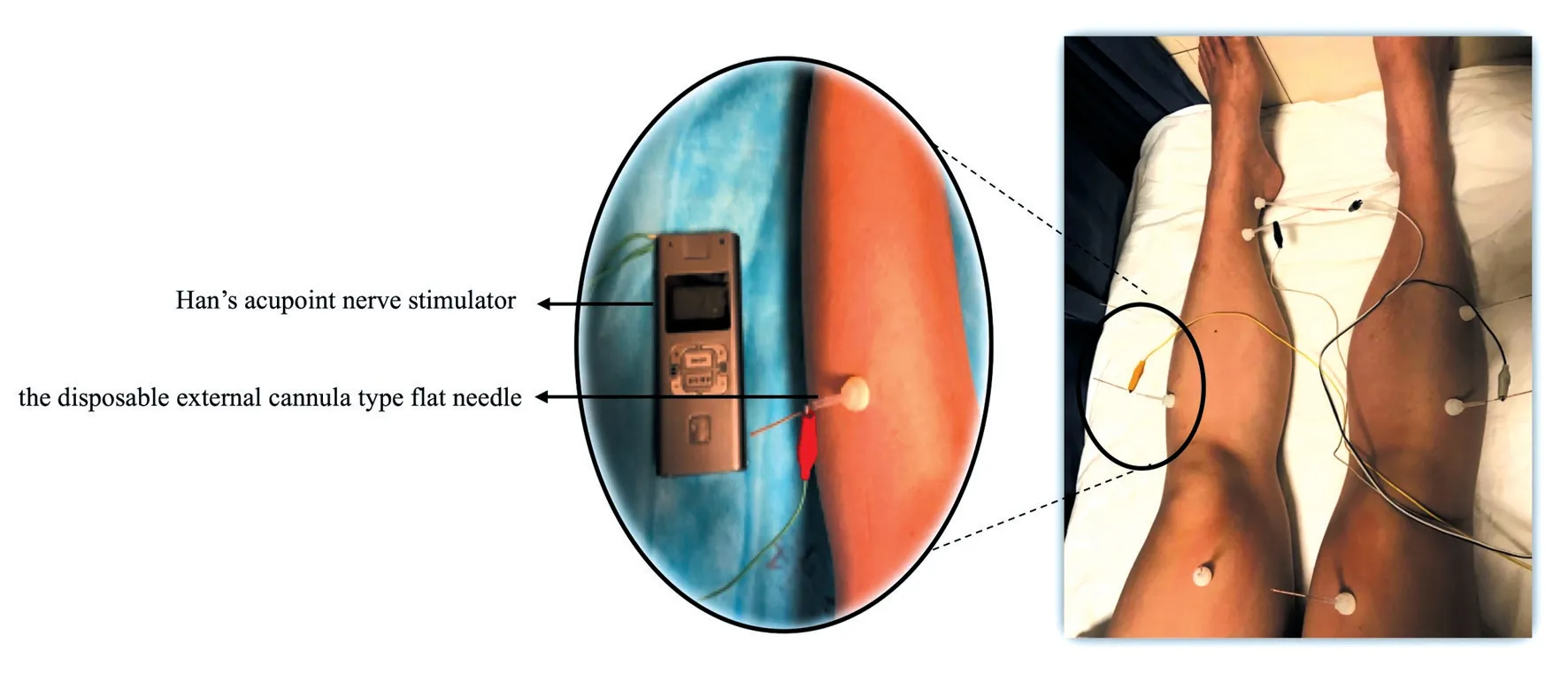
Figure 1 Sham electroacupuncture operation diagram
Outcome assessment
All outcomes were measured at baseline and after 12 weeks of treatment,and the original data were recorded in case report forms.Hormone levels were considered the primary outcomes,and TCM symptom pattern score,basal body temperature (BBT),and menstrual cycle were recognized as the secondary outcomes.
TCM symptom pattern efficacy index criteria
The diagnostic criteria for PCOS with kidney deficiency and phlegm-dampness in the "Guiding Principles for Clinical Research of New Chinese Medicines" and"Guidelines for the Diagnosis and Treatment of Common Gynecological Diseases in Traditional Chinese Medicine" are formulated:TCM symptom efficacy index=(score before treatment- score after treatment)/score before treatment ×100 %.(a) recovery:TCM symptom pattern efficacy index ≥90%;(b) effective:TCM symptom pattern efficacy index ≥33.3%;(c)invalid:TCM symptom pattern efficacy index<33.3%.
TCM symptom index criteria
According to the "Guiding Principles for Clinical Research of New Chinese Medicines"20and "Guidelines for the Diagnosis and Treatment of Common Gynecological Diseases in Traditional Chinese Medicine"19issued by the Ministry of Health of the People's Republic of China,the efficacy criteria for the treatment of kidney deficiency and phlegm-dampness,"irregular menstruation","amenorrhea",and "infertility",are used to establish the quantification of the symptom pattern points table for evaluation.The score and TCM symptoms are positively related.
BBT biphasic body temperature assessment criteria
BBT was determined as follows:the measurement time of basal body temperature was fixed at 5-7 o'clock every day,and patients tried to measure at the same time every day.After waking up every morning,patients took a thermometer and put it under the tongue,measured the temperature under the tongue for 5 min,and recorded the body temperature.
Classification criteria:(a) typical biphasic:the difference between high and low temperature was 0.3 to 0.6 ℃,and the body temperature increased for 12 to 14 d;(b)atypical biphasic:there was a low temperature during ovulation to the luteal phase,the temperature raised slowly,and this period was more than 3 d;the difference between high and low temperature was less than 0.2 ℃;the body temperature fluctuation in the high-temperature period was more than 0.1 ℃,and this period was less than 12 d;(c)single-phase:no fluctuation in body temperature.
Hormone levels assessment
Chemiluminescence Microparticle Immunoassay(CMIA):biochemical parameters,including E2,T,FSH,and luteotropic hormone (LH) levels,were analyzed using kits purchased from Ming Qing Biology Limited Company(Shanghai).All procedures were carried out according to the manufacturer's protocols.
Enzyme-linked immunosorbent assay (ELISA):the obtained peripheral blood samples were centrifuged at 3000×gand 4 ℃for 10 min;then,serum was extracted to evaluate AMH and P450arom levels using ELISA kits (Beinglay Biotechnology Co.Ltd.,Wuhan,China)according to the manufacturer's instructions.
Statistical analysis
IBM SPSS Statistics (Version 26.0,IBM Corp,Armonk,New York State,USA)software was used to analyze the data.The mean ± standard deviation (±s)was used to measure the normal distribution,and the median (quartile) (QL-QU) was used to indicate a nonnormal distribution.Groupt-test was used to assess the difference between groups that were normally distributed.Pairedt-test was used to assess the difference before and after treatment.A non-parameter test was used to assess data with a nonnormal distribution,and a rank-sum test was used for comparison between the grade data groups.Values ofP<0.05 were considered statistically significant.
RESULTS
Summary of patient flow diagram
In total,62 women with PCOS were allocated randomly to receive treatment,and there was one case lost during treatment in each group(1 case because of pregnancy and 1 case because of hospitalization for sudden illness),and finally,60 subjects were included);therefore,data from 60 women with PCOS were analyzed (Figure 2).

Figure 2 Summary of patient flow diagram
Comparison of Baseline data of the two groups
A total of 62 subjects were enrolled,and the trial was discontinued in 2 cases (1 case discontinued treatment during pregnancy,1 case discontinued treatment due to sudden illness),and finally a total of 60 subjects were enrolled.There were 30 cases in the intervention group,the oldest was 40 years old,the youngest was 17 years old,and the average age was (27 ± 5) years old.There were 30 cases in the control group,the oldest was 41 years old,the youngest was 20 years old,and the average age was (30 ± 6) years old.The average course of disease in the intervention group is (6 ± 4)years,and the average course of disease in the control group is(6±5)years.There was no statistically significant difference in the age and course of disease between the two groups(P>0.05).
Comparisons of E2,T,LH,FSH,AMH and P450arom levels before and after treatment
To evaluate whether electroacupuncture significantly regulated hormone levels in PCOS patients.Compared to pretreatment,the E2 and P450arom levels of the intervention group were increased after treatment (allP <0.05),and the T,LH and AMH levels were decreased(PT<0.05,PLH<0.01,PAMH<0.01).There was no significant difference in the FSH level(P>0.05)of the intervention group before and after treatment.In the control group,the E2 level was increased (P <0.05),and LH level was decreased (P <0.05),and there was no statistically significant difference in T,FSH,AMH,and P450arom levels (allP >0.05).Before treatment,there was no significant difference between the intervention and control groups (P >0.05).After treatment,the T,LH,and AMH levels in the intervention group were decreased,and the P450arom level was increased compared with those in the control group (bothP <0.05).There was no significant difference between E2 and FSH levels(allP>0.05;Table 1).
Comparison of the clinical efficacy of the two groups
Among the 30 cases in the intervention group,5 cases were cured,21 cases were effective and 4 cases were ineffective,with a total effective rate of 86.7 %.Of the 30 patients in the control group,13 cases were effective and 17 cases were ineffective,with a total effective rate of 43.3%.The clinical efficacy of the intervention group was better than that of the control group (P <0.01,Table 2).
Comparison of the total TCM symptom pattern score before and after treatment
According to the total TCM symptom pattern score,the average score of the intervention group before treatment was 25 ± 6,and after treatment it was 13 ± 4.The average score of the control group before treatment was 25 ± 6,and after treatment it was 21 ± 6.The intervention group was significantly lower than that before (P <0.01),the control group was also lower than that before (P <0.05),and the intervention group was significantly better than the control group(P<0.01).
Comparison of the TCM symptom pattern score before and after treatment
Before treatment,there was no statistical difference in the scores of TCM symptoms between the two groups of patients in the menstrual cycle,menstrual volume,menstrual quality,fatigue,waist and knee weakness,cold feeling in the lower abdomen,chest tightness,and greasy mouth and phlegm (allP >0.05).Compared with before treatment,the TCM symptoms scores of the menstrual cycle,menstrual volume,menstrual quality,fatigue,waist and knee weakness,cold feeling in the lower abdomen,chest tightness,and greasy mouth and phlegm in the intervention group were significantly reduced after treatment (allP <0.01),and that of the control group was also reduced after treatment(P<0.01,P<0.05).Compared with the control group,the TCM symptom scores of menstrual volume in the intervention group were significantly lower than those of the control group after treatment (P <0.01),and the TCM symptom scores of the menstrual cycle,menstrual quality,waist and knee weakness,chest tightness,and greasy mouth and phlegm in the intervention group were lower than those of the control group after treatment (allP <0.05),but there was no significant difference in the scores of TCM symptoms between the two groups of patients in fatigue,cold feeling in the lower abdomen after treatment (allP >0.05,Table 3).
Comparison of BBT before and after treatment
After treatment intervention group contained 10 cases of biphasic,16 cases of atypical biphasic,and 4 cases of monophasic BBT.The total effective rate was 86.7 %.In the control group,there were 5 cases of biphasic,9 cases of atypical biphasic,and 16 cases of monophasic BBT.The total effective rate is 46.7 %.The intervention group was significantly superior to the control group(P<0.05,Table 4).
Comparison of menstrual cycle of the two groups
After treatment,the intervention group contained 25 cases of regular menstrual cycle and 5 cases of the irregular menstrual cycle.The total effective rate was 83.3 %.In the control group,there were 13 cases of regular menstrual cycle and 17 cases of the irregular menstrual cycle.The total effective rate is 43.3 %.The intervention group was significantly superior to the control group(P<0.05,Table 5).

Table 1 E2,T,LH,FSH,AMH and P450arom levels before and after treatment

Table 2 Comparison of the clinical efficacy of the two groups
Table 3 TCM symptom pattern score before and after treatment(±s)
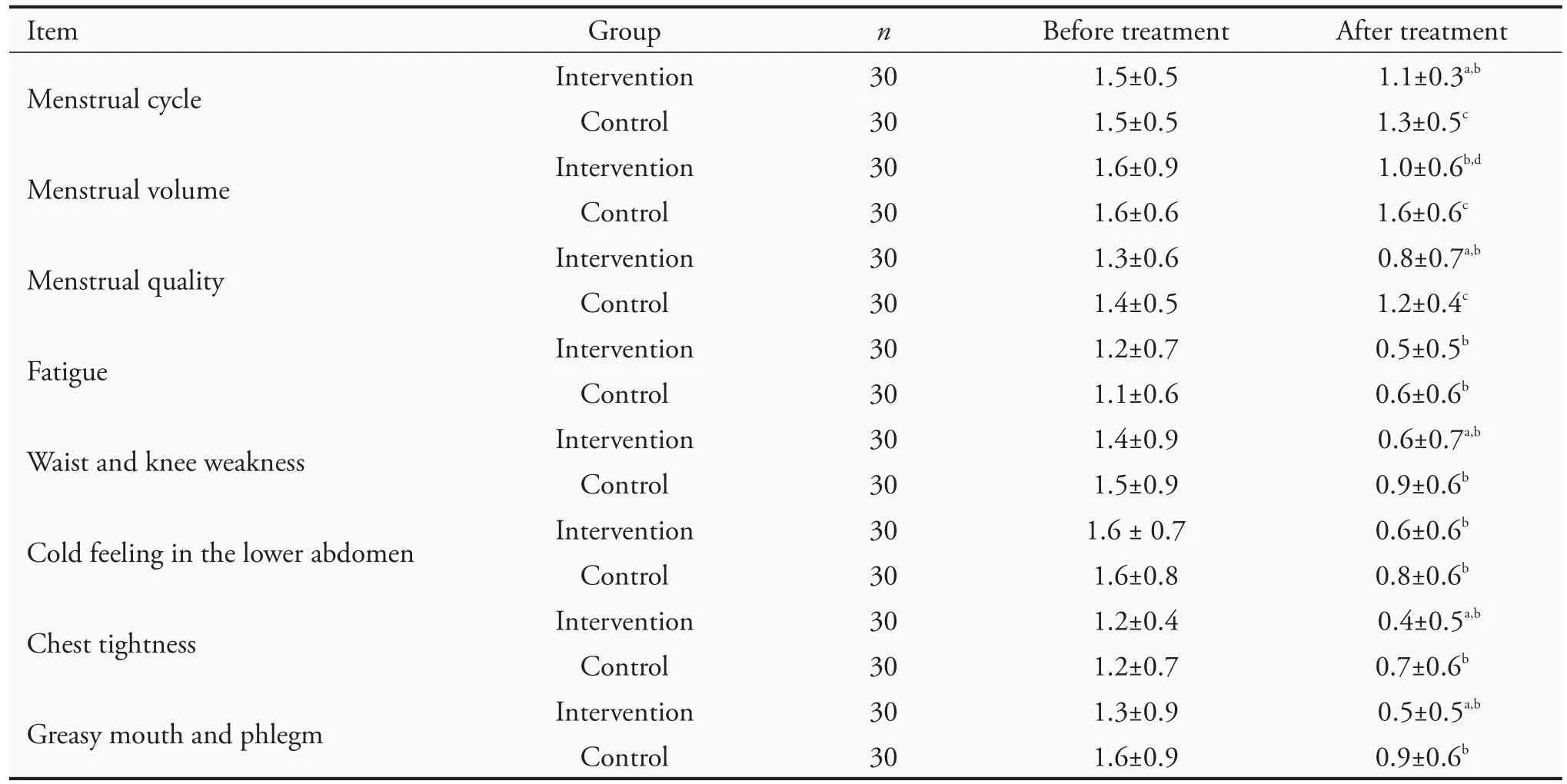
Table 3 TCM symptom pattern score before and after treatment(±s)
Notes:intervention group:acupoints were subjected to (43 ± 1) ℃herb-partitioned moxibustion and electroacupuncture treatment;control group:acupoints were subjected to(37±1)℃herb-partitioned moxibustion and sham electroacupuncture treatment.Compared with the control group,aP<0.05,dP<0.01;compared with this group before treatment,bP<0.01,cP<0.05.
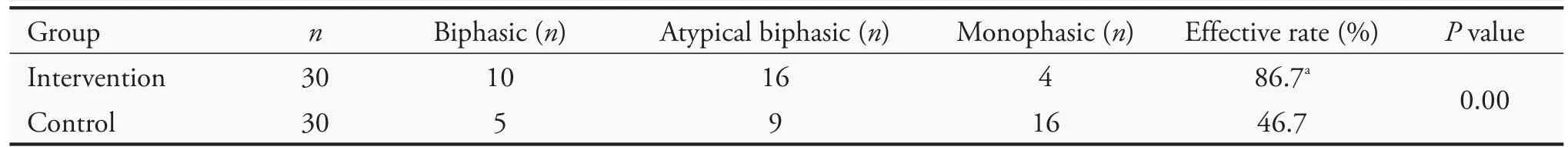
Table 4 Comparison of BBT before and after treatment

Table 5 Comparison of menstrual cycle of the two groups
Evaluation of safety
There were 2 adverse events in the clinical trial process in the intervention group.One patient was slightly scalded because the moxa stick fell at the Guanyuan(CV4) point,and then burn ointment was applied;the other patient was slightly scalded at the right uterine point,and burn ointment was applied;both patients completely recovered.There were no serious adverse events.
DISCUSSION
According to its clinical manifestations,PCOS can be attributed to "amenorrhea," "infertility," or "late menstruation" in TCM.PCOS patients often have kidney deficiency and phlegm-dampness constitutions.A deficiency of kidney essence makes it difficult for the ovum to develop.A deficiency of kidney Yang cannot warm spleen Yang,causing an obstructed circulation ofQiand blood and making water accumulate into phlegm.21Specifically,stagnation ofQi,blood,and phlegm-dampness in the Chong and conception vessels make it difficult for the ovum to be discharged,causing oligomenorrhea,amenorrhea,and infertility.In recent years,acupuncture and moxibustion have been indicated as an effective therapy in the treatment of PCOS.22-24Studies have shown that acupuncture can adjust the human endocrine function by stimulating the internal functions of the body's tissues and organs,thereby restoring the normal function of the ovary,producing menstruation and ovulation.25-27All the results of this study indicate that the clinical efficacy of the intervention group was better than that of the control group,suggesting herb-partitioned moxibustion combined with electroacupuncture treatment can significantly improve the symptoms of late menstruation,low menstrual volume,abnormal menstrual cycle,and reduce the symptoms of TCM.
Women with PCOS often experience irregular menstrual cycles.Generally,a normal cycle starts on the first day of menstruation and is followed by a preovulatory period that is referred to as the follicular phase.After ovulation,the cycle enters a postovulatory period,which is referred to as the luteal phase that lasts until the day before the next onset of menstruation.The length of the menstrual cycle exhibits significant variation,both within and among individuals.28The BBT reflects this biphasic aspect of the menstrual cycle:29BBT tends to be relatively low during the follicular phase (the hypothermic phase),and it increases by 0.3 to 0.5 ℃after the cycle enters the luteal phase(the hyperthermic phase).30In addition,women's BBT shows a periodic pattern that is associated with the menstrual cycle.31Therefore,BBT is an important proxy for studying menstrual cycles in PCOS women.The results of this study show that the intervention group is superior to the control group in improving BBT and menstrual cycles,suggesting that herb-partitioned moxibustion combined with electroacupuncture treatment can significantly improve ovulation abnormalities in PCOS patients.
Follicles go through five stages in development:primordial follicles,primary follicles,secondary follicles,antral follicles,and preovulatory follicles.The early development of primordial follicles and primary follicles is not affected by gonadotropins(FSH mainly)and ovarian hormones (E2 mainly),while the development of the secondary follicle and antral follicle stage is affected by FSH and estrogen.FSH can induce granulosa cell expression of P450arom,which turns androgens into estrogen,and FSH can also promote follicle development to form dominant follicles.32AMH is considered a negative regulator of follicle growth and development because it reduces the sensitivity of FSH in promoting follicle growth,thereby inhibiting the development of growing follicles.Previous research has reported that AMH and T levels of PCOS patients are positively correlated.Eldaret al33found that the serum expression of AMH in PCOS patients was significantly higher than it was in healthy women.
Acupuncture can affect PCOS by regulating the body's metabolic level and insulin sensitivity,affecting local environmental hormone disturbances in the ovary and uterus,and stimulating the ovary to restore normal ovulation function.15In addition,it also has a certain ability to regulate AMH levels in PCOS patients.34Previous work found that after stimulating Zhongji (CV3)and Guanyuan (CV4) acupoints in PCOS rat models by electroacupuncture,the expression of AMH in follicular granulosa cells was decreased and the expression of P450arom was increased,resulting in a decrease in T level and an increase in E2 levels.13,15Results in this study suggest that the intervention group was superior to the control group in decreasing T and LH levels,and indicate that herb-partitioned moxibustion combined with electroacupuncture treatment can significantly improve E2 lever,and decrease the levers of T and LH related sex hormone dysregulation in PCOS patients.In terms of the effect on the levels of AMH and P450arom,the AMH level of the intervention group decreased significantly after treatment,and the P450arom level increased.The intervention group was better than the control group at improving the levels of AMH and P450arom.
The herb-partitioned moxibustion combined with electroacupuncture treatment can effectively improve the clinical symptoms of the PCOS patients with kidney deficiency and phlegm-dampness.In addition,herb-partitioned moxibustion combined with electroacupuncture treatment can improve the abnormal levels of AMH and P450arom,and it can promote the activity of P450arom by reducing the AMH level to reintroduce FSH-dependent follicular development,which would improve follicular development in PCOS patients.Thus,these results provide clinical evidence for promoting the clinical application of acupuncture treatment in PCOS patients,which provide in-depth insight into the mechanism of acupuncture treatment in PCOS.
ACKNOWLEDGMENTS
We thank all participants for their trust and persistence.We are very thankful to all physicians,medical staff,and other contributors to this trial.
 Journal of Traditional Chinese Medicine2021年6期
Journal of Traditional Chinese Medicine2021年6期
- Journal of Traditional Chinese Medicine的其它文章
- In vivo anti-diarrheal activity of jujube honey on castor oil-induced diarrhea in mice
- Ethanolic extract of Puhuang (Pollen Typhae) modulates lipopolysaccharide-induced inflammatory response through inducible nitric oxide synthase/cyclooxygenase-2 signaling in RAW 264.7 macrophages
- Target prediction and activity verification for the antidepressant action of Huangqin(Radix Scutellariae Baicalensis)
- Pingchuan formula (平喘方) improves allergic asthma in mice through inhibiting nuclear factor-kappa B/mitogen-activated protein kinase signaling pathway
- Can Fig and Olive Ameliorate the toxicity Induced by 2-nitropropane in some organs of mice? role of inflammatory versus anti-inflammatory genes
- Efficacy of Renshen(Radix Ginseng)plus Fuzi(Radix Aconiti Lateralis Preparata)on myocardial infarction by enhancing autophagy in rats
