Neurons derived from human-induced pluripotent stem cells express mu and kappa opioid receptors
Zhi-Hai Ju, Xuan Liang, Yao-Yao Ren, Luo-Wa Shu, Yan-Hong Yan, Xu Cui
Abstract Neuroprotection studies have shown that induced pluripotent stem (iPS) cells have the possibility to transform neuroprotection research.In the present study, iPS cells were generated from human renal epithelial cells and were then differentiated into neurons. Cells in the iPScell group were maintained in stem cell medium. In contrast, cells in the iPS-neuron group were first maintained in neural induction medium and expansion medium containing ROCK inhibitors, and then cultivated in neuronal differentiation medium and neuronal maturation medium to induce the neural stem cells to differentiate into neurons. The expression of relevant markers was compared at different stages of differentiation. Immunofluorescence staining revealed that cells in the iPS-neuron group expressed the neural stem cell markers SOX1 and nestin on day 11 of induction, and neuronal markers TUBB3 and NeuN on day 21 of induction. Polymerase chain reaction results demonstrated that, compared with the iPS-cell group, TUBB3 gene expression in the iPS-neuron group was increased 15.6-fold. Further research revealed that, compared with the iPS-cell group, the gene expression and immunoreactivity of mu opioid receptor in the iPS-neuron group were significantly increased (38.3-fold and 5.7-fold, respectively), but those of kappa opioid receptor had only a slight change (1.33-fold and 1.57-fold increases, respectively). Together, these data indicate that human iPS cells can be induced into mu opioid receptor- and kappa opioid receptor-expressing neurons, and that they may be useful to simulate human opioid receptor function in vitro and explore the underlying mechanisms of human conditions.
Key Words: brain; cells; factor; in vivo; neural differentiation; protein; stem cells; stroke
Introduction
Cerebral ischemic/hypoxic injury is a common pathophysiological process in ischemic stroke (Yu et al., 2019; Bae et al.,2020). Reperfusion injury after thrombolytic therapy is accompanied by high morbidity and mortality, and can further aggravate brain injury. An effective treatment is currently lacking (Catanese et al., 2017). Recent studies have reported that opioid agonists can produce different degrees of neuroprotection (Chunhua et al., 2014; Meng et al., 2016;Gui et al., 2017). Morphine is a classic representative of mu opioid receptor (MOR) agonists that is commonly used in the clinic. It exerts neuroprotection through the PI3K/Akt signaling pathway, protein kinases C membrane translocation, and miR-134 expression (Liu et al., 2008; Zhou et al., 2011; Meng et al.,2016). Other non-opioid receptor agonists, such as Salvinorin A, reduce mortality and improve neurological developmental outcomes in neonatal mouse hypoxia models (Chen et al., 2014). Herkinorin, a semi-synthetic opioid receptor agonist, provides neuroprotection against cerebral ischemia/reperfusion injury in mice by inducing cPKCγ membrane translocation (Gui et al., 2017). Together, these findings suggest that opioid receptor activation plays an important role in neuroprotection (Dong et al., 2019; Sun et al., 2019).
The opioid system is involved in the modulation of various physiological and pathological responses, including antinociception, neuroprotection, behavior and memory regulation, drug addiction, thermosensation, respiratory depression, immunoreaction, and ion channel functions(Macey et al., 2010; Shapovalov et al., 2013; Liang et al.,2016; Roeckel et al., 2016; Darcq and Kieffer, 2018; Gupta et al., 2018; Melo et al., 2018; Pellissier et al., 2018). Hypoxiainduced and agonist-mediated opioid internalization can be inhibited by opioid antagonists (Hill and Walsh, 2005). Our previous study revealed that oxygen/glucose deprivation for 1 hour, which mimics hypoxia, induces reversible opioid internalization in murine Neuro-2A (N2A) cells (Xi et al., 2017).Cell and animal experiments have suggested that opioid activation has possible neuroprotective effects (Beevers et al.,2013; Eigentler et al., 2013).
Much of our understanding about the mechanisms governing brain development and function in primates comes from research using a few models that are relatively distantly related to humans. However, there are many species differences in the proportions of opioid subtype binding sites in the mammalian brain. In the guinea pig brain, the proportion of opioid binding sites was reported as 24% mu, 32% delta, and 44% kappa. In rabbits, the proportions were 43% mu, 19%delta, and 37% kappa, while in rats, they were 51% mu, 29%delta, and 20% kappa (Robson et al., 1985). There are also many central nervous system differences between primates and rodents. Humans have detailed neuronal connections,with the immense complexity of the human connectome. The genetic and molecular mechanisms of human brain evolution are also very different from that of rodents (Hill and Walsh,2005; Rakic, 2009; Sousa et al., 2017). Experimental, ethical,and legal limitations have hindered research on the human brain. However, whether animal models can mimic human diseases is highly controversial (Drake, 2013).
The use of human-derived cells to investigate mechanisms of the disease may allow for the clinical transformation of relevant theories. The emergence of induced pluripotent stem(iPS) cells has injected vitality into the study of regenerative medicine, disease model establishment, and drug and toxicity screening (Lancaster et al., 2013; Kikuchi et al., 2017). Using human iPS cells to establish a model to explore human diseases allows both the identification of disease mechanisms and the performance of drug screening. Few studies have investigated the neuroprotective mechanisms of human iPSderived differentiated neural cells (De Filippis et al., 2016).In a previous study, we successfully constructed iPS cell lines using human urinary exfoliated epithelial cells (Wang et al.,2016; Ju et al., 2017). Here, we aimed to induce neuronal differentiation of human iPS cells and to detect whether these neurons express opioid receptors, which will be important for subsequent studies of human opioid function.
Materials and Methods
Cells
We used human urine-derived iPS cells reprogrammed through an episomal system, which were generated in Beijing Cellapy Biotechnology Co., Ltd., as detailed in our previous reports (Wang et al., 2016; Ju et al., 2017). All six donors in the study signed a consent form that was available as a requirement for human studies. The undifferentiated iPS cells were cultured for further study in Essential 8TMMedium(A1517001, Thermo Fisher, Waltham, MA, USA) at a density of 10,000 cells/cm2with 5% CO2at 37°C.
Differentiation of iPS cells into neural stem cells
For the iPS-cell group, the cells were maintained in Essential 8TMMedium (A1517001; Thermo Fisher) to maintain an undifferentiated state. For the iPS-neuron group, the iPS cells were digested with accutase when their confluence was approximately 85%. After centrifugation, the cells were resuspended in neural induction medium (05835; Stemcell,Vancouver, Canada) and the ROCK inhibitor Y27632 was added(Y0503; Sigma, St. Louis, MO, USA). The cells were then plated at a density of 4–5 × 106onto AggreWell (Stemcell, Shanghai,China), centrifuged, and incubated. For the next 4 days, the cultivating medium was half exchanged every day. On day 5,the spheres on AggreWell were attached to the cell culture plate and neural induction medium (05835; Stemcell) was added to start the induction process, with a medium change every 2 days. On day 11, rosettes were chosen to plate, and these were continued to be cultured in the neural stem cell expansion medium (iNM-001; CIB, Shenzhen, China). This step was repeated if necessary. When the rosettes were sufficiently amplified, they were digested with accutase and dispase to obtain neural stem cells (NSCs), and were then plated with neural stem cell expansion medium (iNM-001; CIB) for further amplification.
Differentiation of NSCs into neurons
The cells in the iPS-cell group were continuously maintained in an undifferentiated state using Essential 8TMMedium. In the iPS-neuron group, when the NSCs reached a confluence of approximately 100%, they were digested using accutase.After centrifugation, the cells were resuspended in neuronal differentiation medium (08500; Stemcell) and seeded onto the plate, and the medium was replaced every 2 days for the next week. On day 8, cells were digested with accutase,centrifuged, and resuspended in neuronal maturation medium (iNM-007A, CIB) to begin the maturation process.The medium was replaced every 2 days. On day 21, cells were fixed for immunofluorescence.
Immunofluorescence
Cells were fixed with 4% paraformaldehyde for 20 minutes at room temperature and then washed with phosphatebuffered saline (PBS). Next, cells were treated with a blocking solution, comprising PBS containing 3% bovine serum albumin, and were then permeabilized with 0.3% Triton X-100 for 30 minutes at room temperature. The following primary antibodies (Abcam, Cambridgeshire, UK) were diluted in blocking solution and incubated at 4°C overnight: anti-Oct4 (mouse anti-Oct4 monoclonal antibody, ab184665;1:1000), anti-SOX1 (rabbit anti-SOX1 polyclonal antibody,ab87775; 1:500), anti-nestin (rabbit anti-nestin polyclonal antibody, ab92391; 1:250), anti-OPRK1 (rabbit anti-ku opiod receptor [KOR] polyclonal antibody, ab113533; 1:1000), anti-OPRM1 (rabbit anti-MOR polyclonal antibody, ab10275;1:1000), anti-TUBB3 (mouse anti-beta III tubulin monoclonal antibody, ab78078; 1:1000), and anti-NeuN (rabbit anti-NeuN polyclonal antibody, ab104225; 1:500). After washing with PBS, secondary antibodies were added and incubated at room temperature in a dark box for 1 hour. Alexa Fluor 488-labeled goat anti-rabbit IgG (H + L) (A0423; 1:500), Alexa Fluor 488-labeled goat anti-mouse IgG (H + L), and Cy3-labeled goat anti-rabbit IgG (H + L) (A0516; 1:500) were purchased from Beyotime (Shanghai, China). Nuclei were labeled with 4′,6-diamidino-2-phenylindole (DAPI; C1005; Beyotime). Mean fluorescence intensity (i.e., integrated density/area) was calculated using ImageJ 1.52q software (National Institutes of Health, Bethesda, MD, USA) according to the software instructions. At least 50 cells from three separate experiments were counted.
Quantitative polymerase chain reaction analysis
The primers used for the polymerase chain reaction (PCR)reaction system are listed in Table 1. The PCR conditions were 95°C for 60 seconds followed by 40 cycles of 95°C for 5 seconds and 60°C for 34 seconds. Melting curves were obtained for each of the genes. PCR was performed on an ABI PCR system (ABI 7500; Applied Biosystems, Foster City, CA,USA). The average cycle threshold (Ct) values of tested genes were calculated against average glyceraldehyde 3-phosphate dehydrogenase (GAPDH) Ct values from the same sample.∆Ct = Ct (tested gene) – Ct (GAPDH), and ∆∆Ct = ∆Ct (iPSneuron group) – ∆Ct (iPS-cell group). The fold changes of gene transcript levels of MOR, KOR, MAP2, and TUBB3 between the two groups were calculated as 2–∆∆Ct(Wang et al., 2016).

Table 1 |Primers used for qPCR
Statistical analysis
Results are given as the mean ± SD. Data were analyzed using SPSS 22.0 software (IBM Corp., Armonk, NY, USA) and the unpaired Student’st-test was used for data analysis. All histograms were plotted using GraphPad Prism 7 software(version 7.0a, San Diego, CA, USA).P< 0.05 was considered statistically significant.
Results
Culture of human urine-derived iPS cells
The iPS cells cultured in stem cell medium had a high nucleusto-cytoplasm ratio and tightly packed colonies with defined borders (Figure 1). Immunofluorescence staining confirmed expression of the human pluripotency-associated marker Oct4, and karyotype analysis of iPS cells in our previous report (Wang et al., 2016) revealed a normal karyotype of 24 chromosomes.
Generation of NSCs from iPS cells
To derive early-stage NSCs from iPS cells, we differentiated iPS cells into NSCs using a monolayer culture protocol.Differentiation was carried out in a defined, serum-free medium for the neural induction of iPS cells by blocking TGF-β/BMPdependent SMAD signaling. Immunofluorescence revealed the presence of early-stage NSC markers nestin and SOX1 in the iPS-neuron group (Figure 2), suggesting that the iPS-derived compact colony-forming cells were early-stage NSCs.
Generation of neurons from iPS cell-derived NSCs
NSCs are multipotent and can differentiate into three neural subtypes: neurons, oligodendrocytes, and astrocytes. Here, we investigated the potential of NSC to differentiate into neurons.Single-cell-dissociated NSCs were seeded onto AggreWell in neuronal differentiation medium for 3 weeks. qPCR and immunofluorescence were used to confirm the differentiation of NSCs. qPCR analysis revealed thatTUBB3gene levels were upregulated. Immunofluorescence confirmed the PCR result,with cells observed to be immunoreactive for TUBB3. NeuN staining showed the cellular features of the neurons (Figure 3).
iPS cell-derived neurons express MOR and KOR
Several lines of evidence suggest that opioid receptor internalization may be important for regulating neural function,whether in a physiological or non-physiological environment.We thus also tested whether our differentiated neurons expressed opioid receptors. Indeed, MOR and KOR expression was detected in both iPS cells and iPS cell-derived neurons.The immunoreactivity of MOR and KOR in iPS cells and iPS cellderived neurons was calculated as the mean fluorescence intensity. Compared with the iPS-cell group, in the iPS-neuron group there was a 5.7-fold increase in mean fluorescence intensity of MOR and a 1.57-fold increase in KOR (Figure 4).MAP2, a neuron-specific protein that was used as a control, was upregulated 101.2-fold in iPS cell-derived neurons. Furthermore,transcription of both MOR and KOR was upregulated when the iPS cells differentiated into neurons (MOR: 38.3-fold, KOR: 1.33-fold, compared with iPS cells) (Figure 5).
Discussion
In the present study, we demonstrated that human iPS cellderived neurons express opioid receptors, including KOR and MOR. With the differentiation of iPS cells into neurons, both the gene expression and immunoreactivity of MOR were markedly increased, whereas KOR was only slightly increased.Our results suggest that iPS cell-derived neurons may be an ideal candidate for studying human opioid receptor function.
Opioid receptors belong to the G-protein coupled receptor family, which constitutes the most abundant receptor class in the human genome (Fredriksson et al., 2003; Darcq and Kieffer, 2018). G-protein coupled receptors regulate a variety of biological functions, and are the receptor class most commonly targeted by pharmacological therapies. Receptor activation is often accompanied by receptor internalization,which is a complex regulatory process that terminates receptor cell surface signaling and can also elicit different intracellular signaling cascades (Pavlos and Friedman, 2017).MOR internalization plays a role in the signaling that mediates antinociception, as well as in the regulation of morphological changes in the dendritic spine effects of opioids (Liao et al.,2007; Macey et al., 2010). We previously used anin vitromodel of oxygen/glucose deprivation and reoxygenation to explore how KOR responds to hypoxia and reoxygenation. The results indicated that, in neuroblastoma cells, hypoxia induces reversible KOR internalization, which is inhibited by selective KOR antagonists or dynamin inhibitors and reversed by reoxygenation (Xi et al., 2017). A previous study reported that,because of different phosphorylation sites in the KOR receptor,there are species differences between humans and mice in the functional selectivity of different KOR receptor agonists to activate G proteins and internalize the receptors (Di Mattio et al., 2015). However, the studies by both DiMattio et al. and ourselves were performed in transfected cell systems, which do not adequately mimic normal physiological environments(Di Mattio et al., 2015; Xie et al., 2017).
The lack of a scalable, robust, and physiologically relevant model of human neurons has hindered the study of opioid receptor functions in health and disease. However, iPS cells can be derived from diseased or disease-free subjects,and iPS cell-derived neurons from patients with genetically inherited neurological disorders can be used to study disease mechanisms (Lippmann et al., 2012; Abud et al., 2017;Georges et al., 2019; Vatine et al., 2019). Researchers found that a 3′ polymorphism with a variable number of tandem repeats (VNTR) affected human dopamine transporter expression levels in iPS cell-derived human dopaminergic neurons (Sheng et al., 2016). Another study demonstrated that human iPS cell-derived dopaminergic progenitor cells survived and functioned as midbrain dopaminergic neurons in a primate model of Parkinson’s disease (Kikuchi et al., 2017).Furthermore, Grossert et al. (2019) investigated the molecular mechanisms of ketamine treatment at clinically relevant concentrations by establishing anin vitromodel based on human iPS cell-derived neural progenitor cells. These authors found that ketamine increased the proliferation of those cells via insulin-like growth factor 2, independent of N-methyl-Daspartate receptors (Grossert et al., 2019).

Figure 1 |Morphology and characterization of iPS cells cultured for 5 days.

Figure 2 | NSCs derived from iPS cells cultured for 11 days.

Figure 3 |Expression of TUBB3 and NeuN in iPS cell-derived neurons differentiated from NSCs after 21 days of culture.

Figure 4 | Immunoreactivity of KOR and MOR in iPS cells and iPS cell-derived neurons.

Figure 5 | Gene expression levels of KOR and MOR in iPS cells and iPS cell-derived neurons.
Studies on cellular reprogramming, such as those involving iPS cells, can potentially eliminate the need for embryo-derived pluripotent cells, providing more detailed insights into human development and diseases while simultaneously surpassing ethical constraints. Furthermore, iPS cell-derived neurons reflect the individual and are thus closer to clinical practice.We reprogrammed urinary exfoliated renal epithelial cells to produce human iPS cells, based on our previous study, and successfully obtained non-integrating human iPS cells using the episomal system to deliver transcription factors (Ju et al., 2017). A non-integrating iPS cell without exogenous gene interference ensures that any neurons derived from it are adequately physiological, for mechanical studies. Our results confirmed that human iPS cells are readily available and can be used to generate iPS cell-derived neurons, which express KOR and MOR. Patient-derived iPS cells can model phenotypic diseases in neurons in which the genetic components of the disease are captured (Rowe and Daley, 2019). However, to the best of our knowledge, there have been no reports of pilot studies of opioid receptor internalization using human iPS cell-derived neural cells, and no studies investigating whether human iPS cell-derived neurons express opioid receptors.Here, we report the establishment of human iPS cell-derived neurons that express KOR and MOR.
Furthermore, gene expression and immunoreactivity of KOR and MOR were detected in both iPS cells and iPS cell-derived neurons in the present study. As the iPS cells differentiated into neurons, both the gene expression and immunoreactivity of MOR gradually increased. However, KOR had only slight increases in both mRNA levels and immunoreactivity. This increased expression of MOR indicates that it may be more important than KOR for neuronal differentiation. Our results revealed that, compared with MOR immunoreactivity,MOR mRNA levels were more elevated. Post-transcriptional and post-translational regulation, mRNA and protein degradation, modifications such as folding, and other factors may lead to inconsistencies between mRNA abundance and immunoreactivity. Moreover, the expression levels of many genes change over time, and this was confirmed in our study. Kim et al. (2006) reported that both MOR and KOR are necessary to induce embryonic stem cells (ESCs) to differentiate into neural progenitors. These authors detected MOR and KOR expression and immunoreactivity in both ESCs and retinoic acid-induced ESC-derived, nestin-positive neural progenitors. Both opioids promoted the limited proliferation of undifferentiated ESCs via the ERK/MAP kinase signaling pathway. Additionally, MOR- and KOR-selective agonists diverted ESCs from self-renewal and coaxed the cells to differentiate. In another study, opioid gene expression in P19 cells, a line of pluripotent murine ESCs, triggered the formation of myocardial cellsin vitro(Ventura and Maioli,2000). Our results demonstrated that both iPS cells and iPS cell-derived neurons have relatively high levels of MOR and KOR transcription and translation. However, we were unable to find relevant studies comparing the expression of opioid receptors between human primary neurons and iPS cellderived neurons. This may be because of ethical constraints.
The focus of translational medicine should be closer to human conditions, rather than relying solely on animal models to study human diseases (De Filippis et al., 2016). Therefore,using human iPS cells to establish a model for studying human diseases may be an effective approach that can both identify disease mechanisms and allow drug screening. Previously,we established neurons derived from iPS cells that were reprogrammed from urinary exfoliated renal epithelial cells;in the present study, we demonstrated that these iPS cellderived neurons express KOR and MOR. Taken together, our data support the feasibility of using iPS cell-derived neurons to investigate the role of opioid internalization in neuroprotection and to explore other opioid receptor functions in a humanderived model.
There are some shortcomings in our research. First, we only detected the expression of KOR and MOR because there have been more studies on the function of these two receptors, and they may have greater clinical significance.Second, although opioid receptor internalization plays a vital role in neuroprotection, we did not investigate whether physiological or non-physiological stimuli cause KOR and MOR internalization in iPS cell-derived neural cells. This will be the focus of our next study.Collectively, we successfully established human iPS cellderived neurons that express KOR and MOR, which is very conducive to the transformation of basic research theory into clinical practice. The development of iPS cell-derived neurons has expanded the scope of human research. More in-depth studies into opioid receptors in this cell model are expected to follow, which will provide more information about these receptors in humans.
Acknowledgments:We thank all the students and staffs of Department of Anesthesiology, Beijing Tongren Hospital, Capital Medical University,China for the constructive advice of this study.
Author contributions:Experiment implementation, collection and analysis of the data, drafting of the manuscript: ZHJ; experiment implementation and data interpretation: XL; data interpretation and drafting of the manuscript: YYR, LWS and YHY; study concept, data interpretation and manuscript preparation: XC. All authors approved the final version of the manuscript.
Conflicts of interest:The authors declare that there are no conflicts of interest associated with this manuscript.
Financial support:This work was supported by the National Natural Science Foundation of China, No. 81301065 (to XC); the Talent Training Plan of Beijing, No. D003034000031 (to XC). The funding sources had no role in study conception and design, data analysis or interpretation, paper writing or deciding to submit this paper for publication.
Institutional review board statement:The iPS cell line used in this study was available from a commercial organization. Our present experiment does not involve animals and humans, so it is free from ethics. All six donors in the study signed a consent form that was available as a requirement for human study.
Copyright license agreement:The Copyright License Agreement has been signed by all authors before publication.
Data sharing statement:Datasets analyzed during the current study are available from the corresponding author on reasonable request.
Plagiarism check:Checked twice by iThenticate.
Peer review:Externally peer reviewed.
Open access statement:This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix,tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
Open peer reviewer:Shyam Gajavelli, University of Miami Miller School of Medicine, USA.
Additional file:Open peer review report 1.
- 中国神经再生研究(英文版)的其它文章
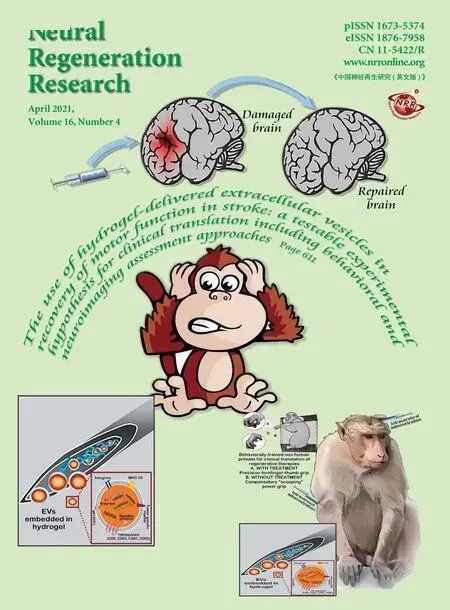
- The use of hydrogel-delivered extracellular vesicles in recovery of motor function in stroke: a testable experimental hypothesis for clinical translation including behavioral and neuroimaging assessment approaches
- Advances in human stem cell therapies: pre-clinical studies and the outlook for central nervous system regeneration
- MicroRNAs in laser-induced choroidal neovascularization in mice and rats: their expression and potential therapeutic targets
- The emerging role of probiotics in neurodegenerative diseases: new hope for Parkinson’s disease?
- The phenotypic convergence between microglia and peripheral macrophages during development and neuroinflammation paves the way for new therapeutic perspectives
- Modeling subcortical ischemic white matter injury in rodents: unmet need for a breakthrough in translational research