On-treatment isolated superior ophthalmic vein thrombosis complicated with carotid cavernous fistula: a case report
Yee Lin Lo, Kah Wei Ong, Teck Chee Cheng, Wan Haslina Wan Abdul Halim, Meng Hsien Yong
Department of Ophthalmology, Faculty of Medicine, Universiti Kebangsaan Malaysia, Kuala Lumpur 56000, Malaysia
Dear Editor,
We are writing this letter to present a case of ontreatment isolated superior ophthalmic vein thrombosis(SOVT) that progressed to cavernous sinus thrombosis(CST) and further complicated with carotid cavernous fistula(CCF). SOVT is a rare but potentially lethal illness. It is normally presented with orbital congestion syndrome with proptosis, ophthalmoplegia, diplopia, and high intraocular pressure (IOP)[1]. Late detection of this disease can lead to devastating complications such as optic nerve compression,CST and subsequently CCF. Case reports regarding SOVT are scarce thus there are limited management guidelines available. We present a case of SOVT which was complicated with CCF despite prompt medical treatment being given, but subsequently resolved with an added-on surgical intervention.Principles outlined in the Declaration of Helsinki was followed. Informed consent was obtained from the subject.
Case PresentationA 72-year-old lady with no known medical illness presented with sudden onset of double vision associated with unilateral left eye (OS) blurring of vision, redness, eyelid drooping, and eyeball protrusion (Figure 1). Her vision was 6/24 OS and 6/9 right eye (OD). There was a positive relative afferent pupillary defect (RAPD) OS. Ocular examination OS showed diffuse conjunctival congestion and chemosis with clear cornea and quiet anterior chamber. The IOP was 32 mm Hg. The fundus examination showed hyperaemic optic disc but otherwise normal. Her OD examination was normal. Exophthalmometry revealed 7 mm proptosis OS(15 mm OD, 22 mm OS). Extraocular muscles (EOMs)examination showed near-total external ophthalmoplegia(Figure 2). There was no palpable thrill or bruit. All cranial nerves examinations were normal except those mentioned.She was afebrile and there was no evidence of active infection elsewhere.
Her inflammatory markers [white blood cell 5.5×109/L,erythorcyte sedimentation rate (ESR) 10 mm/h, C-reactive protein (CRP) 0.10 mg/dL] were not raised. Further blood tests were negative for autoimmune and malignant diseases with normal thyroid profile, rheumatoid factor, antineutrophil cytoplasmic antibody (ANCA), and tumor markers. However,coagulopathy screening was not done.
Magnetic resonance imaging (MRI) of brain and orbit with venogram/angiogram (MRV/MRA) revealed distended left superior ophthalmic vein up to 6 mm in diameter with filling defect extended from the left orbital apex to the sclera, in keeping with SOVT (Figures 3 and 4). They were associated with inflammatory enhancement of the adjacent intra- and extra-conal fat plane and EOMs (mainly superior rectus and lateral rectus). Otherwise, no collection noted to suggest abscess. There was no evidence of CST or CCF on the MRV/MRA. The brain scan showed multiple subacute and chronic ischaemic changes due to mild intracranial atherosclerotic disease with no evidence of thrombosis. There were bilateral frontal, ethmoidal and maxillary sinuses mucosal thickening to suggest mild sinusitis.
The diagnosis of left acute isolated SOVT was made and the patient was referred and co-managed with the hematologist.She was treated with intravenous methylprednisolone 1 g for three days followed by a tapering dose of oral prednisolone.Oral anticoagulant Rivaroxaban 15 mg twice a day was commenced concurrently. Besides, she was prescribed antiglaucoma medications to control her IOP.
Despite early prompt treatment, her left eye deteriorated after one week with worsening of the orbital congestion,ophthalmoplegia, and raised IOP. MRV/MRA was repeated and revealed an indirect left CCF and evidence of CST.The endovascular procedure with proximal thrombosis embolization was performed by an interventional radiologist.The procedure successfully decreased her venous pressure and reversed her orbital congestion. The tapering dose of oral prednisolone was completed in 6wk duration, and oral anticoagulant was continued for 3mo.
Aside from residual positive RAPD, her other optic nerve function tests, IOP, and EOMs movement were all normalized within three months after the endovascular procedure(Figure 5). She can carry out her routine schedule and will be coming back for follow-up with surveillance MRI.
DISCUSSION
SOVT is a rare medical condition but often presented initially in the primary or emergency care settings[2]. It is a multifactorial disorder predisposed by alteration of Virchow’s triad (stasis of blood flow, endothelial dysfunction, and coagulopathy)[1]. The classical triad of clinical features consists of conjunctival chemosis, proptosis and cranial bruits. Other suggestive signs include blood in Schlemm’s canal, high IOP,and retinal haemorrhage[3].
The aetiology can be divided into septic and aseptic causes.Septic causes include infection from the adjacent structurese.g., sino-orbital, dental, and other mid facial infection or distant infective embolie.g., bacterial endocarditis. Aseptic causes include orbital inflammation, thyroid orbitopathy,trauma, vascular malformation, and neoplasm[4].
Laboratory investigations are important to differentiate the inflammatory or infective cause of thrombosis. These include septic screening, screening of autoimmune and connective tissues diseases[5]. Neoplasm is highly related to hypercoagulable condition thus, tumor markers test should be included as well. Anticoagulation drugs on the other hand may lead to false results in thrombophilia screening thus should be done only before the treatment or delayed till the treatment is completed[6].
The diagnosis of SOVT is based on clinical ground and confirmed by imaging studies. Neuroimaginge.g., computed tomography venogram (CTV) and MRV are both highly sensitive in early disease detection. MRV is superior in demonstrating patency of the cavernous sinus as compared to CTV[7]. SOVT can occur simultaneously with CST but can also be a separate entity[8]. In this case, repeated MRV demonstrated the subsequent involvement of CST and CCF as the complication of isolated SOVT.

Figure 1 Left eye chemosis, ptosis and proptosis on presentation.

Figure 2 Reduce ocular motility on the left eye with near-total external ophthalmoplegia.
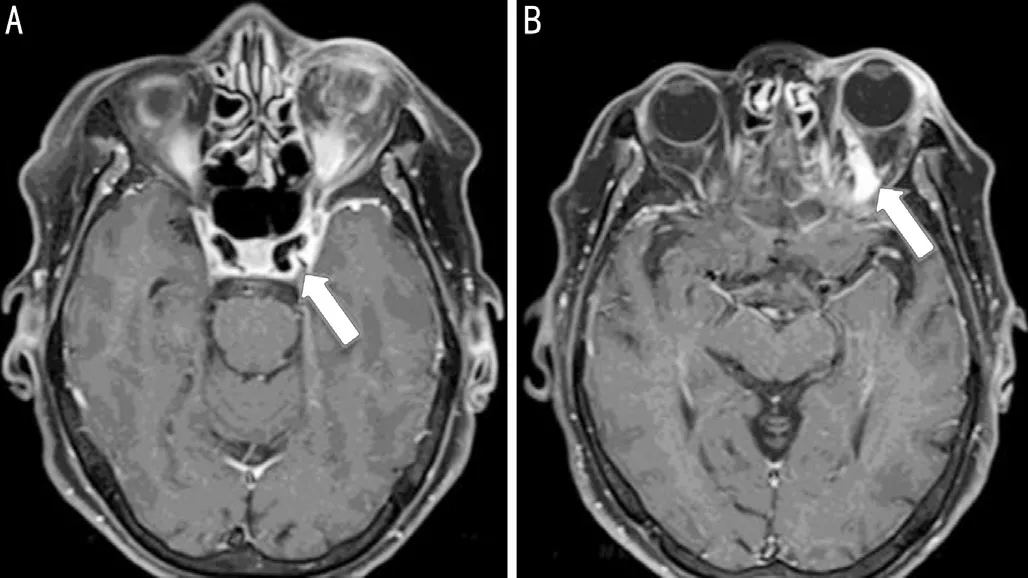
Figure 3 MRI T1 phase (axial) showing normal cavernous sinus(A, arrow) and dilated left superior ophthalmic vein (B, arrow).
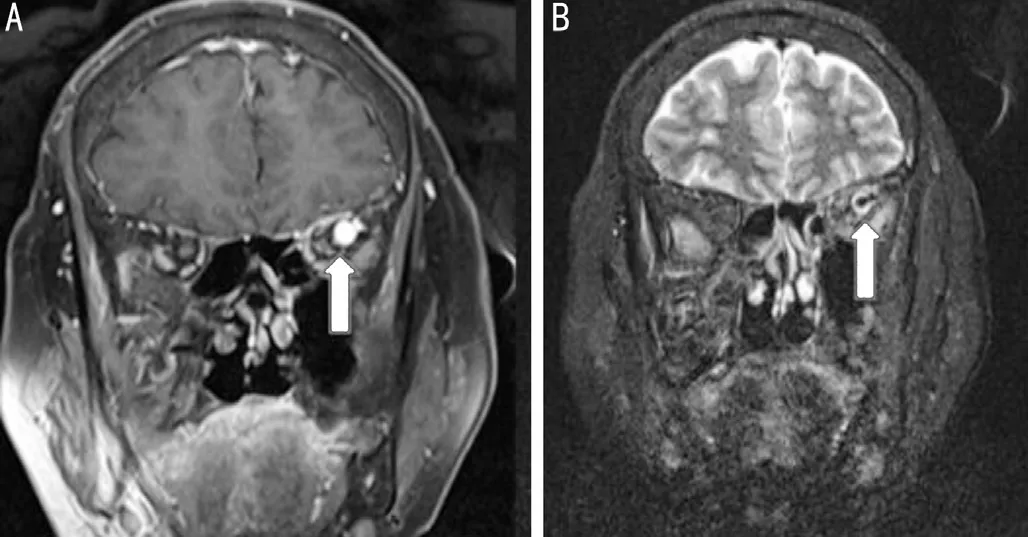
Figure 4 MRI T2 phase (coronal) showing dilated left superior ophthalmic vein (A, arrow) and filling defect (B, arrow).

Figure 5 Near-total resolution of proptosis, ptosis and chemosis of the left eye.
Given its rare occurrence, there is no standard guideline in the treatment of SOVT. Anticoagulant with intravenous heparin is recommended as initial therapy followed by oral anticoagulant.A randomized controlled trial recommended dose-adjusted intravenous heparin according to prothrombin time (PTT)by aiming to double the PTT but below 120s[9]. The optimal duration of oral anticoagulant therapy is currently unsure.However, based on a study by the European Federation of Neurological Societies (EFNS) a minimum of three months is recommended in cases secondary to transient risk factor;six to twelve months in a patient with an idiopathic cause or haematologic factors. Patients with the recurrent attack of thrombosis events should be on lifelong anticoagulants[10].This case was treated with oral anticoagulants solely from the beginning and complicated with CST/CCF. Intravenous heparin may be able to prevent the extension of the thrombosis faster with the faster onset of action and better monitoring markers[10]. The use of corticosteroid in non-infectious SOVT has no clear advantage but might be used to reduce inflammation and vasogenic oedema surrounding the ocular structures especially in the cases of optic nerve compression as in this case[11].
In conclusion, prompt diagnosis and early treatment with multidisciplinary approach are crucial to preserve the patient’s vision and to prevent the life-threatening complication in management strategy of cerebral vascular thrombosis or fistula. Improvement in the accessibility of MRV will help in the timely diagnosis of these conditions.
ACKNOWLEDGEMENTS
Conflicts of Interest:Lo YL,None;Ong KW,None;Cheng TC,None;Wan Abdul Halim WH,None;Yong MH,None.
 International Journal of Ophthalmology2022年10期
International Journal of Ophthalmology2022年10期
- International Journal of Ophthalmology的其它文章
- Lacrimal sac lymphoma: a case series and literature review
- Age-related changes of lens thickness and density in different age phases
- Therapeutic potential of pupilloplasty combined with phacomulsification and intraocular lens implantation against uveitis-induced cataract
- Prophylaxis with intraocular pressure lowering medication and glaucomatous progression in patients receiving intravitreal anti-VEGF therapy
- Optimal timing of preoperative intravitreal anti-VEGF injection for proliferative diabetic retinopathy patients
- Prognosis value of Chinese Ocular Fundus Diseases Society classification for proliferative diabetic retinopathy on postoperative visual acuity after pars plana vitrectomy in type 2 diabetes
