Macular vascularisation changes analysed using OCT angiography after successful rhegmatogenous retinal detachment repair
Marie Hartmann, Alaa Din Abdin, Doris Fraenkel, Christian Munteanu, Berthold Seitz, Shady Suffo
Department of Ophthalmology, Saarland University Medical Center, Homburg/Saar 66421, Germany
Abstract
● KEYWORDS: retina; vitrectomy; optical coherence tomography angiography
INTRODUCTION
Rhegmatogenous retinal detachment (RRD) is one of the most common ophthalmological emergencies requiring immediate surgery. A retinal tear causes vitreous fluid to escape into the subretinal space leading to a detachment of the neurosensory retina from the retinal pigment epithelium[1].Pars plana vitrectomy (PPV) is an established and effective procedure that is routinely performed in such cases[2]. At the end of the operation, a tamponade is performed, and different substances can be used, two of which are gas or silicone oil[3‐4].Silicone oil is used when a longer tamponade is needed,e.g.,in cases of proliferative vitreoretinopathy (PVR) stage C or more, in patients who need to fly during the weeks following surgery in cases of an inferior break at 6 o’clock[5‐6]or when the postoperative lying instructions could not be followed by the patients. However, it has a few disadvantages that must be taken into consideration. First, it requires a second operation,as it needs to be removed as opposed to gas, which evaporates.Furthermore, silicone oil is associated with more complications than gas, mainly corneal decompensation, band keratopathy,quick progression of a cataract and more exceptionally pupillary block glaucoma[7‐9].
Additionally, there seems to be another complication related to silicone oil causing profound acute visual loss without any anatomical explanation. Case series relating to this phenomenon have become more and more frequent: Janhnechtet al[10], Newsomet al[11], Cazabonet al[12], Satchiet al[13],Herbertet al[14], Williamset al[15], Todeet al[16], and Moyaetal[17]all reported profound unexplained visual loss following silicone oil removal. A few hypotheses were postulated: optic nerve damage due to direct tissue infiltration of silicone oil[12]and generalised macular dysfunction with lesions of retinal ganglion cells and horizontal‐bipolar cell synaptic processes in the outer plexiform layer[18‐19]. Christensen and la Cour[20]compared the macular optical coherence tomography (OCT)examination of patients after retinal detachment surgery using silicone oil and found a significant reduction of the inner retinal thickness and postulated a neuronal cell loss in the macular area as a possible explanation.
Rodríguezet al[21]analysed optical coherence tomography angiography (OCTA) after RRD sugery with PPV and found that the superficial macular perfusion and full retinal thickness decreased under silicone oil tamponade.
OCTA is a new non‐invasive tool allowing ophthalmologists to assess the vascular system of the macula without any dye injection[22]. Its use has been spreading for the evaluation of maculopathies such as diabetic maculopathy[23], retinal vein occlusion associated macular oedema[24]or macular degeneration[25]. Furthermore, its use has been proven helpful in detecting and following choroidal neovascularization[26].The two main parameters evaluated are the size of the foveal avascular zone (FAZ) and the parafoveolar vascular density(PVD) in both superficial and deep vascular networks. The FAZ is the region in the macula responsible for central vision.It has the highest concentration of cone photoreceptors and is entirely devoid of retinal capillaries. This zone can be measured using OCTA, and this measurement of the FAZ size is highly reproducible and provides quantitative information regarding the macula[27‐28]. FAZ size may vary in healthy eyes, but there seems to be a correlation between its size and the best‐corrected visual acuity (BCVA) in eyes with retinal diseases, shown in macular degeneration[29].
SUBJECTS AND METHODS
Ethical ApprovalThis retrospective, observational,comparative, single‐centre study followed the principles of the Declaration of Helsinki and was approved by the Ethic Committee of the University of Saarland (ethic motion number 293/20). Informed conscent was obtained from all the patients.Our work aimed to investigate the FAZ size and the PVD in the superficial capillary plexus in patients with RRD involvingvsnot involving the macula who underwent a PPV with gasvssilicone oil tamponade. Additionally, every patient underwent an OCT.
Study Design and SubjectsFor this study, a data collection was done retrospectively, including 77 eyes which had been diagnosed with a RRD with and without macular involvement and underwent a PPV with tamponade using either gas or silicone oil between January 2017 and October 2018 at the Department of Ophthalmology, Saarland University Medical Center in Homburg/Saar, Germany.
An analysis a priori was conducted with the Software G*Power (Erdfelder, Faul, Buchner, HHU Düsseldorf,Germany) to assess the number of patient necessary for the study with alpha=0.05 and power=0.80. The test determined that 64 patients had to be included in the group RRD with and 64 patients in the group RRD without macular involvement to achieve the desired power.
We only included patients with RRD without previous ocular surgery, except for a cataract operation, and without any ocular pathology such as epiretinal membrane, macular hole,glaucoma, macular degeneration, or retinal vascular disease.The patients incluRodríguezded all underwent one or two PPV.The preoperative examination included BCVA, intraocular pressure (IOP), axial length using optical or ultrasonic biometry, slit‐lamp, and dilated fundus examination. All patients were examined in the outpatient clinic of our Department between 6 and 24mo after the last PPV. The last PPV was either the retinal repair surgery with gas tamponade or the second PPV to extract silicone oil.
The BCVA and IOP were evaluated during this postoperative visit, and the slit‐lamp and dilated fundus examination were repeated. An OCTA (Zeiss Cirrus 5000 HD‐OCT, Zeiss Meditec Inc, Oberkochen, Germany) was also performed. We evaluated and compared the FAZ and PVD in the superficial capillary plexus in four groups using an OCTA. The OCTA examination was coupled with an OCT (Spectralis, Heidelberg Engineering, Germany), were we evaluated the central retinal thickness, the presence or absence of a macular oedema and the presence or absence of an epiretinal membrane in each group.
The four groups were as follows: Group 1: RRD with macular involvement treated with silicone oil tamponade; Group 2:RRD without macular involvement treated with silicone oil tamponade; Group 3: RRD with macular involvement treated with gas tamponade; Group 4: RRD without macular involvement treated with gas tamponade.
Surgical ProceduresAll patients were treated using a standard three‐port 23‐gauge PPV technique in either retrobulbar or general anesthesia. In eyes with cataracts, a standard cataract surgery was performed simultaneously.Three trocars were used for a vitrectomy performed with the EVA DORC system (Alcon, Fort Worth, Texas, USA).A fluid‐perfluorocarbon fluid exchange allowed subretinal fluid drainage from the causative retinal tear(s), followed by a retinopexy (photocoagulation or cryopexy). At completion of vitrectomy either 20% sulphur hexafluoride (SF6,n=30)or octafluoropropace (C3F8) (n=13) gas or silicon oil 2000(n=20) or 5700 centistoke (n=14) was injected into the vitreouschamber. All patients were hospitalised and stayed between 2 and 4d postoperatively. The silicone oil tamponade patients needed a second PPV to remove it. This second operation was performed between 6wk and 6mo after the first one. The average time between the first and second interventions was 17.4±10.2wk. The second operation followed the same steps as the first one, except that silicone oil was extracted.

Table 1 Patient’s characteristics n (%)
Optical Coherence Tomography Angiography AnalysisThe measurements were made using the CIRRUS TM OCT with AngioPlex technology from ZEISS, Oberkochen,Germany, which uses the optical microangiography algorithm.We acquired 6×6 mm2scans. En face images of the retinal vasculature were generated for the superficial capillary plexus,allowing the sizing of the FAZ as the area inside the capillary network’s central border and the measurement of the PVD in the superficial capillary plexus[30]. The images were read by an experience retinologist and checked for artifacts and segmentation errors.
Optical Coherence Tomography AnalysisWe measured the central retinal thickness and noted the presence or absence of cystoid macular oedema (CME) and epiretinal membrane.
Statistical AnalysisNormally distributed variables were reported as mean±standard deviation. We used a one‐way ANOVA test to compare the ages and axial lengths and combined it with post hoc Bonferroni corrections for FAZ size and PVD in all four groups. An independentt‐test was used to compare each group’s BCVA and ICF pre‐ and postoperatively.A Pearson Chi‐squared test allowed for comparing the groups regarding sex, lens status and presence of a preoperative vitreoretinopathy. Before performing data analyses, all BCVA measurements were converted to the logarithm of the minimum angle of resolution (logMAR) scale. Spearman’s correlation analyses examined the relationships between superficial FAZ areas and postoperative BCVA. The data were assembled and analysed using SSPS Software version 20.0 for Windows (SSPS Inc., Chicago, IL, USA). AP‐value<0.05 was considered to indicate a statistically significant difference.
RESULTS
Patients’ CharacteristicsTotally 77 eyes from 70 patients were distributed in 4 groups. The mean age was 60.4±16.3y.The patients’ characteristics are detailed in Table 1.
In group 1, 6 eyes presented with a PVR Stadium C and one Stadium D. In group 2, the patient presented a PVR Stadium C.
A one‐way ANOVA test showed no statistically significant difference between the four groups regarding age and axial length (P=0.75 andP=0.36, respectively). A Pearson Chi‐squared test showed that the four groups were comparable regarding sex and lens status (P=0.60,P=0.44, respectively). The preoperative presence or absence of PVR was also documented,and a Pearson Chi‐square test showed no significant association between the presence or absence of a PVR in any group (P=0.24).Moreover, the median duration of the macular detachment was 3 (0‐8)d in group 1, 2 patients could not say when they started to see so poorly, and 1d (0‐1.25) in group 3.
Best-corrected Visual Acuity and Intraocular PressureAn independent samplest‐test was conducted to compare pre‐and postoperative BCVA in all four groups. It showed that the postoperative BCVA was statistically significantly better than the preoperative BCVA in three groups:P<0.01 in group 1,P=0.02 in group 3 andP=0.04 in group 4. There was no significant difference between the pre‐ and postoperative IOP in all four groups. The pre‐ and postoperative BCVA and IOP results are detailed in Table 2.
Optical Coherence Tomography Angiography ResultsThe mean results from the OCTA analysis are detailed in Table 3, and the FAZ sizes for every patient are shown in Figure 1. A one‐way ANOVA test showed that the FAZ size was statistically significantly larger in eyes with RRD involving the macula than in those not involving itP=0.005. However, there was no statistically significant difference in the FAZ sizes of the eyes treated with silicone oil tamponade compared to those treated with gas tamponade,P=0.54. Regarding the PVD, there was no statistically significant difference between the groups treated with silicon oilvsgas (P=0.31) nor between the groups with RRD withvswithout macular detachment(P=0.16).A Pearson correlation analysis showed a significant positive correlation between postoperative BCVA and FAZ size in the superficial capillary plexus for all groups combined,P=0.01(Figure 1).
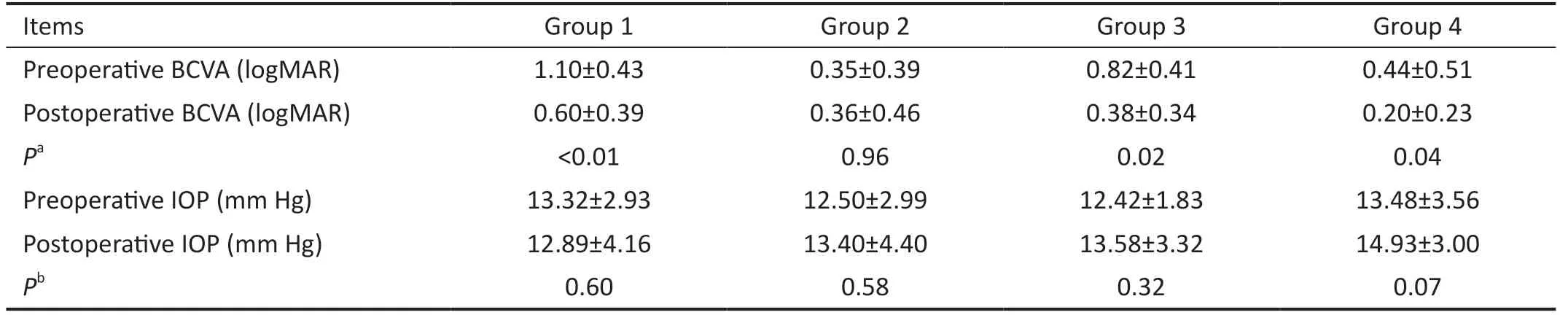
Table 2 Pre- and postoperative BCVA and IOP
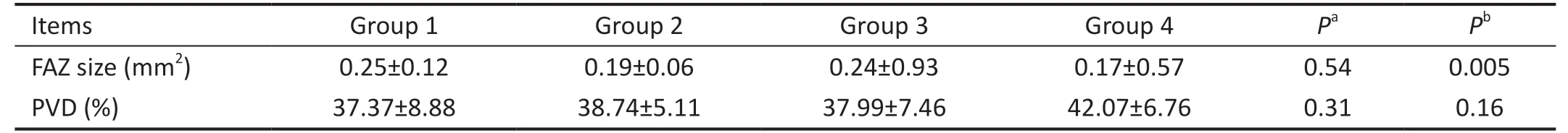
Table 3 Mean OCTA results
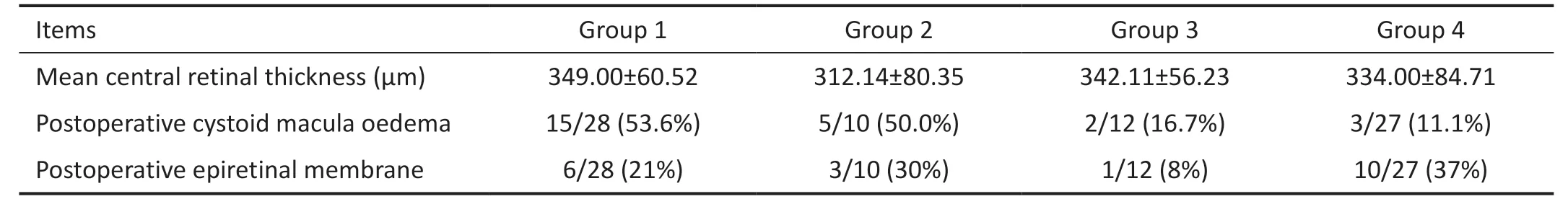
Table 4 Mean OCT results
A one‐way ANOVA test showed no statistically significant difference between PVD in the superficial capillary plexus in patients treated with gas versus silicone oil (P=0.31) or in RRD withvswithout macular involvement (P=0.16).
Optical Coherence Tomography ResultsThe mean OCT results are detailed in Table 4.
In all four groups, we performed a one‐way ANOVA‐test to evaluate the mean central retina thickness. There was no statistically significant difference between the groups treated with gasvssilicone oil (P=0.68) nor in the groups with RRD withvswithout macular detachment (P=0.26). There also was no statistically significant difference in any of the subgroup.
A Pearson Chi‐squared test showed a significant association between the presence of postoperative CME and usage of gas(P<0.001) but no significant association between postoperative CME and macular involvement (P=0.05).
他记得河遥县跑火船的民俗。每年这个时候,家家户户都用竹竿扎成筏子,上面堆满稻草,然后将木筏浮在江面上,点燃木筏上的稻草,让燃烧的木筏顺流而下,一眼望去,江上仿佛燃起了无数火团,天地江水都被染得红彤彤的,甚是壮观。
A Pearson Chi‐squared test showed no significant association between the presence of postoperative epiretinal membrane and usage of gas (P=0.65) and no significant association between postoperative epiretinal membrane and macular involvement (P=0.08).
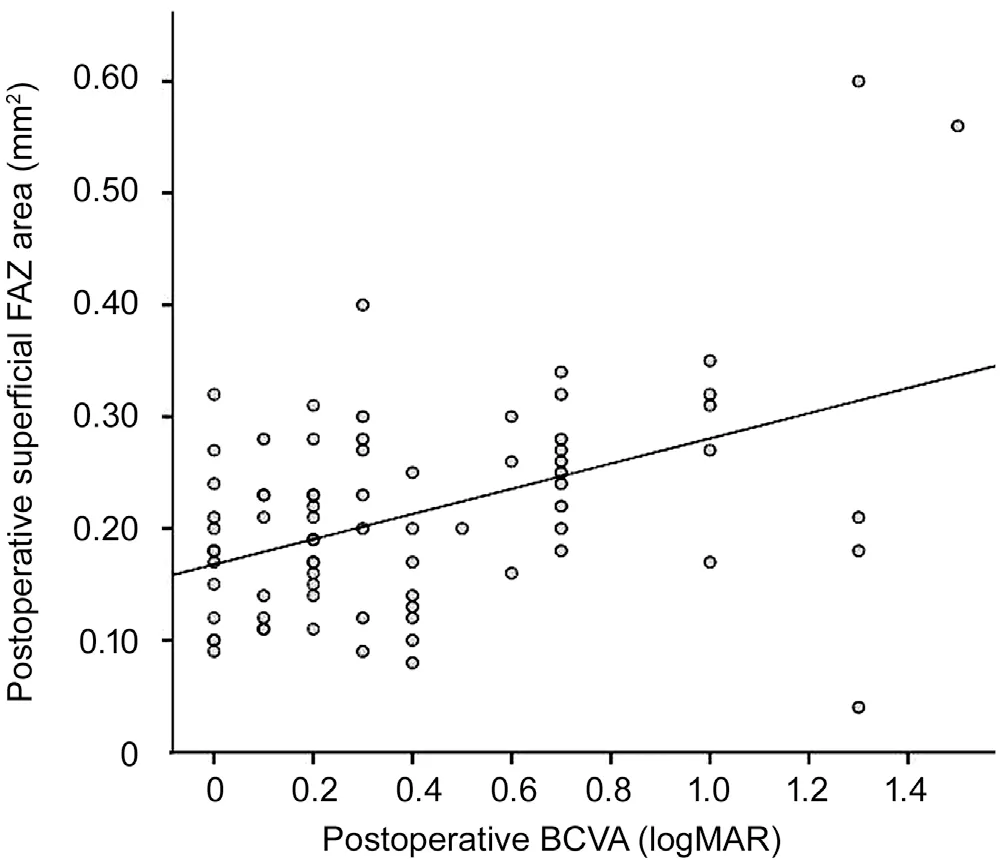
Figure 1 Correlation between postoperative BCVA and FAZ size in all four groups BCVA: Best-corrected visual acuity; FAZ: Foveal avascular zone in the superficial capillary plexus.
DISCUSSION
The downsides of silicone oil are known and well established.There is a fear of vision loss among retina surgeons when using silicon oil during PPV. The frequency of cataracts, keratopathy,ocular hypertension and glaucoma is significantly higher in eyes treated with a silicone oil tamponade[30]. Cases of severe visual loss after silicone oil were observed with a significant reduction in inner retinal thickness in eyes treated with silicone oil tamponade versus gas tamponade in RRD without macular involvement[16,31].
In cases of inferior breaks, a combined PPV with scleral buckle is also a good alternative to silicone oil tamponade and should be explored first[32‐33].
Our main result was the FAZ size in the superficial capillary plexus – which was significantly larger in both groups with RRD with macular involvementvswithout, but neither between silicone oilvsgas tamponade nor in any of the subgroups.
Retinal capillaries supply the inner two‐thirds of the retina,whereas the choriocapillaris supplies the outer third. The deep capillary plexus is located in the inner nuclear layer, and the superficial capillary plexus is located in the ganglion cell layer, but the fovea is a capillary‐free zone. Our commercially available OCTA could only measure the size of the superficial FAZ, which is why we only evaluated the superficial FAZ size in our study.
Other authors corroborate our result. Wooet al[34]published similar results in 2018 and showed that superficial and deep FAZ areas were more extensive in eyes with macula‐off RRD than in eyes with macula‐on RRD and fellow eyes. They hypothesised that, in addition to hypoxic damage caused by sensory retinal detachment from the retinal pigment epithelium, ischemic damage could occur because of changes in retinal vessels and an increase in inflammatory mediators.Despite morphologically successful surgery, this could explain some poor visual outcomes. In 2020, Bonfiglioet al[35]agreed with those results, further confirming the central role of macular detachment for visual prognosis in RRD.
Our groups were comparable in sex, age, axial length, and lens status. Although no statistical difference was shown,more patients were with PVR in group 1 (25.0%,vs10.0%in group 2, 8.3% in group 3 and 7.4% in group 4). This could be explained by the fact that an RRD involving the macula typically progresses longer than when the macula is not involved, and RRD duration is a known risk factor for developing PVR[36]. Considering that the duration of the macular detachment, and extrapolated the duration of the retinal detachment, was longer in group 1, the data, also suggest that the long duration of the detachment could be a cause for the PVR, especially in group 1.Furthermore, a silicone oil tamponade is typically preferred in complicated situations, including in the presence of PVR[37‐38].
The postoperative BCVA was statistically significantly better than the preoperative BCVA in all groups except group 2. This can be explained by the fact that the preoperative BCVA was the worst in this group and that silicone oil is usually reserved for cases with the worst visual prognosis.
We could not demonstrate any statistically significant association between postoperative epiretinal membrane and macular involvement (P=0.08). But the lowPvalue and the fact that others showed an association could signify that our group were too small to reveal that the postoperative development of an epiretinal membrane is associated with macula‐off RRD[39].
Our study had several limitations. It is a monocentric retrospective design, potentially leading to a selection bias.This study was retrospective, causing heterogeneity in the time between the last operation and the postoperative control(between 6 and 24mo). Because of this wide window, any pathological changes could be multifactorial, and a causal correlation is difficult to establish. It is an additional bias to our work. Our sample was relatively small. Therefore, further prospective studies with more patients are needed to confirm our results. Moreover, our commercially available OCTA did not allow us to measure FAZ area and PVD in the superficial and deep capillary plexus separately, giving only the values in the superficial capillary plexus.
In conclusion, our study suggests that despite the known complications caused by silicone oil, the type of tamponade used during PPV to treat an RRD does not seem to have a major impact on the future integrity of the parafoveolar vascularisation and the size of the FAZ in the superficial capillary plexus as analysed with a commercially available OCTA.
ACKNOWLEDGEMENTS
Conflicts of Interest: Hartmann M, None;Abdin AD, None;Fraenkel D,None;Munteanu C,None;Seitz B, None;Suffo S, None.
 International Journal of Ophthalmology2023年1期
International Journal of Ophthalmology2023年1期
- International Journal of Ophthalmology的其它文章
- Visual perception alterations in COVID-19: a preliminary study
- COVID-19 pandemic impact on ocular trauma in a tertiary hospital
- Apolipoprotein A1 suppresses the hypoxia-induced angiogenesis of human retinal endothelial cells by targeting PlGF
- Comparison of vegetable oils on the uptake of lutein and zeaxanthin by ARPE-19 cells
- Identifying a novel frameshift pathogenic variant in a Chinese family with neurofibromatosis type 1 and review of literature
- Recurrence risk factors of intravitreal ranibizumab monotherapy in retinopathy of prematurity: a retrospective study at one center
