MSCT动态增强扫描对肝脏淋巴瘤的诊断分析
吴建明,马周鹏,章顺壮,周建军
(1.温州医学院附属慈溪医院放射科,浙江 慈溪 315300;2.复旦大学附属中山医院放射科,上海 200032)
肝脏淋巴瘤是起源于肝脏淋巴组织和残留造血组织的罕见恶性肿瘤[1]。笔者搜集我院及上海中山医院5年来经手术病理或临床治疗随访证实的8例肝脏淋巴瘤的MSCT资料,进行回顾性分析。
1 资料与方法
1.1 一般资料
本组8例,男6例,女2例,年龄38~67岁,平均48.5岁。主要临床表现:低热6例,体重下降5例,腹部胀痛不适3例,腹胀、腹泻1例,3例伴有消瘦、贫血。
1.2 检查方法
运用GE Light speed 16排螺旋CT机,120kV,300mA,层厚5mm,每例均行腹部平扫和动脉期、静脉期、延迟期增强扫描。增强对比剂选用碘帕醇(300mgI/ml),总量按 1.5ml/kg 体重计算,注射流率3.5ml/s。经肘静脉注射,动脉期扫描延迟25s,门脉期扫描延迟65s,延迟期5min。
2 结果
2.1 CT平扫

图1 肝脏多发淋巴瘤动脉期,见肝脏多发类圆形较低密度肿块,增强弱于肝实质,边界稍模糊,部分病灶见“血管漂浮征”(箭头)。图2 多发淋巴瘤门脉期,肝脏左、右叶及尾状叶多发不规则分叶状肿块,大小不等,增强弱于肝实质,边界较清,强化不均匀,右叶病灶见“血管漂浮征”(箭头),血管局部受压变窄。图3a,3b 肝脏多发淋巴瘤。图3a:动脉期,见肝脏左、右叶及尾状叶多发不规则分叶状肿块,大小不等,增强稍强于肝实质,边界模糊,强化不均匀,左、右叶病灶见“血管漂浮征”(箭头)。图3b:门脉期肝内多发肿块强化弱于肝实质,边界欠清但较动脉期清晰,肝左叶见局限胆管增宽(短箭头),腹腔见肿大淋巴结(长箭头)。图4a,4b 肝脏多发淋巴瘤。图4a:动脉期显示肝左叶肿瘤较明显,呈类圆形较规则,增强稍强于肝实质,不均匀,边界模糊(箭头),尾状叶未见明显病灶。图4b:增强静脉期,左叶肿瘤强化弱于肝实质,边界变清,内见“血管漂浮征”(长箭头),并见右叶肝内胆管略扩张,尾状叶腔静脉前见低密度病灶(短箭头)。Figure 1.Multiple lymphoma in arterialphase,showed multi-oval tumors with low density in liver,the enhancement were fainter than normal tissue of liver,and with dim edges,some tumors showed “blood vessel floating-sign”(arrow).Figure 2.Multiple lymphoma in portal venous phase,showed multi-irregular lesions with lobulation and irregular size,the enhancement was fainter than normal tissue of liver,and with clear edges and inhomogeneous enhancement,the focus in the right lobe showed “blood vessel floating-sign”(arrow)and with local compression.Figure 3a,3b.Multiple lymphoma of liver.Figure 3a:Arterial-phase,showed multi-irregular lesions with lobulation and irregular size,the enhancement was more intense than normal tissue of liver and with dim edges and inhomogeneous enhancement,the focus in right and left lobe showed “blood vessel floating-sign”(arrow).Figure 3b:Portal venous-phase,the enhancement of multi-tumors was fainter than normal tissue of liver and with relatively clear edges than that in the arterial-phase,with local dilation of bile duct in left lobe(short arrow),there were enlarged celiac lymph-nodes(long arrow).Figure 4a,4b.Multiple lymphoma of liver.Figure 4a:Arterial-phase,showed the tumors had clear margin with oval regular shape in the left lobe,the enhancement was inhomogeneous and more intense than normal tissue of liver with dim edges(arrow).Figure 4b:Portal venous-phase,the enhancement of tumor in left lobe was fainter than normal tissue of liver and with clear edges and showed “blood vessel floating-sign”(long arrow);with local dilation of bile duct of right lobe,focus with low density can be seen in caudate lobe in front of inferior vena cava(short arrow).
6例肿瘤位于门静脉左右分支邻近或汇管区(图 1~5),2 例位于肝脏周边(图 6,7),平扫密度相对较均匀,未见明显坏死,肿瘤最大径约1~8cm,CT值约18.8~32.1HU,其中3例单发(图5~7),呈圆形或类圆形肿块,4例呈多发类圆形或不规则肿块(图1~4),1例呈左叶弥漫多发小斑片状结节(图8)。4例肿块型病灶边界较清晰(图2,5~7),其余4例肿瘤边界均较模糊(图 1,3,4,8),所有肿瘤未见钙化。
2.2 CT增强扫描
增强肿瘤动脉期呈轻-中度强化,强化相对较均匀,6例较正常肝组织强化弱,仅2例较正常肝组织强化稍强(图1~8);门脉期强化均略加强,但8例均明显弱于正常肝组织,延迟期强化减弱,6例肿瘤中见相对正常的血管走行,类似“血管漂浮征”,以门静脉期较明显,但血管局部轻度受压变窄(图1~5,8)。所有病灶边界增强后较平扫变清晰,以门脉期明显,1例平扫及动脉期均未见尾状叶病灶,但门脉期发现(图4a,4b);6例见腹腔或腹膜后肿大淋巴结,大小不均匀,呈轻-中度强化,强化相对均匀,所有病例未见明显坏死。2例见胆道轻度扩张,所有病例未见腹水,3例脾脏肿大。
2.3 病理结果
8例肿瘤临床均证实为淋巴瘤,其中2例为肝脏原发淋巴瘤,1例为手术证实,另1例为穿刺活检证实,另外6例为继发淋巴瘤,经穿刺及临床随访证实。
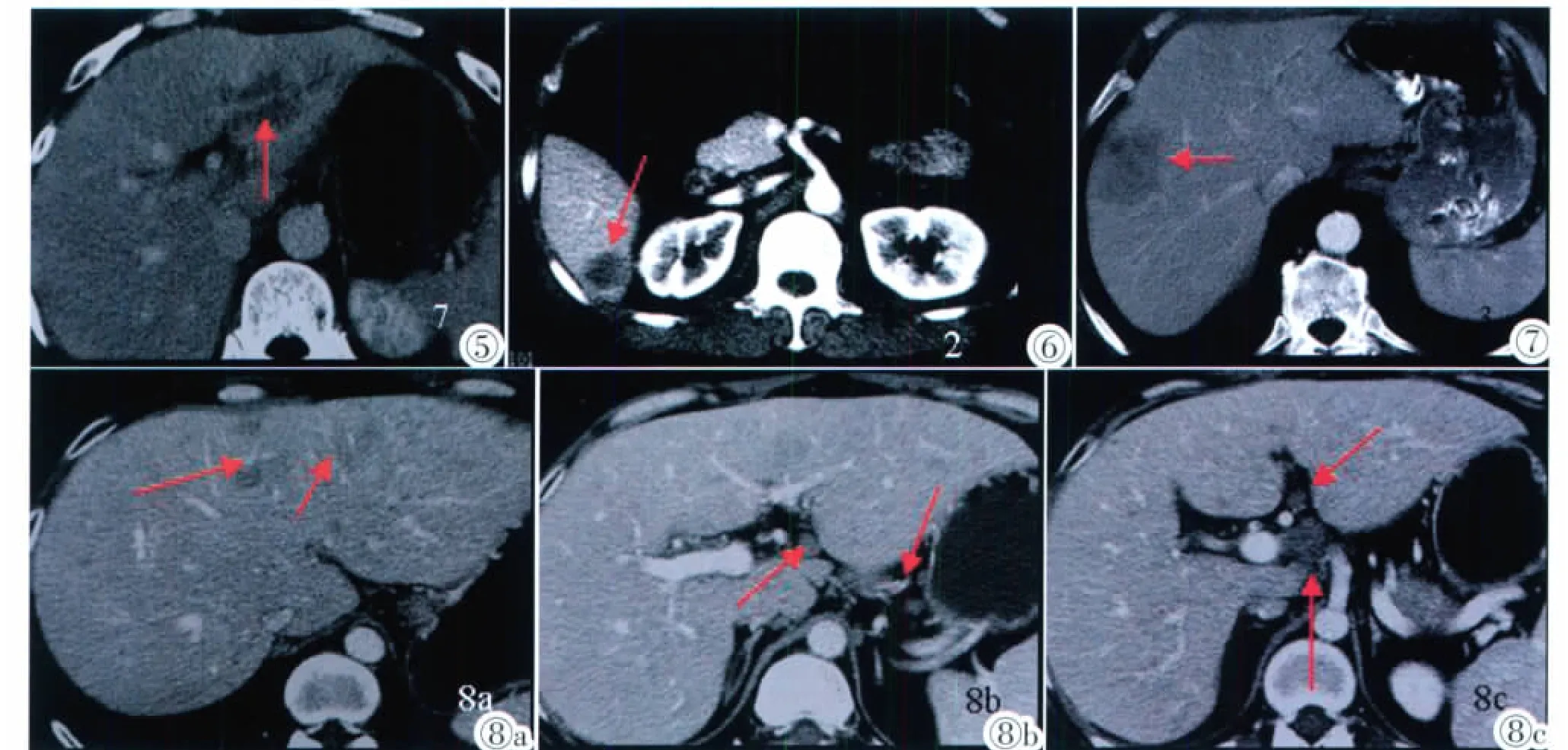
图5 肝脏单发淋巴瘤门脉期,显示肿瘤位于肝左叶,呈类圆形较规则,增强弱于肝实质,相对均匀,边界相对较清,内见“血管漂浮征”(箭头)。图6 肝右叶单发淋巴瘤动脉期,肿瘤呈类圆形肿块,位于右叶边缘近包膜区,增强弱于肝实质,边界较清,强化相对均匀(箭头)。图7 肝右叶单发淋巴瘤门脉期,肿瘤呈类圆形肿块,位于右叶边缘近包膜区,增强弱于肝实质,边界相对较清,强化不均匀(箭头)。图8a~8c 淋巴瘤弥漫性肝脏浸润。图8a:动脉期,左叶多发小斑片低密度结节,呈地图样,边界欠清,增强弱于肝实质,部分病灶见“血管漂浮征”(箭头)。图8b:门脉期,左叶多发病灶继续强化但增强仍弱于肝实质,腹腔见多个肿大淋巴结(箭头)。图8c:腹腔见多个肿大淋巴结(箭头)。Figure 5.Single-lymphoma in portal venous-phase,showed oval tumor located in the left lobe of liver with regular shape,the enhancement was homogeneous and fainter than normal tissue of liver,with relatively clear edges and “blood vessel floating-sign”(arrow).Figure 6.Single lymphoma in arterial phase,showed oval tumor located in the border of right lobe of liver,the enhancement were fainter than normal tissue of liver,with clear edge and moderate homogeneous enhancement(arrow).Figure 7.Single-lymphoma in portal venous-phase,showed oval tumor located in the border of right lobe of liver,the enhancement was fainter than normal tissue of liver,with relatively clear edges and inhomogeneous enhancement(arrow).Figure 8a~8c.Diffused lymphoma infiltrated liver.Figure 8a:Arterial-phase,showed multismall nodules with low density in the left lobe of liver,with dim edge,the enhancement were fainter than normal tissue of liver,and some foci showed “blood vessel floating-sign”(arrow).Figure 8b:Portal venous-phase,multi-foci in the left lobe showed continuous enhancement and were fainter than normal tissue of liver,and some enlarged celiac lymph-nodes were seen(arrow).Figure 8c:Multi-lymph nodes were seen in peritoneal cavity(arrow).
3 讨论
3.1 肝脏淋巴瘤的病理和临床
肝脏原发和继发淋巴瘤均罕见,以原发性更少见,发病率仅占肝脏恶性肿瘤的0.1%,占结外淋巴瘤的0.4%[2]。原发肝脏淋巴瘤起源于肝脏但无肝外侵犯及淋巴结肿大,可发生于任何年龄,尤以中年男性多见[1]。其病因及临床病理特点尚未完全认识清楚,免疫抑制治疗、器官移植、获得性免疫综合征(AIDS)患者发病率高,与免疫抑制治疗后病毒感染引起的肝脏淋巴组织增生有关[3],此外丙型肝炎病毒也可以刺激B淋巴细胞慢性多克隆增殖,导致肝脏淋巴瘤,黏膜相关淋巴瘤也可累及肝脏[4]。肝脏继发淋巴瘤较原发常见,多有肝外病灶和非引流区淋巴结肿大,其中霍奇金和非霍奇金淋巴瘤比例差异不大,与其他脏器继发淋巴瘤以非霍奇金淋巴瘤为主不同[3]。肝脏淋巴瘤无特异性临床表现,常见症状包括发热、消瘦和盗汗等。
肝脏淋巴瘤确诊依靠病理学检查。免疫组化、流式细胞术、基因重排和核型分析有助于进一步诊断,原发性者镜下可见瘤细胞呈结节状或弥漫性生长两种模式。在结节状生长模式,瘤细胞呈破坏性生长,瘤组织内没有门脉管道结构;在弥漫性生长模式,肝脏结构被保存下来,且可见瘤细胞浸润门脉结构,也可以沿着肝窦状隙扩展生长[5]。
3.2 肝脏淋巴瘤CT表现
原发性及继发性肝脏淋巴瘤CT表现相似,主要有以下几种[6]:①肝内孤立病变;②肝内多发性病变;③弥漫性肝脏浸润。Gazelle等[7]研究一组23例肝脏淋巴瘤发现,原发性肝脏淋巴瘤孤立病灶占64%,多发病灶占36%,无弥漫性肝浸润表现;而继发性肝脏淋巴瘤中,孤立病灶只占8%,多发病灶占66%,弥漫性肝浸润占26%。本组资料中2例原发性淋巴瘤均为孤立肿块;6例继发性淋巴瘤中1例为孤立病变(16.7%),4例为多发病变(66.7%),1例呈弥漫浸润(16.7%)。本组继发性肝脏淋巴瘤中弥漫浸润型比例较低,考虑为本组病例数较少的缘故。
病变平扫通常为低或较低密度,文献报道肝内孤立病变、多发性病变边界大多相对清楚,少数弥漫浸润型边界不清[6],但本组资料中4例肿块型边界较清晰,其余3例多发肿块及1例浸润型边界均较模糊,考虑可能病例较少的缘故。肿瘤密度大多数较均匀,合并出血、坏死、钙化等较少见。此外继发肝脏淋巴瘤往往伴有腹腔或腹膜后淋巴结肿大,而非引流区淋巴结异常肿大对继发肝脏淋巴瘤的诊断更有意义[3]。
肝脏淋巴瘤为乏血供肿瘤,大多数病灶动态增强呈进行性轻-中度延迟强化,动脉期强化轻微,门静脉期呈轻-中度强化,小病灶较均匀,较大病灶不均匀。门脉期强化较动脉期有加强,但明显弱于正常肝组织,大多数病灶门脉期增强后原边界稍模糊者边界更为清楚,本组即有1例门脉期发现平扫及动脉期未发现的尾状叶病灶,故门脉期意义较大,严格把握门脉期扫描能发现平扫不能发现的病灶,文献报道位于汇管区的淋巴瘤侵犯胆管时可有胆管扩张[3],本组2例即是如此。
肝脏淋巴瘤的其他强化方式包括部分肿瘤出现一过性、境界模糊的病灶周边淡片状强化,类似于异常灌注;部分肿瘤出现向心性充填现象;部分肿瘤[8]可见较薄的边缘强化,弥漫浸润型淋巴瘤肝脏组织和淋巴瘤组织强化都不明显。由于淋巴瘤起源于肝脏间质,文献报道增强扫描时部分肿瘤内可见肝脏固有血管[6],类似“血管漂浮征”,本组8例中有6例出现此征象,占75%,以门脉期明显,但血管局部轻度受压变窄。
总结国内外文献[3,6-8],结合本组资料,笔者认为以下几点有利于CT诊断肝脏淋巴瘤:①病变多位于门静脉左右支附近或位于汇管区;②单发或多发肿块(多见)或弥漫性肝脏浸润(较少见);③CT平扫呈相对较低密度,境界清楚或不清楚,密度相对均匀,出血、坏死、钙化少见;④动态增强呈进行性轻-中度强化,强化相对均匀;⑤部分病灶内可见类似“血管漂浮征”,以门脉期明显;⑥继发淋巴瘤往往伴有腹腔或腹膜后淋巴结肿大,或非引流区淋巴结异常肿大。
3.3 主要鉴别诊断
胆管细胞癌:肝左叶多见,CT平扫为低密度,多有较明显胆管扩张。动态增强早期病灶通常无明显强化,病灶中心多有持续强化,另外常伴有邻近肝脏包膜及肝组织的萎缩。
肝脏炎性病灶:CT平扫为低密度,边界不清,增强强化明显者如肝脓肿与淋巴瘤鉴别相对较易,部分强化不明显类似于淋巴瘤,有时与弥漫型鉴别难度较大,但无类似“血管漂浮征”及腹腔或腹膜后淋巴结肿大。
肝转移瘤:有原发肿瘤病史,多发多见,大小不一,分布散在,有时病灶见“靶征”或“牛眼征”。增强后可表现为边缘强化并可见肿大淋巴结,与肝淋巴瘤有重叠表现,但边缘强化较淋巴瘤明显,鉴别有时难度较大,需结合病史。
局灶性结节增生:为肝脏少见的良性占位性病变,CT平扫为低密度,增强早期病灶明显强化,中心瘢痕无明显强化,增强中晚期大多数病灶较动脉期稍弱但仍较明显,中心瘢痕逐渐延迟强化且较明显,鉴别相对容易。
[1]Ben N,Ammar C,Chaari N,et al.Primary non Hodgkin lymphoma of the liver:case report and review of the literature[J].Cancer Radiother,2006,10:595.
[2]Eom DW,Huh JR,Kang YK,et al.Clinicopathological features of eight Korean cases of primary hepatic lymphoma[J].Pathol Int,2004,54(4):830-836.
[3]陆蓉,周建军,李敏,等.肝脏淋巴瘤:动态增强CT的诊断价值[J].临床放射学杂志,2009,28(2):218-220.
[4]Chatelain D,Maes C,Yzet T,et al.Primary hepatic lymphoma of MALT type:a tumor that can simulate a liver metastasis[J].Ann Chir,2006,131:121.
[5]Emile JF,Azoulay D,Gornet JM,et al.Primary non-Hodgkin’s lymphomas of the liver with nodular and diffuse infiltration patterns have different prognoses[J].Ann Oncol,2001,12:1005-1010.
[6]丁建辉,彭卫军,周良平,等.肝脏淋巴瘤CT和MRI表现[J].中国医学计算机成像杂志,2008,14(5):409-414.
[7]Gazelle GS,Lee MJ,Hahn PF,et al.US,CT and MRI of primary and secondary liverlymphoma [J].J Comput Assist Tomogr,1994,18:412-415.
[8]Rizzi EB,Schinina V,Cristofaro M,et al.Non Hodgkin’s lymphoma of the liver in patients with AIDS:sonographic,CT,and MRI findings[J].J Clin Ultrasound,2001,29:125.