Sv2/Rv3比值在定位流出道室性期前收缩或室性心动过速中的应用价值
胡喜田,陈勤聪,穆 东,李子莉,吕新湖,魏小刚
(河北省石家庄市第一医院心内二科,河北 石家庄 050011)
Sv2/Rv3比值在定位流出道室性期前收缩或室性心动过速中的应用价值
胡喜田,陈勤聪,穆东,李子莉,吕新湖,魏小刚
(河北省石家庄市第一医院心内二科,河北 石家庄 050011)
[摘要]目的探讨V2导联S波与V3导联R波振幅(S-wave amplitude in lead V2divided by R-wave amplitude in lead V3,Sv2/Rv3)比值、胸前导联移行区指数(transitional zone index,TZI)在鉴别右心室流出道(right ventricular outflow tract,ROVT)起源室性期前收缩( premature ventricular beat,PVB)/室性心动过速(right ventricular tachycardia,VT)与左心室流出道(Left ventricular outflow tract,LOVT )起源PVB/VT中的价值。方法回顾性分析成功进行射频消融的60例流出道PVB/VT患者的心电图和电生理资料,通过体表心电图测取的Sv2/Rv3比值和TZI对PVB/VT的起源部位进行定位分析。结果60例患者均经过消融成功。消融靶点:ROVT起源45例,LOVT起源15例;LOVT起源PVB/VT的TZI较ROVT起源PVB/VT明显小。TZI<0作为LOVT起源PVB/VT临界值,其对LOVT起源PVB/VT的敏感度为80.0%,特异度为82.2%,准确度为81.7%,阳性预测值为60.0%,阴性预测值为92.5%。LOVT起源PVB/VT的Sv2/Rv3比值较ROVT起源PVB/VT明显小。Sv2/Rv3比值<1.5作为LOVT起源PVB/VT临界值,其对LOVT起源PVB/VT的敏感度为86.7%,特异度为84.4%,准确度为85.0%,阳性预测值为65.0%,阴性预测值为95.0%。结论Sv2/Rv3比值、TZI对流出道PVB/VT定位诊断具有较好的预测价值。
[关键词]室性早搏复合征;心电描记术;导管消融术
doi:10.3969/j.issn.1007-3205.2015.07.005
流出道特发性室性心动过速(ventricular tachycardia,VT)或室性期前收缩(premature ventricular beat,PVB)最常见的起源部位为右心室流出道(right ventricular outflow tract,ROVT)、主动脉窦、肺动脉、希氏束附近等[1-4],心电图表现为左束支传导阻滞和电轴右偏。通过体表心电图可以定位流出道PVB/VT的起源部位,为临床提供参照,减少手术时间、费用、X线曝光时间。目前有几种心电图定位方法得到临床推荐[5-8],但它们容易受到导联位置、心脏解剖、心脏转位、心室肥厚、体型、胸部畸形、优势传导通路存在等[6,9-11]影响,其准确度与实用性受到限制。本研究对射频消融成功的60例流出道PVB/VT患者的心电图和电生理资料进行回顾性分析,评价最新心电图定位指标V2导联S波与V3导联R波振幅(S-wave amplitude in lead V2divided by R-wave amplitude in lead V3,Sv2/Rv3)比值[11]与临床已验证的胸前导联移行区指数(transitional zone index,TZI)[7]在指数定位流出道VT、PVB的应用价值,提供新的定位流出道起源指标。
1资料与方法
1.1一般资料2010年1月—2014年2月河北省石家庄市第一医院心内科连续进行射频消融成功的流出道PVB/VT 60例,男性36例,女性24例,年龄18~65岁,平均( 42.5±13.3 )岁。超声心动图检查除外心力衰竭患者,其中ROVT起源45例,左心室流出道(left ventricular outflow tract,LOVT)起源VT 15例。流出道PVB/VT的心电图特点为:左束支传导阻滞伴电轴右偏,Ⅱ、Ⅲ、aVF导联有高振幅的R波,V1导联QRS波为rS型。
1.2方法
1.2.1用Sv2/Rv3比值判断流出道起源所有研究对象均在安静环境下描记心电图,用日本光电Cardimax Fx-740212导联心电图机,选择12导联同步描记心电图。记录PVB/VT发作时和窦性心律心电图,心电图振幅10 mm,速度25 mm/s,电极置于标准的胸前导联和肢体导联。特别关注胸前导联V1位于胸骨右缘第Ⅳ肋间,V2位于胸骨左缘第Ⅳ肋间,因为不确切的导联位置可能导致记录的PVB/VT QRS波明显改变[12]在同一12导联心电图上,应用游标卡尺进行PVB/VT和窦性心律时的心电图分析。Sv2/Rv3比值测定相关定义:Sv2/Rv3比值是指PVB/VT在V2导联QRS波的S波与V3导联QRS的R波振幅的比值。测量患者心电图PVB/VT在V2导联QRS波的S波与V3导联R波的幅度,并进行两者振幅比值的计算,Sv2/Rv3比值≤ 1.5 时提示PVB/VT起源于LOVT,若>1.5时,提示起源于ROVT。见图1。
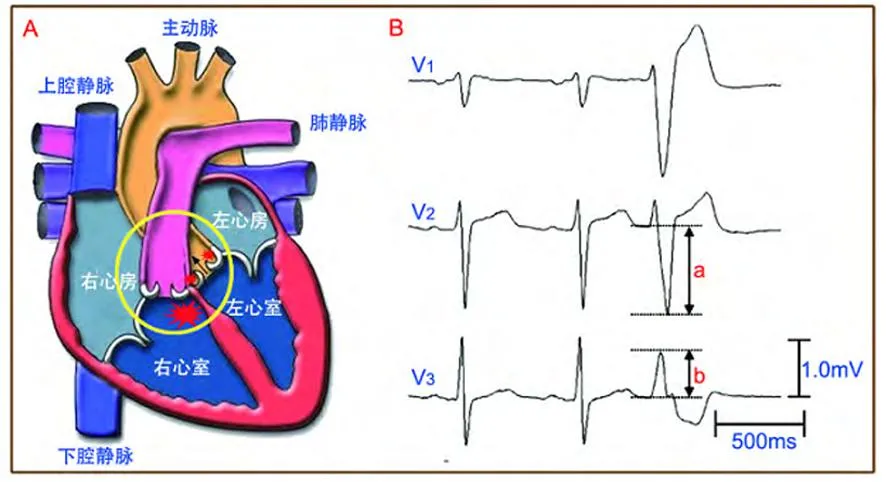
图1流出道局部解剖关系与Sv2/Rv3比值测定示意图
Figure 1A transition zone of outflow of anatomy and Sv2/Rv3
1.2.2用TZI判断流出道起源按照Yoshida等[11]提出的方法测取TZI。确定移行区导联:当胸导联的R波与S波比值为0.9~1.1时则为移行区,正常时移行区位于V3或V4导联。移行区积分:移行区所在的导联数即为移行区的积分,如出现在导联V4则积4分,出现在V4与V5导联之间则积4.5分,见表1,图2。移行区指数:用PVB或VT的移行区积分减去窦性心律的移行区积分为移行区指数,当其<0时提示位于主动脉窦内,≥0时提示位于ROVT。

表1 胸前导联R波移行部位与胸前导

图2流出道解剖与胸前导联移行区积分示意图
Figure 2A transition zone of outflow of anatomy and chest lead transitional zone index
1.3统计学方法应用SPSS 18.0软件进行统计学分析。受试者工作曲线分析得出最佳临界值,计算敏感度、特异度、准确度、阳性预测值、阴性预测值。P<0.05为差异有统计学意义。
2结果
2.1电生理标测消融结果患者手术即刻成功60例,ROVT消融成功45例,LOVT消融成功15例。60例中PVB 46例、VT 14例。
2.2TZI对流出道PVB/VT定位诊断60例患者12导联心电图中,有49例与电生理检查结果相符,其准确度为81.7%(49/60),其中对ROVT起源PVB/VT的准确度为82.2%(37/45),对LOVT起源PVB/VT的准确度为80.0%(12/15)。TZI<0定位LOVT起源PVB/VT的敏感度、特异度、准确度、阳性预测值和阴性预测值分别为80.0%、82.2%、81.7%、60.0%和92.5%。Sv2/Rv3比值对流出道PVB/VT定位诊断:60例患者12导联心电图中,有51例与电生理检查结果相符,其准确度为85.0%(51/60),其中对ROVT起源PVB/VT的准确度为84.4%(38/45),对LOVT起源PVB/VT的准确度为86.7%(13/15)。 Sv2/Rv3比值≤1.5定位LOVT起源PVB/VT的敏感度、特异度、准确度、阳性预测值和阴性预测值分别为86.7%、84.4%、85.0%、65.0%和95.0%。后者指标更好,见表2。

表2 TZI、Sv2/Rv3比值定位LOVT起源PVB/VT
3讨论
射频消融是治疗流出道PVB/VT的主要方法之一,对药物疗效差、心脏扩大心功能下降的患者能起到根治作用[3,13-18];但LOVT起源PVB/VT和ROVT起源PVB/VT的消融术式、 有效消融靶点等方面都存在明显不同,因而迫切需要术前心电图能作出更高水平的鉴别,目前心电图已为临床提供良好的借鉴。由于ROVT和主动脉窦、大静脉、二尖瓣环与主动脉窦连接处等解剖关系邻近,以及心脏转位、胸廓畸形等影响使心电图定位PVB/VT的起源部位存在一定的误差,寻找一种敏感度和特异度均高的心电图指标成为临床心电图学研究的热点。
LVOT 与 RVOT毗邻,两者均与主动脉根部相毗邻,主动脉根部占据心脏的中心部位,ROVT位于主动脉根部左侧前面[16]。这些解剖特点造成起源于主动脉窦的PVB/VT较ROVT起源的PVB/VT在胸前V1、V2导联R波持续时间更长,R/S比值更高[11]。因此,应用V1、V2导联R波或S波幅度可能找到合理的心电图定位指标,解剖分析显示V3导联位置与ROVT的距离较主动脉根部更近。解剖特点决定V3导联R波幅度与V2导联S波幅度可用于定位流出道PVB/VT起源,具有较高的敏感度和特异度,Sv2/Rv3比值较上述两项指标的敏感度、特异度更高。
Quyang等[5]在心电图进行鉴别的研究中发现,起源于主动脉窦的PVB/VT,其 V1导联QRS波的R波时限指数和R波振幅指数均明显大于ROVT起源的PVB/VT的相应值,提出鉴别两者的心电图标准:①先确定PVB/VT具有心室流出道起源的一般心电图特点;②胸导联的移行区位于V2导联;③V1导联的R波时限指数≥50%,R波振幅指数≥30%。凡满足上述条件的PVB/VT则起源于主动脉窦,未能满足者起源于ROVT。当患者的心脏无明显转位时,上述诊断与鉴别标准的敏感度高达80%,特异度为79%。此心电图鉴别标准在临床应用时发现,当患者原本窦性心律就存在心脏转位时,能明显影响PVB/VT起源部位精确定位。Brian等[6]在研究中发现,R波时限指数和R/S振幅指数对心脏转位的患者中定位诊断价值降低,提出一个“V2移行比”的概念,即VT时R/R+S或窦性心律时R/R+S的比值来克服心脏转位等影响,LOVT起源的VT的V2移行比显著大于ROVT起源的VT,当V2转变比>0.6时,预测LOVT起源VT的准确度为91%,而当VT时胸前导联移行晚于窦性心律时,则可100%排除LOVT起源的可能。2011年,Yoshida等[7]提出TZI的概念可用于ROVT或LOVT起源PVB/VT的鉴别,并具有鉴别两者较高的敏感度和特异度,可以避免心室转位和本身心电图干扰作用,进一步提高定位诊断的准确度。2014年,Yoshida等[11]再次提出一项新指标Sv2/Rv3比值,通过观察207例流出道PVB/VT并成功进行了射频消融治疗的患者,其中心律失常起源于ROVT 154例,起源于LOVT 53例,Sv2/Rv3比值鉴别两者的敏感度为89%,特异度为94%,较R波时限指数和R/S振幅指数,Sv2/Rv3定位更加准确,且差异有统计学意义;该组病例不仅包括器质性心脏病患者,而且包括非器质性心脏病患者,拓宽了心电图定位PVB/VT起源的应用范围。
本研究通过回顾性分析60例流出道PVB/VT心电图显示:TZI与射频消融的准确度为81.7%(49/60),其中对ROVT起源PVB/VT的准确度为82.2%(37/45),对LOVT起源PVB/VT的准确度为80.0%(12/15);Sv2/Rv3比值与射频消融手术的准确度为85.0%(51/60),其中对ROVT起源PVB/VT的准确度为84.4%(38/45),对LOVT起源PVB/VT的准确度为86.7%(13/15);TZI<0定位主动脉窦起源心律失常的敏感度为80.0%,特异度为82.2%,准确度为81.7%,阳性预测值为60.0%,阴性预测值92.5%;Sv2/Rv3比值≤1.5的敏感度为86.7%,特异度为84.4%,准确度为85.0%,阳性预测值为65.0%,阴性预测值为95.0%。表明Sv2/Rv3比值较胸前导联移行比有更好的准确度和特异度,倾向于更有临床应用的优势,这与Yoshida 等[7,11]的研究一致。关于两者的优劣需要通过扩大样本例数进一步研究。通过临床验证显示,TZI与Sv2/Rv3比值均是定位流出道起源部位的可靠指标,有一定的临床应用价值,值得临床推广应用。
本研究手术例数较少,且为回顾性研究,研究入组分析时间跨度较长,对心电图的分析靠手测,可能存在标准化不足,影响研究的可靠性。今后如能增加手术例数,进行前瞻性研究设计,可能会获得更为可靠的临床研究结果。
[参考文献]
[1]Yamada T,McElderry HT,Okada T,et al.Idiopathic left ventricular arrhythmias originating adjacent to the left aortic sinus of valsalva: electrophysiological rationale for the surface electrocardiogram[J].J Cardiovasc Electrophysiol,2010,21(2): 170-176.
[2]Yamada T,McElderry HT,Doppalapudi H,et al.Idiopathic ventricular arrhythmias originating from the left ventricular summit: anatomic concepts relevant to ablation[J].Circ Arrhythm Electrophysiol,2010,3(6):616-623.
[3]Aliot EM,Stevenson WG,Almendral-Garrote JM,et al.EHRA/HRS Expert Consensus on Catheter Ablation of Ventricular Arrhythmias : developed in a partnership with the European Heart Rhythm Association(EHRA),a Registered Branch of the European Society of Cardiology (ESC),and the Heart Rhythm Society(HRS);in collaboration with the American College of Cardiology (ACC) and the American Heart Association (AHA)[J].Europace,2009,11(6):771-817.
[4]Yokokawa M,Good E,Crawford T,et al.Reasons for failed ablation for idiopathic right ventricular outflow tract-like ventricular arrhythmias[J].Heart Rhythm,2013,10(8):1011-1018.
[5]Ouyang F,Fotuhi P,Ho SY,et al.Repetitive monomorphic ventricular tachycardia originating from the aortic sinus cusp: electrocardiographic characterization for guiding catheter ablation[J].J Am Coll Cardiol,2002,39(3):500-508.
[6]Brian BP,Park RE,Marchlinski FE,et al.The V(2) transition ratio: a new electrocardiographic criterion for distinguishing left from right ventricular outflow tract tachycardia origin[J].J Am Coll Cardiol,2011,57(22):2255-2262.
[7]Yoshida N,Inden Y,Uchikawa T,et al.Novel transitional zone index allows more accurate differentiation between idiopathic right ventricular outflow tract and aortic sinus cusp ventricular arrhythmias[J].Heart Rhythm,2011,8(3):349-356.
[8]Cheng Z,Cheng K,Deng H,et al.The R-wave deflection interval in lead V3 combining with R-wave amplitude index in lead V1: a new surface ECG algorithm for distinguishing left from right ventricular outflow tract tachycardia origin in patients with transitional lead at V3[J].Int J Cardiol,2013,168(2):1342-1348.
[9]Yamada T,Murakami Y,Yoshida N,et al.Preferential conduction across the ventricular outflow septum in ventricular arrhythmias originating from the aortic sinus cusp[J].J Am Coll Cardiol,2007,50(9):884-891.
[10]王宇彬,楚建民,宋书凯,等.室间隔优势传导导致主动脉窦起源室性早搏呈左束支阻滞传导图形[J].中华心血管病杂志,2013,41(1):13-17.
[11]Yoshida N,Yamada T,McElderry HT,et al.A novel electrocardiographic criterion for differentiating a left from right ventricular outflow tract tachycardia origin: the V2S/V3R index[J].J Cardiovasc Electrophysiol,2014,25(7):747-753.
[12]Anter E,Frankel DS,Marchlinski FE,et al.Effect of electrocardiographic lead placement on localization of outflow tract tachycardias[J].Heart Rhythm,2012,9(5):697-703.
[13]李健,于波,杨耀,等.冠状动脉窦内射频消融室性心律失常的研究[J].临床心电学杂志,2013,22(1):37-40.
[14]吴晓羽,李为民,谭震,等.起源于左ROVT心动过速和早搏的射频导管消融治疗[J].中华心血管病学杂志,2007,35(7):620-624.
[15]路长鸿,常瑜,朱凌华,等.射频导管消融治疗主动脉左冠状窦室性心律失常疗效观察[J].中国循证心血管医学杂志,2011,3(2):136-137.
[16]Anderson RH.Clinical anatomy of the aortic root[J].Heart,2000,84(6):670-673.
[17]Fang F,Wen C,Yang L,et al.Radiofrequency ablation can reverse the structural remodeling caused by frequent premature ventricular contractions originating from the right ventricular outflow tract even in a“normal heart”[J].Clinics(Sao Paulo),2013,68(10):1312-1317.
[18]Penela D,van Huls van Taxis C,Aguinaga L.Neurohormonal,structural,and functional recovery pattern after premature ventricular complex ablation is independent of structural heart disease status in patients with depressed left ventricular ejection fraction a Prospective multicenter study[J].J Am Coll Cardiol,2013,62(13):1195-1202. T,McElderry HT,Okada T,et al.Idiopathic left ventricular arrhythmias originating adjacent to the left aortic sinus of valsalva: electrophysiological rationale for the surface electrocardiogram[J].J Cardiovasc Electrophysiol,2010,21(2): 170-176.
[2]Yamada T,McElderry HT,Doppalapudi H,et al.Idiopathic ventricular arrhythmias originating from the left ventricular summit: anatomic concepts relevant to ablation[J].Circ Arrhythm Electrophysiol,2010,3(6):616-623.
[3]Aliot EM,Stevenson WG,Almendral-Garrote JM,et al.EHRA/HRS Expert Consensus on Catheter Ablation of Ventricular Arrhythmias : developed in a partnership with the European Heart Rhythm Association(EHRA),a Registered Branch of the European Society of Cardiology (ESC),and the Heart Rhythm Society(HRS);in collaboration with the American College of Cardiology (ACC) and the American Heart Association (AHA)[J].Europace,2009,11(6):771-817.
[4]Yokokawa M,Good E,Crawford T,et al.Reasons for failed ablation for idiopathic right ventricular outflow tract-like ventricular arrhythmias[J].Heart Rhythm,2013,10(8):1011-1018.
[5]Ouyang F,Fotuhi P,Ho SY,et al.Repetitive monomorphic ventricular tachycardia originating from the aortic sinus cusp: electrocardiographic characterization for guiding catheter ablation[J].J Am Coll Cardiol,2002,39(3):500-508.
[6]Brian BP,Park RE,Marchlinski FE,et al.The V(2) transition ratio: a new electrocardiographic criterion for distinguishing left from right ventricular outflow tract tachycardia origin[J].J Am Coll Cardiol,2011,57(22):2255-2262.
[7]Yoshida N,Inden Y,Uchikawa T,et al.Novel transitional zone index allows more accurate differentiation between idiopathic right ventricular outflow tract and aortic sinus cusp ventricular arrhythmias[J].Heart Rhythm,2011,8(3):349-356.
[8]Cheng Z,Cheng K,Deng H,et al.The R-wave deflection interval in lead V3 combining with R-wave amplitude index in lead V1: a new surface ECG algorithm for distinguishing left from right ventricular outflow tract tachycardia origin in patients with transitional lead at V3[J].Int J Cardiol,2013,168(2):1342-1348.
[9]Yamada T,Murakami Y,Yoshida N,et al.Preferential conduction across the ventricular outflow septum in ventricular arrhythmias originating from the aortic sinus cusp[J].J Am Coll Cardiol,2007,50(9):884-891.
[10]王宇彬,楚建民,宋书凯,等.室间隔优势传导导致主动脉窦起源室性早搏呈左束支阻滞传导图形[J].中华心血管病杂志,2013,41(1):13-17.
[11]Yoshida N,Yamada T,McElderry HT,et al.A novel electrocardiographic criterion for differentiating a left from right ventricular outflow tract tachycardia origin: the V2S/V3R index[J].J Cardiovasc Electrophysiol,2014,25(7):747-753.
[12]Anter E,Frankel DS,Marchlinski FE,et al.Effect of electrocardiographic lead placement on localization of outflow tract tachycardias[J].Heart Rhythm,2012,9(5):697-703.
[13]李健,于波,杨耀,等.冠状动脉窦内射频消融室性心律失常的研究[J].临床心电学杂志,2013,22(1):37-40.
[14]吴晓羽,李为民,谭震,等.起源于左ROVT心动过速和早搏的射频导管消融治疗[J].中华心血管病学杂志,2007,35(7):620-624.
[15]路长鸿,常瑜,朱凌华,等.射频导管消融治疗主动脉左冠状窦室性心律失常疗效观察[J].中国循证心血管医学杂志,2011,3(2):136-137.
[16]Anderson RH.Clinical anatomy of the aortic root[J].Heart,2000,84(6):670-673.
[17]Fang F,Wen C,Yang L,et al.Radiofrequency ablation can reverse the structural remodeling caused by frequent premature ventricular contractions originating from the right ventricular outflow tract even in a“normal heart”[J].Clinics(Sao Paulo),2013,68(10):1312-1317.
[18]Penela D,van Huls van Taxis C,Aguinaga L.Neurohormonal,structural,and functional recovery pattern after premature ventricular complex ablation is independent of structural heart disease status in patients with depressed left ventricular ejection fraction a Prospective multicenter study[J].J Am Coll Cardiol,2013,62(13):1195-1202.
(本文编辑:许卓文)
[中图分类号]R541.7
[文献标志码]A
[文章编号]1007-3205(2015)07-0759-05
V2S/V3R index for differentiating origin of idiopathic outflow tract ventricular arrhythmia
HU Xi-tian,CHEN Qin-cong,MU Dong,LI Zi-li,LV Xin-hu,WEI Xiao-gang
(Department of Cardiology,the First Hospital of Shijiazhuang City,Shijiazhuang 050011,China)
[Abstract]ObjectiveTo explore the value of S-wave amplitude in lead V2divided by R-wave amplitude in lead V3(Sv2/Rv3) and transitional zone index(TZI)for distinguishing the ROVT PVB/VT from left ventricular outflow tract(LOVT).MethodsRetrospective analysis was made in the electrocardiogram and electrophysiology from 60 patients with outflow tract PVB/VT,differentifating the ROVT PVB/VT from LOVT by Sv2/Rv3 index and TZI in electrocardiogram.ResultsA total of 60 patients underwent radiofrequency catheter ablation successfully,originating from right ventricular outflow tract(ROVT) in 45 cases,originating from LOVT in 15 cases.The TZI was significantly lower in LOVT origin than in RVOT origin.A cutoff value of TZI<0 predicting LOVT origin with sensitivity 80.0%,specificity 82.2%,accuracy 81.7%,positive predictive value 60.0% and negative predictive value 92.5%.The Sv2/Rv3 index was significantly lower in LOVT origin than in RVOT origin.A cutoff value of Sv2/Rv3 index≤1.5 predicting LOVT with sensitivity 86.7%,specificity 84.4%,accuracy 85.0%,positive predictive value 65.0% and negative predictive value 95.0%.ConclusionWe presented a new simple surface ECG algorithm,Sv2/Rv3 index and transitional zone index,which can reliably distinguish LVOT from RVOT origin in idiopathic outflow tract PVB/VT.
[Key words]ventricular premature complexes;electrocardiography;catheter ablation

