MicroRNAs in Parkinson’s disease and emerging therapeutic targets
Bridget Martinez, Philip V. Peplow
1 Department of Molecular and Cellular Biology, University of California, Merced, CA, USA
2 Department of Anatomy, University of Otago, Dunedin, New Zealand
MicroRNAs in Parkinson’s disease and emerging therapeutic targets
Bridget Martinez1, Philip V. Peplow2,*
1 Department of Molecular and Cellular Biology, University of California, Merced, CA, USA
2 Department of Anatomy, University of Otago, Dunedin, New Zealand
Parkinson’s disease (PD) is the second most common age-related neurodegenerative disorder, with the clinical main symptoms caused by a loss of dopaminergic neurons in the substantia nigra, corpus striatum and brain cortex. Over 90% of patients with PD have sporadic PD and occur in people with no known family history of the disorder. Currently there is no cure for PD. Treatment with medications to increase dopamine relieves the symptoms but does not slow down or reverse the damage to neurons in the brain. Increasing evidence points to in flammation as a chief mediator of PD with in flammatory response mechanisms, involving microglia and leukocytes, activated following loss of dopaminergic neurons. Oxidative stress is also recognized as one of the main causes of PD, and excessive reactive oxygen species (ROS) and reactive nitrogen species can lead to dopaminergic neuron vulnerability and eventual death. MicroRNAs control a range of physiological and pathological functions, and may serve as potential targets for intervention against PD to mitigate damage to the brain. Several studies have demonstrated that microRNAs can regulate oxidative stress and prevent ROS-mediated damage to dopaminergic neurons, suggesting that speci fic microRNAs may be putative targets for novel therapeutic strategies in PD. Recent human and animal studies have identi fied a large number of dysregulated microRNAs in PD brain tissue samples, many of which were downregulated.The dysregulated microRNAs affect downstream targets such asSNCA, PARK2, LRRK2, TNFSF13B, LTA,SLC5A3, PSMB2, GSR, GBA, LAMP-2A, HSC. Apart from one study, none of the studies reviewed had used agomirs or antagomirs to reverse the levels of downregulated or upregulated microRNAs, respectively, in mouse models of PD or with isolated human or mouse dopaminergic cells. Further large-scale studies of brain tissue samples collected with short postmortem interval from human PD patients are warranted to provide more information on the microRNA pro files in different brain regions and to test for gender differences.
Parkinson’s disease; brain tissue; microRNAs; therapeutic targets; humans; animal models
Introduction
Parkinson’s disease (PD) is the second most common age-related neurodegenerative disorder, affecting an estimated 7–10 million people worldwide (Valente et al., 2012). While less than 0.1% are affected among persons < 60 years of age, prevalence increases to 1–2% in those aged > 60 years (Shulman et al., 2011) and 2–3% in those aged > 80 years (de Lau and Breteler, 2006). The clinical main symptoms are caused by a loss of dopaminergic neurons in the substantia nigra, corpus striatum and brain cortex (Braak et al., 2004; Shulman et al.,2011). Patients exhibit a range of clinical symptoms, with the most common affecting motor function including resting tremor, rigidity, akinesia, bradykinesia and postural instability (Winklhofer and Haass, 2010). Non-motor symptoms are often an integral part of the disease and some of them,such as depression, anxiety and hyposmia, can precede the onset of Parkinsonism (Ceravolo et al., 2010). Over 90% of patients with PD have sporadic PD, also known as idiopathic PD (Thomas and Beal, 2007; Valente et al., 2012), and occur in people with no known family history of the disorder. Widespread aggregates of α-synuclein protein in the substantia nigra, together with the presence of cytoplasmic α-synuclein aggregates called Lewy bodies and α-synuclein filaments called Lewy neurites in degenerating neurons, are a pathological hallmark of sporadic PD (Winklhofer and Haass, 2010). Elevated levels of α-synuclein mRNA in substantia nigra dopamine neurons have been observed in sporadic PD (Shulman et al., 2011). Although the causes of these cases remain unclear,sporadic PD likely results from a complex interaction of environmental/acquired and genetic/inherited factors (Nuytemans et al., 2010). A small proportion of cases can be attributed to genetic factors with an autosomal or recessive pattern of inheritance and are sometimes referred to as familial Parkinson’s disease. Mutations inSNCA, PARKIN, UCHL-1, PINK1,DJ-1andLRRK2are the origin of familial cases of Parkinson’s disease, although they account for only 5–10% of patients.
MicroRNAs are abundant, endogenous, short, noncoding RNAs that act as important post-transcriptional regulators of gene expression by binding to the 3’-untranslated region(UTR) of their target mRNAs, thereby interfering with translation or causing destabilization or preferential cleavage of target RNAs (Baek et al., 2008; Ha and Kim, 2014). During the last decade, substantial knowledge has accumulated regarding the biogenesis of microRNAs, their molecular mechanisms and functional roles in a variety of cellular contexts. Altered expression of certain microRNA molecules suggests that they could have a crucial regulatory role in disorders. Increasing evidence points to in flammation as a chief mediator of PD with in flammatory response mechanisms, involving microglia and leukocytes, activated following loss of dopaminergic neurons (Rocha et al., 2015). The free radical nitric oxide (NO)plays a key role in the pathogenesis of in flammation. Under normal physiological conditions, NO has an anti-inflammatory effect, but is considered a pro-inflammatory mediator due to overproduction in abnormal situations (Sharma et al., 2007). The NO synthases (NOS) family synthesizes NO in a two-step reaction involving oxygen and many cofactors.Among the NOS isoforms (neuronal, endothelial, and inducible: nNOS, eNOs, iNOS, respectively), the nNOS is the most implicated in a wide range of functions and pathologies in the CNS. In the CNS, nNOS is located inside the postsynaptic membrane and is physically bound to N-methyl-D-aspartate(NMDA)-type glutamate receptors. Under physiological conditions, mild activation of synaptic NMDARs allows influx of Ca2+, which leads to nNOS catalytic activation (Maccallini and Amoroso, 2016). By contrast, hyperactivation of extrasynaptic NMDARs can lead to an abnormal Ca2+influx into the postsynaptic neuron, with a subsequent overstimulation of nNOS and excessive NO production. This leads to generation of reactive oxygen and nitrogen species that cause DNA and lipid damage (Heinrich et al., 2013; Maccallini et al., 2016).Consequently, neurotransmission is impaired due to mitochondrial dysfunction and synaptic damage. NO also induces apoptosis (Cao et al., 2005). Several microRNAs (miR-939,miR-26a) have been identi fied to bind with the human iNOS 3’-UTR and exert a translational blockade of human iNOS synthesis (Guo and Geller, 2014). Also, overexpression of microRNA-155 decreased, whereas inhibition of microRNA-155 increased, eNOS expression and NO production in human umbilical vein endothelial cells (Sun et al., 2012).
Oxidative stress is recognized as one of the main causes of PD, and excessive reactive oxygen species (ROS) can lead to dopaminergic neuron vulnerability and eventual death. Several studies have demonstrated that microRNAs can regulate oxidative stress inin vitroandin vivoanimal models of PD.Relevant microRNAs involved in regulating oxidative stress can prevent ROS-mediated damage to dopaminergic neurons,suggesting that specific microRNAs may be putative targets for novel therapeutic strategies in PD (Xie and Chen, 2016).Impairment of mitochondrial function resulting in cellular damage is also linked to aging and neurodegeneration and evidence suggests it plays a central role in the pathogenesis of PD (Winklhofer and Haass, 2010). Glutamatergic transmission and in flammatory response mechanisms are altered in striatal neurons following dopaminergic denervation (Gardoni and Bellone, 2015; Kim et al., 2015). Despite extensive research,the molecular mechanisms mediating the changes in striatal neurons following dopaminergic denervation are still unclear.Understanding the mechanisms underlying this process is important for gaining new insights into the pathogenesis of PD. A recent study suggests that the age-related decline of Dicer enzyme combined with increased cellular stress in dopaminergic neurons may compromise microRNA biosynthesis thus contributing to neurodegeneration in PD (Chmielarz et al., 2017).
Circulating microRNAs have been proposed as diagnostic biomarkers for PD and would enable detection at the earliest stages of the disease for therapy to be implemented to delay the onset or minimize the changes in the later stages of the disease. However, other organs may contribute to microRNAs in the blood so that the circulating levels may not accurately re flect the levels of speci fic microRNAs in the diseased brain itself (Sierzega et al., 2017). We have searched the PubMed database for studies on microRNA expression in brain tissue of patients with PD and animal models of PD and their involvement in the pathophysiology of the disease, and which might serve as therapeutic targets using microRNA mimics or antagomirs. The studies retrieved in the literature search covered the period 2007–2017.
Neuropathology/Braak Staging and Animal Models of PD
The diagnosis of PD is still largely made on clinical grounds by four cardinal signs (tremor, bradykinesia, rigidity, and postural instability) as there is no de finitive laboratory test to con firm the diagnosis during life, apart from gene testing in a reduced number of cases. Non-motor symptoms may predate diagnosis by several years and a schematic has been proposed depicting normal aging and PD-related nigral cell loss over time including the time at which diagnosis typically occurs(Noyce et al., 2016). Pre-symptomatic markers of PD may include olfactory loss, depression, rapid eye movement (REM)sleep disorder, and constipation (Schapira et al., 2017). Most reviews of PD indicate that motor signs first appear when approximately 50% of substantia nigra dopaminergic neurons are lost (Marsden, 1990; Ross et al., 2004). A regression analysis of neuron countsversusduration of PD indicated that the number of neurons lost at the time of symptom onset was 31%, adjusted for age (Fearnley and Lees, 1991). At the time of 1 year post diagnosis, patients with PD may retain up to 90%of their substantia nigra dopamine neurons and 50% of their striatal dopaminergic innervation (Kordower et al., 2013).
Based on autopsy findings in patients with PD, Braak et al. (2003) reported that the intraneuronal formation of Lewy bodies and Lewy neurites has a topographically predictable progression. Accordingly Braak staging was created based on the presence of Lewy bodies and Lewy neurites. The pre-symptomatic phase usually falls within Stages 1, 2 and 3,while the symptomatic phase falls into Stages 3, 4, 5 and 6.Stage 1 (medulla oblongata): lesions initially occur in the dorsal glossopharyngeal/vagal motor nucleus and frequently in the anterior olfactory nucleus. There may also be involvement of intermediate reticular zone. Stage 2 (medulla oblongata and pontine tegmentum): this includes the pathology of stage 1 together with lesions in the caudal raphe nuclei, gigantocellular reticular nucleus, and coeruleus-subcoeruleus complex.Stage 3 (midbrain): pathology of stage 2 plus midbrain lesions,particularly in the pars compacta of the substantia nigra. Stage 4 (basal prosencephalon and mesocortex): pathology of stage 3 with lesion at prosencephalon; cortical involvement is confined to the temporal mesocortex (transentorhinal region) and allcortex (CA2-plexus)-the neocortex is unaffected. Stage 5(neocortex): pathology of stage 4 plus lesions in higher order sensory association areas of the neocortex and prefrontal neocortex. Stage 6 (neocortex): pathology of stage 5 plus lesions in first order sensory association areas of the neocortex and premotor areas, occasionally mild changes in primary sensory areas and the primary motor field.
Neurotoxic and genetic animal models have been used to produce PD-related pathology and symptomatology (Blesa et al., 2012; Jackson-Lewis et al., 2012). Neurotoxin-based models produced by 6-hydroxydopamine (6-OHDA) and 1-methyl-1,2,3,6-tetrahydropyridine (MPTP) administration are the most widely used toxic models. Mice, rats, cats, dogs,and monkeys are all sensitive to 6-OHDA. Although similar in structure to dopamine, the presence of an additional hydroxyl group makes it toxic to dopaminergic neurons. This compound does not cross the blood-brain barrier (BBB), which necessitates its direct injection into the substantia nigra, medial forebrain bundle, or striatum. The most common use of 6-OHDA is via unilateral injection into the medial forebrain bundle or striatum. Injection of 6-OHDA into the substantia nigra kills approximately 60% of the tyrosine hydrolase (TH)-containing neurons in this area of the rodent brain with subsequent loss of TH-positive terminals in the striatum. The extent of the lesion depends on the amount of 6-OHDA injected, the site of injection, and the species used. This model does not mimic all the clinical features of PD. Dopamine depletion, nigral dopamine cell loss, and neurobehavioral deficits have been successfully achieved using this model, but it does not seem to affect other brain regions such as olfactory structures, lower brain stem areas, or locus coeruleus. Although 6-OHDA does not produce or induce proteinaceous aggregates or Lewy-like inclusions like those seen in PD, it has been reported that 6-OHDA does interact with α-synuclein (Blandini et al., 2008). 6-OHDA is frequently used as a unilateral injection because bilateral injection of this compound into the striatum produces severe adipsia,aphagia, and death (Ungerstedt, 1971).
MPTP represents the most important and most frequently used parkinsonian toxin applied in animal studies. It was shown to replicate almost all the hallmarks of PD including oxidative stress, ROS, energy failure, and in flammation. MPTP is highly lipophilic and rapidly crosses the BBB after systemic administration. Upon entering the brain, MPTP enters astrocytes and is metabolized into 1-methyl-4-phenylpyridinium(MPP+), its active metabolite which is a positively charged molecule, by monoamine oxidase-B. Once released from the astrocytes into the extracellular spaceviathe OCT-3 transporter, MPP+ is taken up into the neuron by the dopamine transporter (DAT) and can be stored in vesicles. Inside the neuron, MPP+ is able to inhibit complex 1 of the mitochondrial electron transport chain, resulting in the release of ROS as well as decreased ATP production. MPP+ stored in vesicles is thought to expel dopamine into the extracellular space where it can be metabolized and subjected to superoxide and hydroxyl radical attack. MPTP is used mainly in nonhuman primates and mice, but has also been used in many other species such as dogs and cats. The MPTP mouse model is employed to study pathological effects of PD, while the MPTP monkey model is used mainly to study behavioral and symptomatic components of PD. The data generated by mouse models have led to a better understanding of molecular mechanisms involved in PD. .
In recent years a new generation of animal models of PD based on ectopic expression, overexpression, or intracerebral injection of α-synuclein have emerged (Visanji et al., 2016).Viral vector-mediated α-synuclein overexpression has been employed in rodents and nonhuman primates. Adeno-associated virus (AAV) vectors demonstrate high, maintained delivery of α-synuclein, with Lewy-like pathology, overt dopaminergic degeneration, and a parkinsonian behavioral phenotype in rodents (Koprich et al., 2010, 2011). These models develop inclusions of aggregated α-synuclein and/or α-synuclein-mediated neuronal cell loss replicating pathological hallmarks of PD and contributing to advances in the understanding of pathogenic mechanisms underpinning PD.Ip et al. (2017) showed that human mutated AAV1/2-A53T α-synuclein injected wild type-mice had widespread nigral and striatal expression of vector-delivered A53T α-synuclein.At 10 weeks, in AAV1/2-A53T α-synuclein mice there was a 33% reduction in TH+dopaminergic nigral neurons, 29% de ficit in striatal DAT binding, and 38% reduction in dopamine level. The mouse model has certain advantages, especially it being amenable to genetic manipulation. Transgenic mice expressing α-synuclein have been generated to try to model PD to study α-synuclein pathobiology and investigate novel therapeutics (Magen and Chesselet, 2010; Koprich et al., 2017).
Accumulating evidence indicates that L-type calcium channels are involved in brain diseases such as PD (Ortner and Striessnig, 2016) and contribute to basal metabolic stress in substantia nigra dopaminergic neurons (Sulzer and Surmeier, 2013). Cav1.2 and Cav1.3 L-type calcium channels are expressed in the substantia nigra neurons (Ortner and Striessnig, 2016). They contribute to somatodendritic Ca2+oscillations during autonomous pacemaking or bursting in these cells (Guzman et al., 2009). It is considered that this constant Ca2+load contributes to the vulnerability of substantia nigra neurons to degeneration in PD by enhancing mitochondrial oxidative stress (Guzman et al., 2010). Epidemiological studies show that dihydropyridines, which are antagonists of these channels, reduce the observed risk of PD (Ritz et al., 2010).This finding is surprising given the relatively low affinity of dihydropyridines for the subtype of L-type calcium channel responsible for most of the calcium entry in striatonigral dopaminergic neurons, which is one with a Cav1.3 pore-forming subunit (Sinnegger-Brauns et al., 2009; Surmeier et al., 2011).Mice in which the gene for the Cav1.3 pore-forming subunit was deleted (Cav 1.3 knockout mice) and with impaired voltage-gated Ca2+channel activity have been used to study PD.
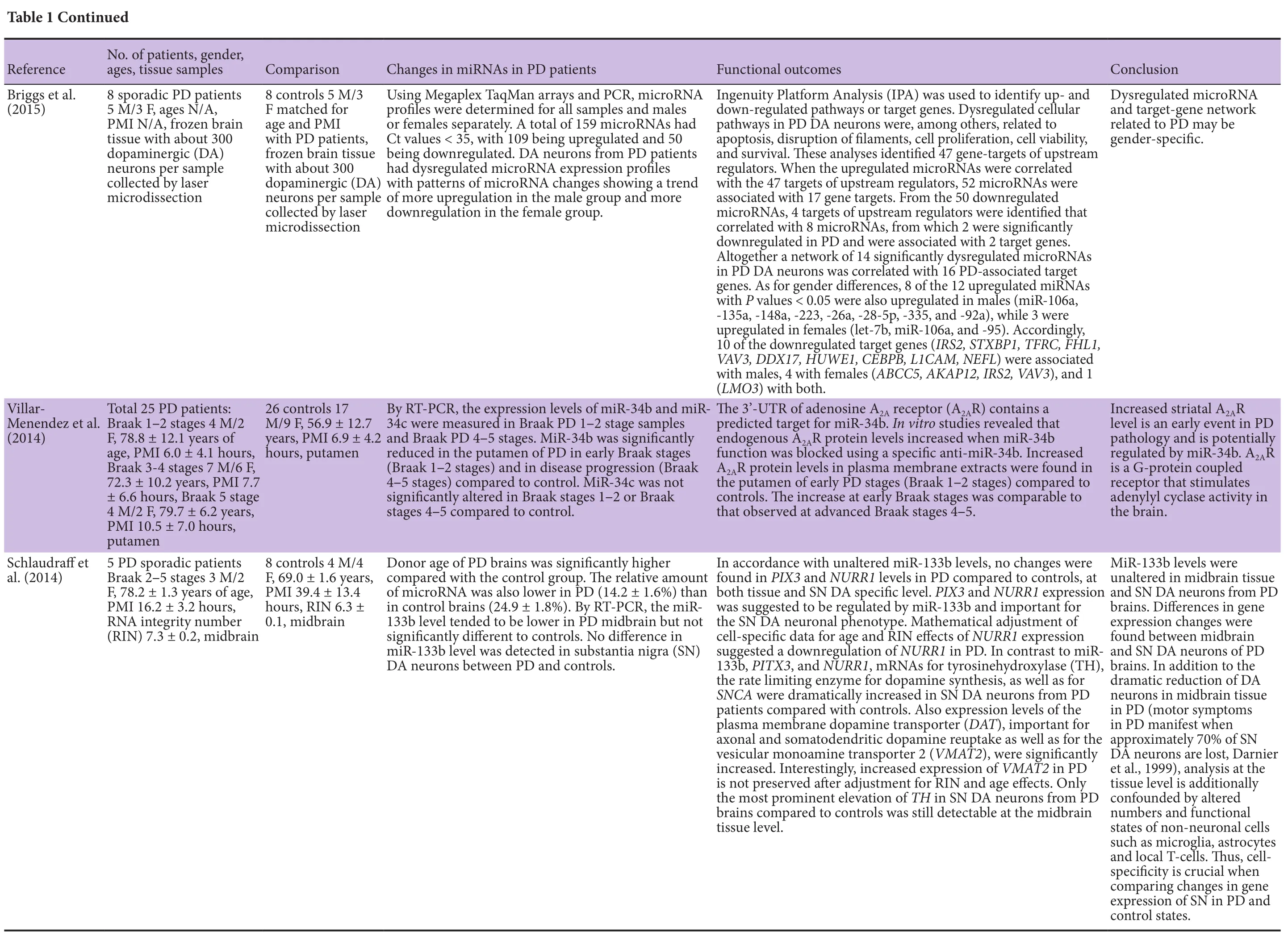
Human studies
Thirteen studies were found and mostly comprised both male and female patients with mean ages ranging from 68 to 80 years (Table 1). Most of the studies indicated that the patients had sporadic PD. The three largest studies were performed on postmortem brain tissue samples from 22 patients (10 male/12 female, mean age 74 years; Tatura et al., 2016), 23 patients (5 male/2 female, Braak stages 1–3, mean age 68 years; 10 male/6 female, Braak stages 4–5, mean age 75 years; Miñones-Moyano et al., 2011) and 25 patients (4 male/2 female, Braak stages 1–2, mean age 79 years; 7 male/6 female, Braak stages 3–4,mean age 72 years; 4 male/2 female, Braak stage 5, mean age 80 years; Villar-Menendez et al., 2014). In the other studies,brain tissues samples were examined from PD patients varying in number from 3 to 20, and although the Braak stages had not been included in most, neuropathological diagnoses of PD had been made according to recognized criteria such as the presence of Lewy bodies and neuronal loss in the substantia nigra. The mean postmortem interval (PMI) for collecting brain tissue samples ranged from 5 to 46 hours.
MicroRNAs upregulated in PD anterior cingulate gyri samples analyzed by RT-PCR were miR-199b, -544a, -488, -221,-144 and those downregulated were miR-7, -145, -543 (Tatura et al., 2016). An analysis of PD putamen samples by NanoS-tring nCounter microRNA assay revealed 6 microRNAs were upregulated, miR-3195, -204-5p, -485-3p, -221-3p, -95, 425-5p, and 7 were downregulated, miR-155-5p, -219-2-3p, -3200-3p, -423-5p, -4421, -421, -382-5p (Nair and Ge, 2016). Using RT-PCR, miR-34b was downregulated in putamen samples of PD patients at Braak stages 1–2 and stages 4–5 (Villar-Menendez et al., 2014). Microarray analysis of PD substantia nigra samples revealed that one microRNA was upregulated, miR-548-d, while 10 were downregulated, miR-198, -485-5p, -339-5p, -208b, -135b, -299-5p, -330-5p, -542-3p, -379, -337-5p.Expression levels of miR-198, -548d, -135b were validated with individual TaqMan assays (Cardo et al., 2014). Also in PD substantia nigra samples, 6 microRNAs were upregulated, miR-21*, -224, -373*, -26b, -106a, -301b, and with similar but milder changes in amygdala samples with a significant upregulation of miR-224 and miR-373*(Alvarez-Erviti et al., 2013). By microarray analysis, 4 microRNAs were upregulated, miR-200b*,-200a*, -195*, -424*, and -7 microRNAs were downregulated,miR-200a, -199a-3p, -148a, -451, -144, -429, -190, in PD frontal cortex samples (Thomas et al., 2012). A signi ficant downregulation of miR-34b and miR-34c occurred in PD amygdala, substantia nigra, and frontal cortex samples (Miñones-Moyano et al., 2011). Interestingly, a signi ficant downregulation was also found in both miR-34b and miR-34c in the amygdala, but not in the frontal cortex, of PD pre-motor cases (Miñones-Moyano et al., 2011). By RT-PCR, miR-133b was downregulated in PD midbrain samples (Kim et al., 2007).
Two of the studies had included PD patients with dementia(PDD) (Cho et al., 2013; Hoss et al., 2016). By RT-PCR, miR-205 was downregulated in PD frontal cortex, and there was no significant difference in the expression level between PD patients and PDD patients. Downregulation of miR-205 also occurred in the PD striatum (Cho et al., 2013). By microRNA sequence analysis, the levels of 64 microRNAs were downregulated whereas the levels of 61 microRNAs were upregulated in PD prefrontal cortex compared to controls, and a set of 29 microRNAs classi fied PD from control brain (93.9% speci ficity, 96.6% sensitivity). 36 microRNAs classi fied PDD from PD without dementia (PDN) (88.9% speci ficity, 81.2% sensitivity).For the majority of differentially expressed microRNAs in PD,PDD samples exhibited larger differences than PDN for the same microRNAs (Hoss et al., 2016). Among the downregulated microRNAs in PD brains were let-7i-3p/5p, miR-184,-1224, -127-5p, and among the upregulated microRNAs was miR-16-5p (Hoss et al., 2016).
In addition, three studies were made on dopaminergic neurons in PD brain tissue samples (Choi et al., 2014; Schlaudraffet al., 2014; Briggs et al., 2015). A widespread expression of miR-7 was shown in dopaminergic neurons in PD substantia nigra (Choi et al., 2014). Also there was no difference in miR-133 level in dopaminergic neurons in PD substantia nigra compared to controls (Schlaudraff et al., 2014). In dopaminergic neurons collected from PD brain tissue, 8 of the 12 upregulated microRNAs were also upregulated in males, miR-106a, -135a,-148a, -223, -26a, -28-5p, -335, -92a, while 3 were upregulated in females, let-7b, miR-106a, -95 (Briggs et al., 2015).
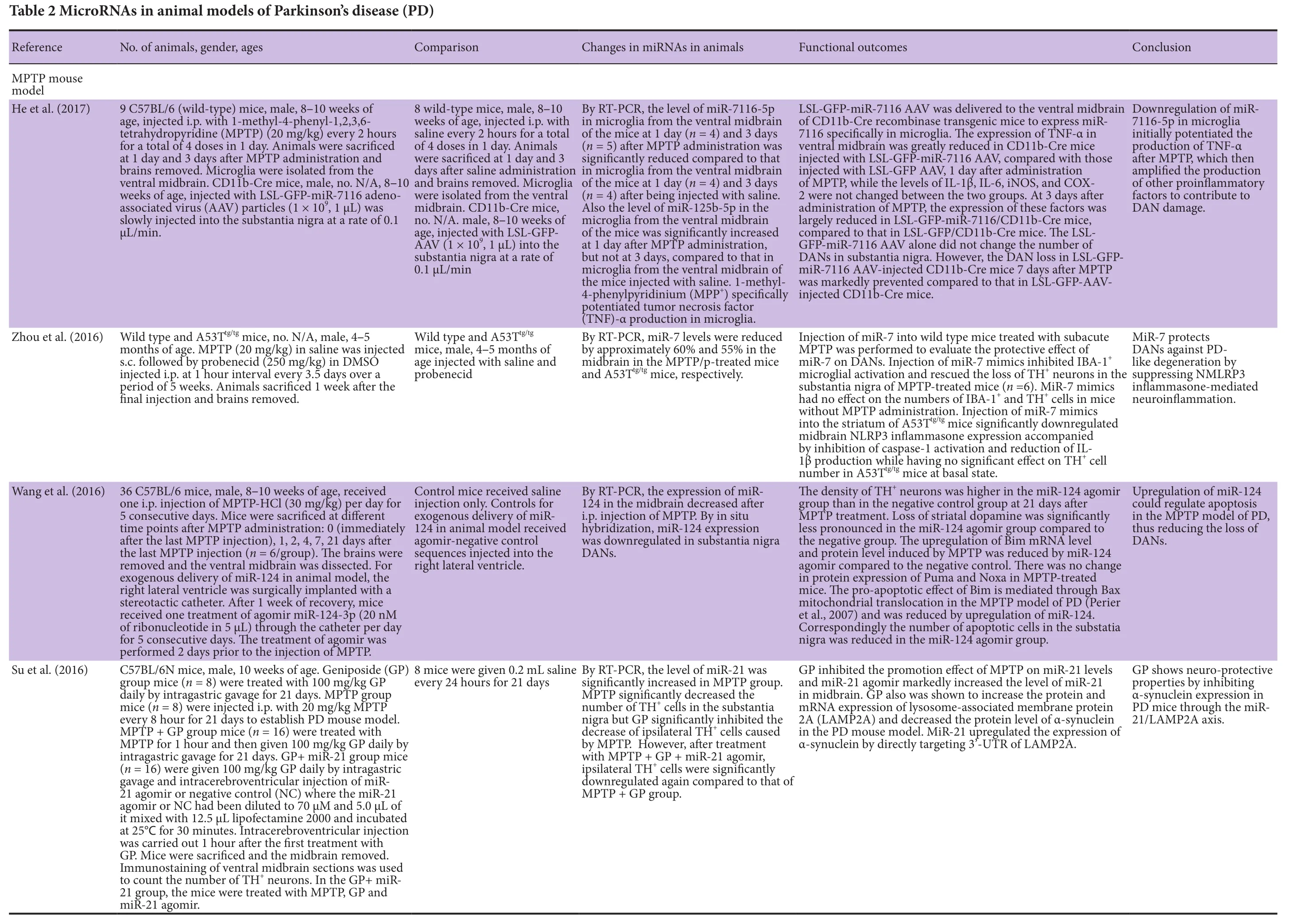
Animal studies
Twelve studies in mice were found and males had been used where the gender was speci fied. Of these studies, 8 had used the MPTP model of PD, 2 the 6-OHDA model, 1 the α-synuclein overexpression model, and 1 the L-type calcium channel Cav1.3 knockout mouse model. The ages of the mice ranged from 6 weeks to 6 months (Table 2).
MPTP model studies
Expression of miR-7116-5p was downregulated while that of miR-125-5p was upregulated in microglia from the ventral midbrain of MPTP-treated mice (He et al., 2017). Also, miR-124 expression was downregulated in substantia nigra dopaminergic neurons following MPTP administration (Wang et al., 2016).
6-OHDA model studies
Mice received a unilateral injection of 6-OHDA 3.75 μg in the medial forebrain bundle (Rivetti di Val Cervo et al., 2017) or 10 μg in the striatum (Saraiva et al., 2016). Treatment of 6-OHDA-treated mice with three transcription factors, NEUROD1, ASCL1 and LMX1A, and the microRNA miR-218, collectively designated NeAL218, reprogrammed astrocytesin vivointo induced dopamine neurons (Rivetti di Val Cervo et al., 2017). MiR-124 nanoparticles (NPs) in mice, receiving a double injection to deliver 6-OHDA into the right striatum and miR-124 NPs into the right lateral ventricle, promoted an increase in migrating neuroblasts and enhanced brain repair (Saraiva et al., 2016).
α-Synuclein overexpression model study
Expression of miR-155 in the substantia nigra was upregulat-ed in mice receiving a unilateral injection of AAV containing α-synuclein into the substantia nigra (Thome et al., 2016).
L-type calcium channel Cav1.3 knockout mouse model studyExpression of miR-204-5p and miR-143-3p was upregulated in the hippocampus of Cav 1.3–/–knockout mice compared to controls (Gstir et al., 2014).
MicroRNAs as Therapeutic Targets for PD
Dysregulated microRNAs in PD brain tissue samples
The human studies have identi fied a large number of microRNAs whose levels were dysregulated in PD brain tissue samples (Table 1). Included among those having downregulated expression were: miR-7, -145, -543 (cingulate gyri); miR-155-5p, -219-2-3p, -3200-3p, -423-5p, -4421, -421, -382-5p, -34b(putamen); miR-198, -485-5p, -339-5p, -208b, -135b, -299-5p,-330-5p, -542-3p, -379, -337-5p, -34b, -34c (substantia nigra);miR- 200a, -199a-3p, -148a, -451, -144, -429, -190, -34b, -34c-205 (frontal cortex); miR-34b, -34c (amygdala); miR-133b(midbrain); miR-205 (striatum); let-7i-3p/5p, miR-184, -1224,-127-5p (prefrontal cortex). Those with upregulated expression were: miR-199b, -544a, -488, -221, -144 (cingulate gyri);miR-3195, -204-5p, -485-3p, -221-3p, -95, 425-5p (putamen);miR-548-d, -21*, -224, -373*, -26b, -106a, -301b (substantia nigra); miR-224, -373*(amygdala); miR-200b*, -200a*, -195*,424*(frontal cortex); miR-16-5p (prefrontal cortex). It would seem that different regions of the PD brain exhibit differently altered microRNA profiles (Figure 1), and this may reflect differences in the numbers and functional states of speci fic cell types present.
Several dysregulated microRNAs may be potential therapeutic targets, but none of the studies had examined the effect of modifying the expression levels of chosen microRNAs in the PD brain. Choi et al. (2014) had suggested that the overexpression of miR-205 may provide an applicable therapeutic strategy to suppress the abnormal upregulation of LRRK2 protein in PD brains. Overexpression could be achieved using a miR-205 agomir or mimic. Also miR-7 protected cells from MPP(+)-induced toxicity in human dopaminergic SH-SY5Y cells (Choi et al., 2014) and the use of a miR-7 agomir may improve PD brain pathophysiology.In vitrotesting using agomirs to downregulated microRNAs or antagomirs to upregulated microRNAs may provide a way of identifying possible microRNAs targets to protect dopaminergic cells exposed to neurotoxins (MPP+ or 6-OHDA).
The animal studies also identi fied several microRNAs whose levels were dysregulated in brain tissues of PD models (Table 2). Included among microRNAs with downregulated expression were: miR-7 (midbrain, ventral midbrain); miR-124(midbrain, substantia nigra); miR-135a-5p. Those with upregulated expression were: miR-21 (midbrain); miR-494, -155(substantia nigra); miR-204-5p, -143-5p (hippocampus). He et al. (2017) found that the level of miR-7116-5p was downregulated while that of miR-125b-5p was upregulated in microglia from the ventral midbrain of MPTP mice. In MPTP model,overexpression of miR-494 by injection of lenti-494 into the substantia nigra exacerbated MPTP-induced neurodegeneration. Reprogramming of striatal astrocytes into induced do-
paminergic neurons occurred on injecting lenti-NeAl218 into the dorsal striatum of 6-OHDA model (Rivetti di Val Cervo et al., 2017). Injection of miR-124 nanoparticles into the lateral ventricle of 6-OHDA model enhanced brain repair (Saraiva et al., 2016). None of the studies reviewed had used agomirs or antagomirs to reverse the levels of downregulated or upregulated microRNAs, respectively, inin vivomouse models of PD or inin vitrowith isolated dopaminergic cells.
Downstream targets of dysregulated microRNAs in brain tissue samples
Downstream targets of several important microRNAs have been indicated in the PD studies reviewed. For example,downregulatedTNFSF13B(TNF superfamily member 13b) is a predicted target of upregulated miR-425-5p andLTA(lymphotoxin alpha) andSLC5A3(soluble carrier family 5 sodium/myo-inositol cotransporter member 3) are predicted targets of upregulated miR-485-3p. The upregulatedPSMB2(proteasome subunit, beta type 2) andGSR(glutathione reductase)are predicted targets of downregulated miR-423-5p and miR-219-3p, respectively (Nair and Ge, 2016).LRRK2(leucine-rich repeat kinase 2) is an experimentally validated target of downregulated miR-1224, andGBA(glucocerebrosidase) is a target of downregulated miR-127-5p and upregulated miR-16-5p(Hoss et al., 2016). DownregulatedLAMP-2A(lysosome-associated membrane protein 2) andHSC(hematopoietic stem cell) are the predicted targets of upregulated miR-26b,-106a, -301b (Alvarez-Erviti et al., 2013). Also the 3’-UTR of transcription factor Ptx3 was identified as a potential target of downregulated miR-133b (Kim et al., 2007). Upregulated miR-21 in PD directly targeted the 3’-UTR of LAMP2A (lysosome-associated membrane protein 2A) (Su et al., 2016), while downregulated miR-135a-5p targeted the 3’-UTR of ROCK2(rho-associated protein kinase 2) (Liu et al., 2016). Upregulated miR-204-5p and miR-143-3p were predicted to target the 3’-UTR of several ion channel mRNAs (Gstir et al., 2014).Also, the 3’-UTR of adenosine A2Areceptor (A2AR) is a predicted target for downregulated miR-34b in PD (Villar-Menendez et al., 2014). Interestingly, dysregulated microRNA and target gene network related to PD may be gender-speci fic(Briggs et al., 2015).
Possible biological implications of some important dysregulated microRNAs in brain tissue samples
?


?


A single microRNA can regulate the expression of hundreds of target genes, so alterations in a panel of microRNAs could greatly affect the pathophysiology and outcome of PD. Use ofin vivoanimal models of PD together within vitrostudies using dopaminergic cells, neural progenitor cells or primary neurons exposed to MPP+ provide a means of testing speci fic microRNAs for protective or adverse effects. For instance,miR-7 was shown to protect dopaminergic neurons from MPP(+)-induced toxicity (Choi et al., 2014), and suppress NLRP3 in flammasone-mediated neuroin flammation in MPTP mouse model (Zhou et al., 2016). Upregulation of miR-205 may provide an applicable therapeutic strategy to suppress the abnormal upregulation of LRRK2 protein in PD brains (Cho et al., 2013). This could be achieved using lenti- or adeno-as-sociated virus containing miR-205 or by a miR-205 agomir.It was proposed that early downregulation of miR-34b/c in PD triggers downstream transcriptome alterations underlying mitochondrial dysfunction and oxidative stress, which ultimately compromise cell viability (Miñones-Moyano et al., 2011).Upregulation of miR-34b/c may be an applicable therapeutic strategy. Also downregulation of miR-7116-5p in microglia initially potentiated the production of TNF-α in MPTP mouse model, which then amplified the production of other proinflammatory factors to contribute to dopaminergic neuron damage (He et al., 2017). Upregulation of miR-7116-5p could be tested in this model to see if it ameliorated neuron damage.The upregulation of pro-apoptotic Bim mRNA level and protein level induced by MPTP was reduced by miR-124 agomir(Wang et al., 2016). Downregulation of miR-135a-5p in MPTP mouse model was associated with an upregulation in ROCK2 that leads to phagocytosis of dopaminergic neurons (Liu et al.,2016). A miR-135a-5p agomir could possibly protect dopaminergic neurons from phagocytosis. Furthermore, the decreased level of miR-7 (Zhou et al., 2016) possibly contributes to increased α-synuclein accumulation and in flammatory response in MPTP mouse model (Junn et al., 2009). In the animal models of PD, downregulated miR-7 and miR-124 (Junn et al., 2009; Kanagaraj et al., 2014; Wang et al., 2016; Zhou et al.,2016) together with upregulated miR-21 and miR-494 (Xiong et al., 2014; Su et al., 2016) are involved in oxidative stress (Xie and Chen, 2016). In PD patients, downregulated miR-7, -34b/c and -205 (Miñones-Moyano et al., 2011; Cho et al., 2013;Villar-Menendez et al., 2014; Tatura et al., 2016) together with upregulated miR-224 (Alvarez-Erviti et al., 2013) are associated with oxidative stress (Xie and Chen, 2016).

Figure 1 Altered expression ofmicroRNAs in Parkinson’s diseasebrain tissues analyzed (based on the human studies reviewed).Upregulated levels of microRNAs areshown in orange; downregulated levels of microRNAs are shown in purple.CG: Cingulate gyri; PUT: putamen; SN:substantia nigra; FC: frontal cortex;PFC: prefrontal cortex; AMYG: amygdala; ST: striatum; MB: midbrain.
Future Perspectives
Currently the diagnosis of patients with PD is mainly made on clinical manifestations of the disease. Molecular imaging allows a window into the pathophysiology of PD, as well as measuring the severity and progression of the disease. The dopamine terminal dysfunction can be demonstrated using positron emission tomography (PET) or single photon emission computed tomography (SPECT) with different tracers, which contribute to early and accurate diagnosis leading to appropriate medications. PET/SPECT imaging, combined with other individual information such as genetic testing, would assist in providing personalized treatment to improve clinical outcomes and minimize adverse effects (Bu et al., 2016). Neuroin flammation ligand imaging the microglial activation might guide the individualized application of non-steroidal anti-in flammatory therapy in PD patients in the future (Stoessl et al., 2011).
Further large-scale studies of brain tissue samples collected with short PMI from human PD patients are warranted to con firm the changes in microRNA expression that have been reported and to test for gender differences. Where gender was speci fied, all of the animal studies had used adult male mice at 6 weeks to 6 months of age. Future studies should be performed with aged animals 22 to 24 months of age. Also both male and female animals should be used, as dysregulated microRNA and target gene network related to PD may be gender-speci fic (Briggs et al., 2015). It has been reported that 50%to 80% of patients with PD have abnormal glucose tolerance that may be further exacerbated by L-dopa therapy (Sandyk, 1993).An observational study concluded that diabetes prevalence was closely similar between patients with PD and subjects without the disease (Becker et al., 2008). In the human studies, it is likely that many of the PD patients would have been taking medication. Animal models of PD should also incorporate possible medications that could have been used such as L-dopa, antidiabetic, antihypertensive, and antihyperlipidemic drugs. A recent clinical trial has shown that exenatide, a medication used for patients with diabetes mellitus type 2, has the potential to modify PD. Patients with sporadic PD aged 25 to 75 years received subcutaneous injections of exenatide 2 mg or placebo once weekly for 48 weeks in addition to their regular medication, followed by a 12-week washout period. Movement disorder was assessed on a rating scale at 60 weeks. Exenatide had positive effects on motor scores in PD that were sustained beyond the period of exposure. Whether exenatide affected the underlying disease pathology is uncertain (Athauda et al., 2017).
Conclusion
This review has shown the expression of a large number of microRNAs to be altered in brain tissue samples of human PD patients and experimental animal models of PD. Some of these altered microRNAs could serve as potential therapeutic targets since modifying the levels of speci fic microRNAs was found to have bene ficial effects in animal models of PD, with improved functional outcomes. For example, miR-124 agomir delivered to the right lateral ventricle in MPTP mouse model increased the density of TH+neurons and reduced the upregulation of Bim mRNA level and protein level induced by MPTP, leading to reduced apoptosis (Wang et al., 2016). The predicted downstream targets of many of the dysregulated microRNAs have also been identi fied, and these included LRRK2, LAMP2A, ROCK2, and several ion channel mRNAs. In flammation and oxidative stress are considered to be chief mediators of PD, with NO playing a key role in the pathogenesis of this neurological disorder. The biological actions of some of the important altered microRNAs may be in regard to these mechanisms.
Author contributions: Bath authors contributed to the study equally.
Con flicts of interest: None declared.
Plagiarism check: Checked twice by iThenticate.
Peer review: Externally peer reviewed.
Open access statement:This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under identical terms.
Open peer reviewer: Cristina Maccallini, University G. d’Annunzio, Italy.
Alvarez-Erviti L, Rodriguez-Oroz MC, Cooper JM, Caballero C, Ferrer I,Obeso JA, Schapira AH (2010) Chaperone-mediated autophagy markers in Parkinson disease brains. Arch Neurol 67:1464-1472.
Alvarez-Erviti L, Seow Y, Schapira AH, Rodriguez-Oroz MC, Obeso JA,Cooper JM (2013) Influence of microRNA deregulation on chaperone-mediated autophagy and alpha-synuclein pathology in Parkinson’s disease. Cell Death Dis 4:e545.
Athauda D, Maclagan K, Skene SS, Bajwa-Joseph M, Letchford D, Chowdhury K, Hibbert S, Budnik N, Zampedri L, Dickson J, Li Y, Aviles-Olmos I, Warner TT, Limousin P, Lees AJ, Greig NH, Tebbs S, Foltynie T (2017)Exenatide once weekly versus placebo in Parkinson’s disease: a randomised, double-blind, placebo-controlled trial. Lancet 390:1664-1675.
Baek D, Villen J, Shin C, Camargo FD, Gygi SP, Bartel DP (2008) The impact of microRNAs on protein output. Nature 455:64-71.
Becker C, Brobert GP, Johansson S, Jick SS, Meier CR (2008) Diabetes in patients with idiopathic Parkinson’s disease. Diabetes Care 31:1808-1812.
Blandini F, Armentero MT, Martignoni E (2008) The 6-hydroxydopamine model: news from the past. Parkinsonism Relat Disord 14 Suppl 2:S124-129.
Blesa J, Phani S, Jackson-Lewis V, Przedborski S (2012) Classic and new animal models of Parkinson’s disease. J Biomed Biotechnol 2012:845618.
Braak H, Ghebremedhin E, Rub U, Bratzke H, Del Tredici K (2004) Stages in the development of Parkinson’s disease-related pathology. Cell Tissue Res 318:121-134.
Braak H, Del Tredici K, Rub U, de Vos RA, Jansen Steur EN, Braak E (2003)Staging of brain pathology related to sporadic Parkinson’s disease. Neurobiol Aging 24:197-211.
Briggs CE, Wang Y, Kong B, Woo TU, Iyer LK, Sonntag KC (2015) Midbrain dopamine neurons in Parkinson’s disease exhibit a dysregulated miRNA and target-gene network. Brain Res 1618:111-121.
Bu LL, Yang K, Xiong WX, Liu FT, Anderson B, Wang Y, Wang J (2016) Toward precision medicine in Parkinson’s disease. Ann Transl Med 4:26.
Cao J, Viholainen JI, Dart C, Warwick HK, Leyland ML, Courtney MJ (2005)The PSD95-nNOS interface: a target for inhibition of excitotoxic p38 stress-activated protein kinase activation and cell death. J Cell Biol 168:117-126.
Cardo LF, Coto E, Ribacoba R, Menéndez M, Moris G, Suárez E, Alvarez V(2014) MiRNA pro file in the substantia nigra of Parkinson’s disease and healthy subjects. J Mol Neurosci 54:830-836.
Ceravolo R, Rossi C, Kiferle L, Bonuccelli U (2010) Nonmotor symptoms in Parkinson’s disease: the dark side of the moon. Future Neurol 5:851-871.
Chmielarz P, Konovalova J, Najam SS, Alter H, Piepponen TP, Er fle H, Sonntag KC, Schutz G, Vinnikov IA, Domanskyi A (2017) Dicer and microRNAs protect adult dopamine neurons. Cell Death Dis 8:e2813.
Cho HJ, Liu G, Jin SM, Parisiadou L, Xie C, Yu J, Sun L, Ma B, Ding J, Vancraenenbroeck R, Lobbestael E, Baekelandt V, Taymans JM, He P, Troncoso JC, Shen Y, Cai H (2013) MicroRNA-205 regulates the expression of Parkinson’s disease-related leucine-rich repeat kinase 2 protein. Hum Mol Genet 22:608-620.
Choi DC, Chae YJ, Kabaria S, Chaudhuri AD, Jain MR, Li H, Mouradian MM, Junn E (2014) MicroRNA-7 protects against 1-methyl-4-phenylpyridinium-induced cell death by targeting RelA. J Neurosci 34:12725-12737.
Damier P, Hirsch EC, Agid Y, Graybiel AM (1999) The substantia nigra of the human brain. II. Patterns of loss of dopamine-containing neurons in Parkinson’s disease. Brain 122:1437-1448.
de Lau LM, Breteler MM (2006) Epidemiology of Parkinson’s disease. Lancet Neurol 5:525-535.
Fearnley JM, Lees AJ (1991) Ageing and Parkinson’s disease: substantia nigra regional selectivity. Brain 114 ( Pt 5):2283-2301.
Gardoni F, Bellone C (2015) Modulation of the glutamatergic transmission by Dopamine: a focus on Parkinson, Huntington and Addiction diseases.Front Cell Neurosci 9:25.
Gstir R, Schafferer S, Scheideler M, Misslinger M, Griehl M, Daschil N,Humpel C, Obermair GJ, Schmuckermair C, Striessnig J, Flucher BE, Hüttenhofer A (2014) Generation of a neuro-speci fic microarray reveals novel differentially expressed noncoding RNAs in mouse models for neurodegenerative diseases. RNA 20:1929-1943.
Guo Z, Geller DA (2014) microRNA and human inducible nitric oxide synthase. Vitam Horm 96:19-27.
Guzman JN, Sánchez-Padilla J, Chan CS, Surmeier DJ (2009) Robust pacemaking in substantia nigra dopaminergic neurons. J Neurosci 29:11011-11019.
Guzman JN, Sanchez-Padilla J, Wokosin D, Kondapalli J, Ilijic E, Schumacker PT, Surmeier DJ (2010) Oxidant stress evoked by pacemaking in dopaminergic neurons is attenuated by DJ-1. Nature 468:696-700.
Ha M, Kim VN (2014) Regulation of microRNA biogenesis. Nat Rev Mol Cell Biol 15:509-524.
He Q, Wang Q, Yuan C, Wang Y (2017) Downregulation of miR-7116-5p in microglia by MPP(+) sensitizes TNF-alpha production to induce dopaminergic neuron damage. Glia 65:1251-1263.
Heinrich TA, da Silva RS, Miranda KM, Switzer CH, Wink DA, Fukuto JM(2013) Biological nitric oxide signalling: chemistry and terminology. Br J Pharmacol 169:1417-1429.
Hoss AG, Labadorf A, Beach TG, Latourelle JC, Myers RH (2016) microRNA Pro files in Parkinson’s Disease Prefrontal Cortex. Front Aging Neurosci 8:36.Ip CW, Klaus LC, Karikari AA, Visanji NP, Brotchie JM, Lang AE, Volkmann J,Koprich JB (2017) AAV1/2-induced overexpression of A53T-alpha-synuclein in the substantia nigra results in degeneration of the nigrostriatal system with Lewy-like pathology and motor impairment: a new mouse model for Parkinson’s disease. Acta Neuropathol Commun 5:11.
Jackson-Lewis V, Blesa J, Przedborski S (2012) Animal models of Parkinson’s disease. Parkinsonism Relat Disord 18 Suppl 1:S183-185.
Junn E, Lee KW, Jeong BS, Chan TW, Im JY, Mouradian MM (2009) Repression of alpha-synuclein expression and toxicity by microRNA-7. Proc Natl Acad Sci U S A 106:13052-13057.
Kanagaraj N, Beiping H, Dheen ST, Tay SS (2014) Downregulation of miR-124 in MPTP-treated mouse model of Parkinson’s disease and MPP iodide-treated MN9D cells modulates the expression of the calpain/cdk5 pathway proteins. Neuroscience 272:167-179.
Kim GH, Kim JE, Rhie SJ, Yoon S (2015) The role of oxidative stress in neurodegenerative diseases. Exp Neurobiol 24:325-340.
Kim J, Inoue K, Ishii J, Vanti WB, Voronov SV, Murchison E, Hannon G,Abeliovich A (2007) A microRNA feedback circuit in midbrain dopamine neurons. Science 317:1220-1224.
Koprich JB, Kalia LV, Brotchie JM (2017) Animal models of alpha-synucleinopathy for Parkinson disease drug development. Nat Rev Neurosci 18:515-529.
Koprich JB, Johnston TH, Reyes MG, Sun X, Brotchie JM (2010) Expression of human A53T alpha-synuclein in the rat substantia nigra using a novel AAV1/2 vector produces a rapidly evolving pathology with protein aggregation, dystrophic neurite architecture and nigrostriatal degeneration with potential to model the pathology of Parkinson’s disease. Mol Neurodegener 5:43.
Koprich JB, Johnston TH, Huot P, Reyes MG, Espinosa M, Brotchie JM (2011)Progressive neurodegeneration or endogenous compensation in an animal model of Parkinson’s disease produced by decreasing doses of alpha-synuclein. PLoS One 6:e17698.
Kordower JH, Olanow CW, Dodiya HB, Chu Y, Beach TG, Adler CH, Halliday GM, Bartus RT (2013) Disease duration and the integrity of the nigrostriatal system in Parkinson’s disease. Brain 136:2419-2431.
Liu Y, Liao S, Quan H, Lin Y, Li J, Yang Q (2016) Involvement of microRNA-135a-5p in the protective effects of hydrogen sul fide against Parkinson’s disease. Cell Physiol Biochem 40:18-26.
Long JM, Ray B, Lahiri DK (2014) MicroRNA-339-5p down-regulates protein expression of β-site amyloid precursor protein-cleaving enzyme 1 (BACE1)in human primary brain cultures and is reduced in brain tissue specimens of Alzheimer disease subjects. J Biol Chem 289:5184-2198.
Maccallini C, Amoroso R (2016) Targeting neuronal nitric oxide synthase as a valuable strategy for the therapy of neurological disorders. Neural Regen Res 11:1731-1734.
Maccallini C, Di Matteo M, Vullo D, Ammazzalorso A, Carradori S, De Filippis B, Fantacuzzi M, Giampietro L, Pandol fiA, Supuran CT, Amoroso R(2016) Indazole, pyrazole, and oxazole derivatives targeting nitric oxide synthases and carbonic anhydrases. Chem Med Chem 11:1695-1699.
Magen I, Chesselet MF (2010) Genetic mouse models of Parkinson’s diseaseThe state of the art. Prog Brain Res 184:53-87.
Marsden CD (1990) Parkinson’s disease. Lancet 335:948-952.
Miñones-Moyano E, Porta S, Escaramís G, Rabionet R, Iraola S, Kagerbauer B,Espinosa-Parrilla Y, Ferrer I, Estivill X, Martí E (2011) MicroRNA pro filing of Parkinson’s disease brains identi fies early downregulation of miR-34b/c which modulate mitochondrial function. Hum Mol Genet 20:3067-3078.
Nair VD, Ge Y (2016) Alterations of miRNAs reveal a dysregulated molecular regulatory network in Parkinson’s disease striatum. Neurosci Lett 629:99-104.
Noyce AJ, Lees AJ, Schrag AE (2016) The prediagnostic phase of Parkinson’s disease. J Neurol Neurosurg Psychiatry. 2016;87(8):871-878.
Nuytemans K, Theuns J, Cruts M, Van Broeckhoven C (2010) Genetic etiology of Parkinson disease associated with mutations in the SNCA, PARK2, PINK1,PARK7, and LRRK2 genes: a mutation update. Hum Mutat 31:763-780.
Ortner NJ, Striessnig J (2016) L-type calcium channels as drug targets in CNS disorders. Channels (Austin) 10:7-13.
Perier C, Bové J, Wu DC, Dehay B, Choi DK, Jackson-Lewis V, Rathke-Hartlieb S, Bouillet P, Strasser A, Schulz JB, Przedborski S, Vila M (2007) Two molecular pathways initiate mitochondria-dependent dopaminergic neurodegeneration in experimental Parkinson’s disease. Proc Natl Acad Sci U S A 104:8161-8166.
Ritz B, Rhodes SL, Qian L, Schernhammer E, Olsen JH, Friis S (2010) L-type calcium channel blockers and Parkinson disease in Denmark. Ann Neurol 67:600-606.
Rivetti di Val Cervo P, Romanov RA, Spigolon G, Masini D, Martín-Montañez E, Toledo EM, La Manno G, Feyder M, Pi flC, Ng Y-H, Sánchez SP,Linnarsson S, Wernig M, Harkany T, Fisone G, Arenas E (2017) Induction of functional dopamine neurons from human astrocytes in vitro and mouse astrocytes in a Parkinson’s disease model. Nat Biotechnol 35:444.
Rocha NP, de Miranda AS, Teixeira AL (2015) Insights into neuroin flammation in Parkinson’s disease: from biomarkers to anti-in flammatory based therapies. Biomed Res Int 2015:628192.
Ross GW, Petrovitch H, Abbott RD, Nelson J, Markesbery W, Davis D, Hardman J, Launer L, Masaki K, Tanner CM, White LR (2004) Parkinsonian signs and substantia nigra neuron density in decendents elders without PD.Ann Neurol 56:532-539.
Sandyk R (1993) The relationship between diabetes mellitus and Parkinson’s disease. Int J Neurosci 69:125-130.
Saraiva C, Paiva J, Santos T, Ferreira L, Bernardino L (2016) MicroRNA-124 loaded nanoparticles enhance brain repair in Parkinson’s disease. J Control Release 235:291-305.
Schapira AHV, Chaudhuri KR, Jenner P (2017) Non-motor features of Parkinson disease. Nat Rev Neurosci 18:435-450.
Schlaudraff F, Grundemann J, Fauler M, Dragicevic E, Hardy J, Liss B (2014)Orchestrated increase of dopamine and PARK mRNAs but not miR-133b in dopamine neurons in Parkinson’s disease. Neurobiol Aging 35:2302-2315.
Sharma JN, Al-Omran A, Parvathy SS (2007) Role of nitric oxide in in flammatory diseases. In flammopharmacology 15:252-259.
Shulman JM, De Jager PL, Feany MB (2011) Parkinson’s disease: genetics and pathogenesis. Annu Rev Pathol 6:193-222.
Sierzega M, Kaczor M, Kolodziejczyk P, Kulig J, Sanak M, Richter P (2017)Evaluation of serum microRNA biomarkers for gastric cancer based on blood and tissue pools pro filing: the importance of miR-21 and miR-331.Br J Cancer 117:266-273.
Sinnegger-Brauns MJ, Huber IG, Koschak A, Wild C, Obermair GJ, Einzinger U, Hoda JC, Sartori SB, Striessnig J (2009) Expression and 1,4-dihydropyridine-binding properties of brain L-type calcium channel isoforms. Mol Pharmacol 75:407-414.
Stoessl AJ, Martin WW, McKeown MJ, Sossi V (2011) Advances in imaging in Parkinson’s disease. Lancet Neurol 10:987-1001.
Su C, Yang X, Lou J (2016) Geniposide reduces alpha-synuclein by blocking microRNA-21/lysosome-associated membrane protein 2A interaction in Parkinson disease models. Brain Res 1644:98-106.
Sulzer D, Surmeier DJ (2013) Neuronal vulnerability, pathogenesis, and Parkinson’s disease. Mov Disord 28:41-50.
Sun HX, Zeng DY, Li RT, Pang RP, Yang H, Hu YL, Zhang Q, Jiang Y, Huang LY, Tang YB, Yan GJ, Zhou JG (2012) Essential role of microRNA-155 in regulating endothelium-dependent vasorelaxation by targeting endothelial nitric oxide synthase. Hypertension 60:1407-1414.
Surmeier DJ, Guzman JN, Sanchez-Padilla J, Goldberg JA (2011) The origins of oxidant stress in Parkinson’s disease and therapeutic strategies. Antioxid Redox Signal 14:1289-1301.
Tatura R, Kraus T, Giese A, Arzberger T, Buchholz M, Hoglinger G, Muller U(2016) Parkinson’s disease:SNCA-,PARK2-, andLRRK2- targeting microRNAs elevated in cingulate gyrus. Parkinsonism Relat Disord 33:115-121.
Thomas B, Beal MF (2007) Parkinson’s disease. Hum Mol Genet 16 Spec No.2:R183-194.
Thomas RR, Keeney PM, Bennett JP (2012) Impaired complex-I mitochondrial biogenesis in Parkinson disease frontal cortex. J Parkinsons Dis 2:67-76.
Thome AD, Harms AS, Volpicelli-Daley LA, Standaert DG (2016) microRNA-155 regulates alpha-synuclein-induced in flammatory responses in models of Parkinson disease. J Neurosci 36:2383-2390.
Ungerstedt U (1971) Adipsia and aphagia after 6-hydroxydopamine induced degeneration of the nigro-striatal dopamine system. Acta Physiol Scand Suppl 367:95-122.
Valente AX, das Neves RP, Oliveira PJ (2012) Epigenetic engineering to reverse the Parkinson’s expression state. Parkinsonism Relat Disord 18:717-721.
Villar-Menendez I, Porta S, Buira SP, Pereira-Veiga T, Díaz-Sánchez S, Albasanz JL, Ferrer I, Martin M, Barrachina M (2014) Increased striatal adenosine A2A receptor levels is an early event in Parkinson’s disease-related pathology and it is potentially regulated by miR-34b. Neurobiol Dis 69:206-214.
Visanji NP, Brotchie JM, Kalia LV, Koprich JB, Tandon A, Watts JC, Lang AE(2016) alpha-Synuclein-based animal models of Parkinson’s disease: challenges and opportunities in a new era. Trends Neurosci 39:750-762.
Wang H, Ye Y, Zhu Z, Mo L, Lin C, Wang Q, Wang H, Gong X, He X, Lu G,Lu F, Zhang S (2016) MiR-124 regulates apoptosis and autophagy process in MPTP model of Parkinson’s disease by targeting to Bim. Brain Pathol 26:167-176.
Winklhofer KF, Haass C (2010) Mitochondrial dysfunction in Parkinson’s disease. Biochim Biophys Acta 1802:29-44.
Xie Y, Chen Y (2016) microRNAs: emerging targets regulating oxidative stress in the models of Parkinson’s disease. Front Neurosci 10:298.
Xiong R, Wang Z, Zhao Z, Li H, Chen W, Zhang B, Wang L, Wu L, Li W,Ding J, Chen S (2014) MicroRNA-494 reduces DJ-1 expression and exacerbates neurodegeneration. Neurobiol Aging 35:705-714.
Xue Y, Ouyang K, Huang J, Zhou Y, Ouyang H, Li H, Wang G, Wu Q, Wei C, Bi Y, Jiang L, Cai Z, Sun H, Zhang K, Zhang Y, Chen J, Fu XD (2013)Direct conversion of fibroblasts to neurons by reprogramming PTB-regulated microRNA circuits. Cell 152:82-96.
Zhou Y, Lu M, Du RH, Qiao C, Jiang CY, Zhang KZ, Ding JH, Hu G (2016)MicroRNA-7 targets Nod-like receptor protein 3 in flammasome to modulate neuroin flammation in the pathogenesis of Parkinson’s disease. Mol Neurodegener 11:28.
Zhu JH, Gusdon AM, Cimen H, Van Houten B, Koc E, Chu CT (2012)Impaired mitochondrial biogenesis contributes to depletion of functional mitochondria in chronic MPP+ toxicity: dual roles for ERK1/2.Cell Death Dis 3:e312.
How to cite this article:Martinez B, Peplow PV (2017) MicroRNAs in Parkinson’s disease and emerging therapeutic targets. Neural Regen Res 12(12):1945-1959.
*Correspondence to:Philip V. Peplow, Ph.D.,phil.peplow@otago.ac.nz.
orcid:0000-0001-5468-1989(Philip V. Peplow)
10.4103/1673-5374.221147
2017-12-05
injection(s) of MPTP 20 mg/kg or 30 mg/kg over a period ranging from 1 to 21 days (for mice aged 6–12 weeks)or 5 weeks (for mice aged 4–5 months), and sacri ficed at chosen time points after the last MPTP injection (if several injections were given). Many of the studies identified downregulation of speci fic microRNAs in brain tissue collected from these animals.Expression of miR-7 in the midbrain of MPTP-treated mice was downregulated compared to controls (Junn et al., 2009; Zhou et al., 2016). Similarly, following MPTP administration, miR-124 was downregulated in the ventral midbrain (Wang et al., 2016)and substantia nigra (Kanagaraj et al., 2014). Also, downregulation of miR-135a-5p was found in the brain tissue of mice after administering MPTP (Liu et al., 2016). By contrast, Su et al. (Su et al., 2016) found that miR-21 was upregulated in midbrain of MPTP-treated mice compared to controls. Xiong et al. (Xiong et al., 2014) showed that miR-494 was expressed highly in the substantia nigra of MPTP-treated mice and that overexpression of miR-494, induced by injecting lentivirus containing miR-494 into the substantia nigra, exacerbated MPTP-induced neurodegeneration, with a loss of dopaminergic neurons.
- 中国神经再生研究(英文版)的其它文章
- Roles of neural stem cells in the repair of peripheral nerve injury
- Conductive polymer scaffolds to improve neural recovery
- The contribution of oligodendrocytes and oligodendrocyte progenitor cells to central nervous system repair in multiple sclerosis: perspectives for remyelination therapeutic strategies
- Surgical reconstruction of spinal cord circuit provides functional return in humans
- Environmental cues determine the fate of astrocytes after spinal cord injury
- Formin’ bridges between microtubules and actin filaments in axonal growth cones