FOXA1与AMACR/P504s在前列腺癌中的表达及其临床意义
张继君 石晓欣 陶丽丽 陈耀丽 赵昌林

[摘要]目的 探討叉头盒A1(FOXA1)及AMACR/P504s在前列腺癌中的表达及其临床意义。方法 收集2014年1月~2018年10月北京大学深圳医院及深圳市第二人民医院经病理确诊的49例原发性前列腺癌标本及8例前列腺癌骨转移标本。采用免疫组化EnVision法检测前列腺癌组织中FOXA1及AMACR/P504s的蛋白表达,分析FOXA1和AMACR/P504s的表达情况。结果 FOXA1在前列腺癌转移标本中的阳性率为62.5%(5/8),低于原发性前列腺癌的93.9%(46/49),差异有统计学意义(P<0.05)。AMACR/P504s在前列腺癌转移标本中的阳性率为75.0%(6/8),与原发性前列腺癌的83.7%(41/49)比较,差异无统计学意义(P>0.05)。原发性前列腺癌:T分期中,T3~4期的FOXA1阳性表达率为67.3%,显著高于T2a~c期的26.5%,差异有统计学意义(P<0.05);Gleason评分中,7~10分的FOXA1阳性表达率为77.6%,显著高于6分的16.3%,差异有统计学意义(P<0.05);有脉管浸润的FOXA1阳性表达率为14.3%,显著低于无脉管浸润的79.6%,差异有统计学意义(P<0.05);不同年龄、神经束侵犯情况下的FOXA1阳性表达率比较,差异无统计学意义(P>0.05);不同T分期、Gleason评分、年龄、脉管浸润以及神经束侵犯情况下的AMACR/P504s阳性表达率比较,差异无统计学意义(P>0.05)。结论 FOXA1和AMACR/P504s是前列腺癌良好的标志物,FOXA1高表达提示预后差。
[关键词]前列腺癌;叉头盒;AMACR/P504s
[中图分类号] R737.25 [文献标识码] A [文章编号] 1674-4721(2019)9(b)-0007-04
Expression and clinical significance of FOXA1 and AMACR/P504s in prostate cancer
ZHANG Ji-jun1 SHI Xiao-xin2 TAO Li-li2 CHEN Yao-li2▲ ZHAO Chang-lin3
1. Department of Pathology, Nanshan District People′s Hospital of Shenzhen City, Guangdong Province, Shenzhen 518000, China; 2. Department of Pathology, Peking University Shenzhen Hospital, Guangdong Province, Shenzhen 518036, China; 3. Department of Oncology, Guangzhou University of Chinese Medicine Clifford Hospital, Guangdong Province, Guangzhou 511495, China
[Abstract] Objective To investigate the expression and clinical significance of FOXA1 and AMACR/P504s in prostate cancer. Methods A total of 49 specimens of primary prostate cancer and 8 specimens of bone metastases from prostate cancer confirmed by pathology were collected from Peking University Shenzhen Hospital and Shenzhen Second People′s Hospital from January 2014 to October 2018. Immunohistochemical EnVision method was used to detect the protein expression of FOXA1 and AMACR/P504s in prostate cancer tissues, and the expression of FOXA1 and AMACR/P504s was analyzed. Results The positive rate of FOXA1 in prostate cancer metastasis specimens was 62.5% (5/8), which was lower than that of primary prostate cancer accounting for 93.9% (46/49), and the difference was statistically significant (P<0.05). The positive rate of AMACR/P504s in prostate cancer metastasis specimens was 75.0% (6/8), compared with 83.7% (41/49) of primary prostate cancer, and the difference was not statistically significant (P>0.05). Primary prostate cancer: in the T stage, the positive expression rate of FOXA1 in T3-4 stage was 67.3%, which was significantly higher than that in T2a-c stage for 26.5%, and the difference was statistically significant (P<0.05). In the Gleason score, the positive expression rate of FOXA1 at 7-10 points was 77.6%, which was significantly higher than that of 6 points for 16.3%, and the difference was statistically significant (P<0.05). The positive expression rate of FOXA1 in vascular infiltration was 14.3%, which was significantly lower than that of no vessel infiltration (79.6%), and the difference was statistically significant (P<0.05). There was no significant difference in the positive expression rate of FOXA1 in different ages and nerve bundle intrusion (P>0.05). There was no significant difference in the positive expression rate of AMACR/P504s in different T stages, Gleason scores, ages, vascular infiltration and nerve bundle intrusion (P>0.05). Conclusion FOXA1 and AMACR/P504s are good markers for prostate cancer, and high expression of FOXA1 suggests poor prognosis.
[Key words] Prostate cancer; FOXA1;AMACR/P504s
前列腺癌是发达国家男性常见的恶性肿瘤[1-2],在我国的发病率也迅速升高,其肿瘤进展的分子学机制尚不完全清楚。AMACR酶参与过氧化物酶体-氧化支链脂肪酸及其衍生物的代谢,已经发现AMACR/P504s在前列腺癌组织内其mRNA及蛋白均升高。叉头盒A1(FOXA1)又被稱为肝细胞核因子3a(HNF3a),是FOX家族转录因子成员[3],能够与非转录状态的染色体结合,提高转录起始因子的基因表达及转录效率,从而调节下游基因的表达[4]。研究表明,FOXA1在多种癌症中高表达,包括涎腺导管癌[5]、非小细胞肺癌[6]、食管癌[7]、甲状腺癌[8]及乳腺癌[9-10]。FOXA因子在器官包括前列腺[11-12]的发育中具有重要作用,可影响前列腺癌的增殖和激素应答[13-14]。本研究通过免疫组化EnVision法检测FOXA1与AMACR/P504s在原发性及转移性前列腺癌组织中的表达,分析其与临床的关系,评估FOXA1与AMACR/P504s在前列腺癌预后的价值,现报道如下。
1资料与方法
1.1一般资料
收集2014年1月~2018年10月北京大学深圳医院及深圳市第二人民医院经病理确诊的49例原发性前列腺癌标本及8例前列腺癌骨转移标本。49例原发性前列腺癌标本取材前均无化疗或放疗病史。57例患者,年龄52~79岁,平均(67.4±14.4)岁;<64岁20例,≥64岁37例;病理类型:前列腺腺癌56例,前列腺小细胞癌1例。原发性前列腺癌中,T分期:T2a~c 14例,T3~4 35例;Gleason评分:6分11例,7分16例,8~10分22例;年龄:<64岁19例,≥64岁30例;脉管浸润:有7例,无42例;神经束侵犯:有28例,无21例。
1.2方法
标本采用10%中性福尔马林固定,经脱水、石蜡包埋,4 μm厚度切片及免疫组化EnVision两步法检测。FOXA1和AMACR/P504s分别为鼠抗、兔抗人单克隆抗体,均购于福州迈新公司。具体操作步骤按照试剂盒说明书进行,其中AMACR/P504s为即用型试剂,FOXA1为浓缩液抗体,稀释浓度为1:100。PBS代替一抗作为空白对照,采用DAB显色,苏木精对比染色。
1.3结果判定标准
FOXA1蛋白在细胞核表达。AMACR/P504s阳性染色为弥漫性或粒状、胞浆性或腔内染色。AMACR/P504s在相邻的良性腺体如有染色,可见部分弱染色[15]。阴性染色属于无染色或局灶性、弱的非腔缘细颗粒染色,对染色强度及阳性细胞百分数分别进行评判。①按阳性肿瘤细胞百分数评分:阳性细胞数占1%~10%为1分;11%~50%为2分;51~80%为3分;81%~100%为4分。②按染色强度评分:阴性为0分;弱阳性为1分;中度阳性为2分;强阳性为3分。将两项得分之积作为最终得分,总分为0~12分,其中0分为阴性,其余均为阳性[16]。
1.4统计学方法
采用SPSS 19.0统计学软件进行数据分析,计量资料用均数±标准差(x±s)表示,两组间比较采用t检验;计数资料采用率表示,组间比较采用χ2检验或Fisher精确检验,以P<0.05为差异有统计学意义。
2结果
2.1 FOXA1和AMACR/P504s在原发性前列腺癌中的表达情况
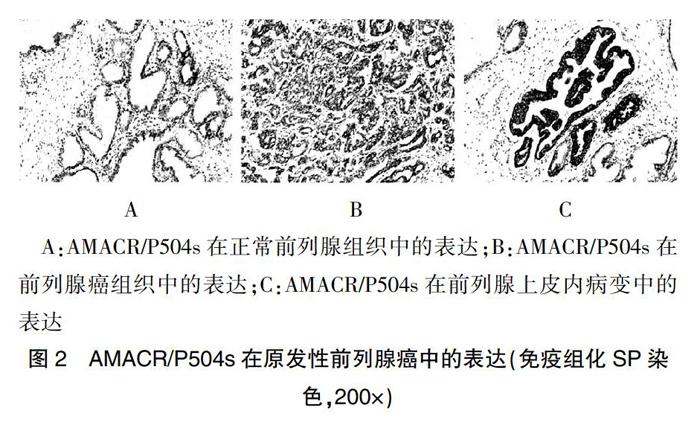
FOXA1仅存在于上皮细胞细胞核,在正常和肿瘤组织间质中均未观察到免疫反应。肿瘤旁前列腺周围带组织内有弱至中等程度表达,肿瘤旁前列腺移行带组织内FOXA1蛋白几乎不表达(图1A);AMACR/P504s在肿瘤旁正常前列腺组织不表达(图2A),FOXA1与AMACR/P504s蛋白在前列腺癌及前列腺上皮内病变均有表达(图1B~C、图2B~C)。FOXA1与AMACR/P504s在原发性前列腺癌中的阳性率分别为93.9%(46/49)和83.7%(41/49),两者的阳性率比较,差异无统计学意义(P>0.05)。
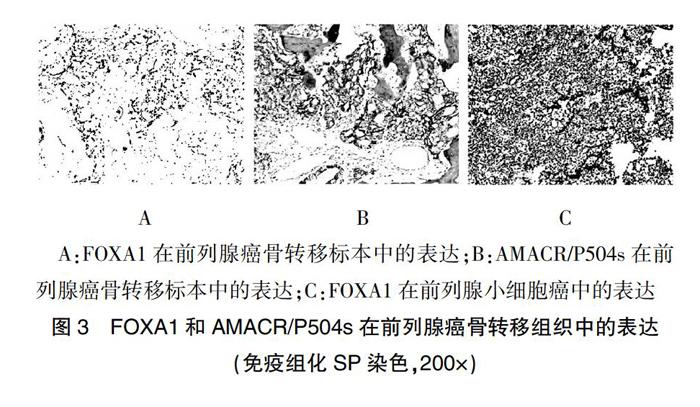
2.2 FOXA1和AMACR/P504s在前列腺癌骨转移组织中的表达情况
FOXA1在前列腺癌转移标本中的阳性率为62.5%(5/8)(图3A),低于原发性前列腺癌的93.9%(46/49),差异有统计学意义(P<0.05);AMACR/P504s在前列腺癌转移标本中的阳性率为75.0%(6/8)(图3B),与原发性前列腺癌的83.7%(41/49)比较,差异无统计学意义(P>0.05);FOXA1蛋白在前列腺小细胞癌中表达较强(图3C)。
2.3 FOXA1和AMACR/P504s在原发性前列腺癌组织不同病理参数情况下的表达
T分期中,T3~4期的FOXA1阳性表达率为67.3%,显著高于T2a~c期的26.5%,差异有统计学意义(P<0.05);Gleason评分中,7~10分的FOXA1阳性表达率为77.6%,显著高于6分的16.3%,差异有统计学意义(P<0.05);有脉管浸润的FOXA1阳性表达率为14.3%,显著低于无脉管浸润的79.6%,差异有统计学意义(P<0.05);不同年龄、神经束侵犯情况下的FOXA1阳性表达率比较,差异无统计学意义(P>0.05);不同T分期、Gleason评分、年龄、脉管浸润以及神经束侵犯情况下的AMACR/P504s阳性表达率比较,差异无统计学意义(P>0.05)(表1)。
3讨论
FOXA1和AMACR/P504s可以作为前列腺癌病理诊断的标志物。FOXA1具有调节类固醇激素受体转活化的功能,是前列腺上皮分化所必需的转录因子[17]。小鼠模型研究表明FOXA1在前列腺上皮内瘤变和前列腺腺癌中的表达持续上调[18]。本研究结果提示,FOXA1在前列腺癌及前列腺上皮内病变中表达均上调,AMACR/P504s在前列腺癌及其上皮内病变组织内高表达[19-21],FOXA1与AMACR/P504s在原发性前列腺癌中的阳性率比较,差异无统计学意义(P>0.05)。两种蛋白在前列腺癌的诊断中各有优缺点,一方面AMACR/P504s的特异性高于FOXA1,在正常前列腺组织中几乎不表达,在前列腺癌中高表达;而FOXA1除了在前列腺癌中高表达,在正常前列腺周围带组织内也有一定的表达。本研究共选择57例前列腺癌组织(包括原发性及前列腺癌转移标本),联合应用FOXA1与AMACR/P504s两种标志物的诊断率达100.0%,尤其是联合应用这两种抗体对鉴别诊断转移性前列腺癌与其他来源肿瘤具有非常重要的临床意义。FOXA1蛋白表达在肿瘤细胞胞核,而AMACR/P504s蛋白表达在肿瘤细胞胞浆,两种蛋白的表达模式有利于应用鸡尾酒染色法同时标记肿瘤细胞。两者可作为前列腺癌诊断的标志物。
FOXA1高表達提示疾病分期晚、恶性程度高、预后差。本研究结果显示,不同T分期、Gleason评分、脉管浸润情况下的FOXA1阳性表达率比较,差异有统计学意义(P<0.05);不同年龄、神经束侵犯情况下的FOXA1阳性表达率比较,差异无统计学意义(P>0.05);不同T分期、Gleason评分、年龄、脉管浸润以及神经束侵犯情况下的AMACR/P504s阳性表达率比较,差异无统计学意义(P>0.05)。提示Gleason评分高、T分期晚,FOXA1表达越强,FOXA1有可能成为一种新的治疗靶点。
综上所述,FOXA1和AMACR/P504s是前列腺癌良好的标志物。FOXA1高表达提示预后差。本研究缺乏去势抵抗性前列腺癌(CRPC)标本,尚不清楚FOXA1与AMACR/P504s在这一类肿瘤中表达情况,有待进一步的研究。
[参考文献]
[1]Siegel RL,Miller KD,Jemal A.Cancer statistics,2019[J].CA Cancer J Clin,2019,69(1):7-34.
[2]Boyle P,Brawley OW.Prostate cancer:current evidence weighs against population screening[J].CA Cancer J Clin,2009,59(4):220-224.
[3]Laissue P.The forkhead-box family of transcription factors:key molecular players in colorectal cancer pathogenesis[J].Mol Cancer,2019,18(1):5.
[4]Yamaguchi N,Nakayama Y,Yamaguchi N.Down-regulation of Forkhead box protein A1(FOXA1)leads to cancer stem cell-like properties in tamoxifen-resistant breast cancer cells through induction of interleukin-6[J].J Biol Chem,2017,292(20):8136-8148.
[5]Urano M,Hirai H,Tada Y,et al.The high expression of FOXA1 is correlated with a favourable prognosis in salivary duct carcinomas:a study of 142 cases[J].Histopathology,2018,73(6):943-952.
[6]Zhang X,Wang L,Liu Y,et al.MiR-760 enhances TRAIL sensitivity in non-small cell lung cancer via targeting the protein FOXA1[J].Biomed Pharmacother,2018,99:523-529.
[7]Xu Y,Wang W,Li L,et al.FOXA1 and CK7 expression in esophageal squamous cell carcinoma and its prognostic significance[J].Neoplasma,2018,65(3):469-476.
[8]Nonaka D.A study of FoxA1 expression in thyroid tumors[J].Hum Pathol,2017,65:217-224.
[9]Shou J,Lai Y,Xu J,et al.Prognostic value of FOXA1 in breast cancer:A systematic review and meta-analysis[J].Breast,2016,27(6):35-43.
[10]Yu X,Zhang Z,Wang Z,et al.Prognostic and predictive value of tumor-infiltrating lymphocytes in breast cancer:a systematic review and meta-analysis[J].Clin Transl Oncol,2016,18(5):497-506.
[11]Kaestner KH.The FoxA factors in organogenesis and differentiation[J].Curr Opin Genet Dev,2010,20(5):527-532.
[12]Sun Q,Yu XP,Degraff DJ,et al.Upstream stimulatory factor 2,a novel FoxA1-interacting protein,is involved in prostate-specific gene expression[J].Mol Endocrinol,2009,23(12):2038-2047.
[13]Zhao Y,Tindall DJ,Huang H.Modulation of androgen receptor by FOXA1 and FOXO1 factors in prostate cancer[J].Int J Biol Sci,2014,10(6):614-619.
[14]Gerhardt J,Montani M,Wild P,et al.FOXA1 promotes tumor progression in prostate cancer and represents a novel hallmark of castration-resistant prostate cancer[J].Am J Pathol,2012,180(2):848-861.
[15]Kumaresan K,Kakkar N,Verma A,et al.Diagnostic utility of α-methylacyl CoA racemase (P504S) & HMWCK in morphologically difficult prostate cancer[J].Diagn Pathol,2010, 5(1):83.
[16]Yan Q,Zhang XR,Zhang Z,et al.Prevalence of protein C receptor(PROCR)is associated with inferior clinical outcome in Breast invasive ductal carcinoma[J].Pathol Res Pract,2017,213(9):1173-1179.
[17]Kim J,Jin H,Zhao JC,et al.FOXA1 inhibits prostate cancer neuroendocrine differentiation[J].Oncogene,2017,36(28):4072-4080.
[18]Mirosevich J,Gao N,Gupta A,et al.Expression and role of Foxa proteins in prostate cancer[J].Prostate,2006,66(10):1013-1028.
[19]Jain D,Gupta S,Marwah N,et al.Evaluation of role of alpha-methyl acyl-coenzyme A racemase/P504S and high molecular weight cytokeratin in diagnosing prostatic lesions[J].J Cancer Res Ther,2017,13(1):21-25.
[20]Luo J,Zha S,Gage WR,et al.Alpha-methylacyl-CoA racemase:a new molecular marker for prostate cancer[J].Cancer Res,2002,62(8):2220-2226.
[21]Wu CL,Yang XJ,Tretiakova M,et al.Analysis of alpha-methylacyl-CoA racemase (P504S) expression in high-grade prostatic intraepithelial neoplasia[J].Hum Pathol,2004,35(8):1008-1013.
(收稿日期:2019-03-06 本文編辑:任秀兰)