Cholangiocarcinoma after flow diversion surgery for congenital biliary dilatation:A case report and review of literature
Ryo Ataka,Takashi Ito,Toshihiko Masui,Satoru Seo,Takamichi Ishii,Satoshi Ogiso,Shintaro Yagi,Kojiro Taura,Shinji Uemoto
Ryo Ataka,Takashi Ito,Toshihiko Masui,Satoru Seo,Takamichi Ishii,Satoshi Ogiso,Shintaro Yagi,Kojiro Taura,Shinji Uemoto,Department of Hepato-Biliary-Pancreatic Surgery and Transplantation,Graduate School of Medicine,Kyoto University,Kyoto 606-8507,Japan
Abstract
Key words:Congenital biliary dilatation;Pancreaticobiliary maljunction;Cholangiocarcinoma;Recurrence;Metachronous neoplasm;Case report
INTRODUCTION
Pancreaticobiliary maljunction(PBM)is an uncommon congenital anomaly defined as junction of the pancreatic and bile ducts outside the duodenal wall,allowing reciprocal reflux of pancreatic juice and bile,which is carcinogenic.Thus,PBM is a high-risk factor for biliary tract cancer,and preventive surgery is necessary.Congenital biliary dilatation(CBD),one type of PBM,is usually treated with prophylactic flow diversion surgery,and the extent of intrahepatic and extrahepatic bile duct resection is often controversial[1,2].A rare case of a young man who developed cholangiocarcinoma 6 years after flow diversion surgery for PBM with CBD is described.
CASE PRESENTATION
A 30-year-old Japanese man was found to have liver dysfunction at a medical examination.He had no remarkable medical history,was not on any medications,and had no allergies to any food or drug.He visited a nearby hospital and was diagnosed as having PBM with CBD.His common bile duct showed cystic dilatation accompanied by intrahepatic bile duct dilatation,which was classified as Todani type IVA(Figure 1).In the same year,he underwent cholecystectomy and a flow diversion operation that consisted of excision of the extrahepatic bile duct,and biliary and Roux-en-Y reconstruction.According to the Union for International Cancer Control(UICC)7thedition,the histopathological specimen showed adenocarcinoma foci,pT1,pNx,pStage IA.He did not have any adjuvant chemotherapy and five and a half years passed without any recurrence of biliary tract cancer.
MULTIDISCIPLINARY EXPERT CONSULTATION
However,six years after his operation,follow-up computed tomography(CT)showed a gradually growing nodule,about 10 mm in diameter,at the bile duct-jejunum anastomosis(Figure 2).Physical examination showed no abnormalities except for his previous operative scar.Laboratory tests were unremarkable,including liver and biliary enzyme profiles.Tumor markers were normal(carcinoembryonic antigen 0.8 ng/mL and carbohydrate 19-9 6.4 U/mL).Fluorodeoxyglucose positron emission tomography(FDG-PET)showed high FDG uptake,and magnetic resonance imaging showed restricted diffusion signals at the same nodular lesion.Double balloon enteroscopy showed the lesion directly.There were four holes anastomoses at the cholangiojejunostomy.A reddish and hemorrhagic tumor protruded from the posterior hole,and the other three holes were intact;the biopsy specimen showed adenocarcinoma(Figure 3).
以本次“长生疫苗事件”所暴露的产品质量不合格、商业贿赂等问题为代表,侵犯儿童健康权的事件屡禁不止。他山之石可以攻玉,基于社会矛盾的相似性,我们可以借鉴他国立法例,来寻求我国进一步完善相关立法的宏观方针与具体措施。

Figure 1 3D-reconstruction of magnetic resonance cholangiopancreatography shows an abnormally dilated common bile duct(white star).Both right and left hepatic ducts also show intrahepatic dilatations(white arrows).
FINAL DIAGNSIS AND TREATMENT
One month after percutaneous transhepatic portal embolization to prevent postoperative liver failure due to small remnant liver volume less than 30%,he underwent right lobectomy,biliary reconstruction,and regional lymph node dissection.At laparotomy,there were severe adhesions due to his previous operation.Right lobectomy was performed with dissection of the right hepatic artery,right portal vein,right hepatic vein,hilar bile ducts,and Roux-en-Y jejunum with cholangiojejunostomy.The remaining bile ducts in the hilar plate were three holes of B1,B2 plus B3,and B4.The biliary reconstruction was performed by new cholangiojejunostomy with a one-hole anastomosis.The Roux-en-Y reconstruction was also performed by a new jejunojejunostomy.The histopathological diagnosis was intraductal papillary neoplasm of the bile duct with high-grade intraepithelial neoplasia.There were no other abnormal findings in other intrahepatic bile ducts,including the anterior and posterior branches,with a negative bile duct margin.The dissected lymph nodes showed no evidence of malignancy.According to the UICC 8thedition,the pTNM classification was pTis,pN0,pStage 0(Figure 4).
OUTCOME AND FOLLOW-UP
The patient’s postoperative course was uneventful,and he was discharged on the 24th postoperative day.There has been no evidence of re-recurrence up to the present time.
DISCUSSION
PBM is a congenital anomaly defined as junction of the pancreatic and bile ducts outside the duodenal wall.Because of the abnormally located junction,the sphincter of Oddi does not work effectively.Reciprocal reflux of pancreatic juice and bile occurs,which introduces carcinogenic chemicals such as activated phospholipase A2 and secondary bile acids.These chemicals usually flow into the biliary tract because the hydropressure in the pancreatic duct is greater than that in the bile duct.The anomaly can also cause chronic cholangitis and chronic bacterbilia.As a result,patients with PBM have a higher risk of biliary tract cancer[3].
PBM can be divided into two categories:PBM with congenital biliary dilatation(CBD),which was previously called congenital choledochal cyst;or PBM without biliary dilatation(BD)[4].Todaniet al[5,6]classified this disease into five categories,and the Todani classification is now commonly used worldwide.
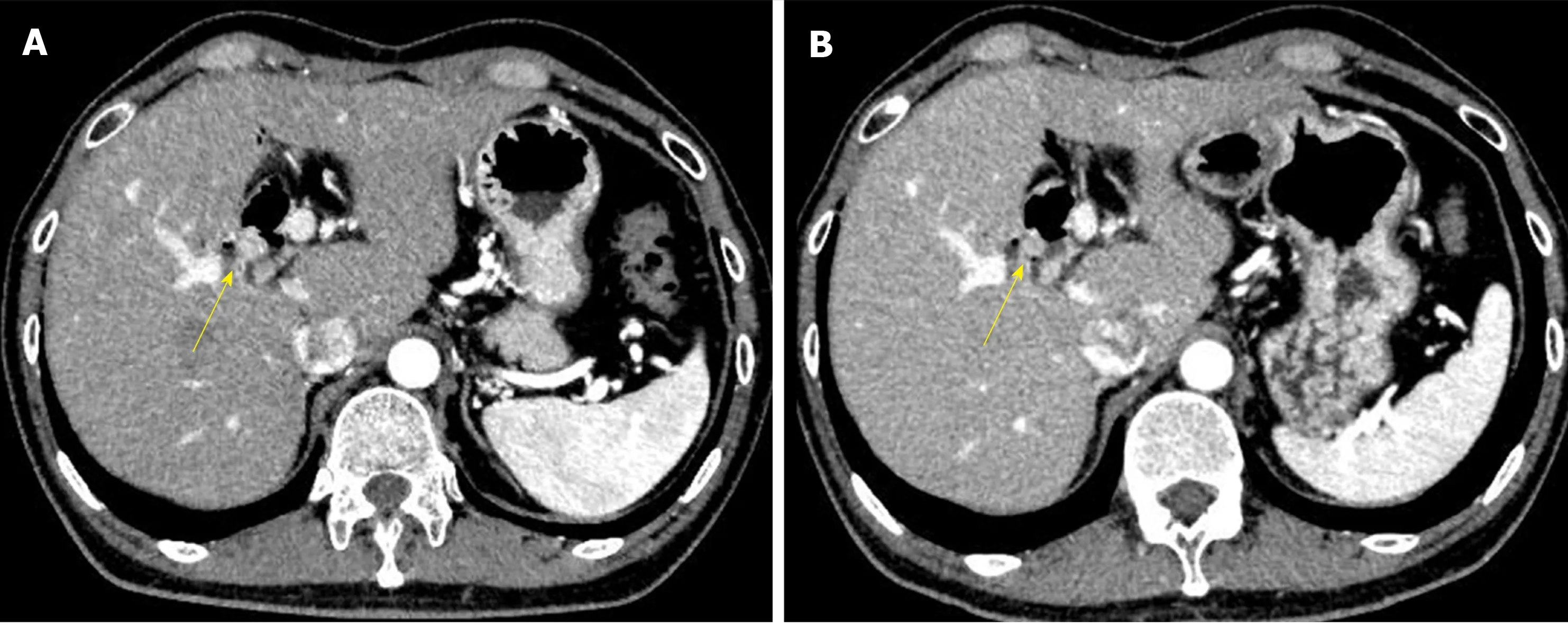
Figure 2 Abdominal CT images with contrast.A:Five and a half years after his first operation;B:Six years after his first operation.The images show a gradually growing nodule with contrast over a half a year(yellow arrow).
The essential management of PBM is prophylactic surgery to avoid carcinogenesis,and it should be performed immediately after the diagnosis of PBM[1].Since bile stasis in the dilated biliary tract is the most important factor for the development of malignant changes in biliary epithelial cells[7],the treatment for PBM with CBD is prophylactic flow diversion surgery,and that for PBM without BD is prophylactic cholecystectomy.However,there is no consensus of opinion on whether intrahepatic dilated bile ducts should be resected for PBM with CBD,or whether extrahepatic nondilated bile ducts should be resected for PBM without BD[1,8].
The present case showed a rare clinical course of PBM with CBD.Watanabeet al[9]reported that the incidence of cancer after extrahepatic bile duct excision is less than 1%.There seem to be two reasons for the carcinogenesis in this case.The first reason is that the flow diversion surgery left the dilated right hepatic duct in the hilar plate.In the first operation,the dilated left hepatic duct was removed,but the dilated right hepatic duct was used for cholangiojejunostomy.Since 30 years had passed before his diagnosis of CBD,there must have been some histological changes in the biliary epithelial cells,such as hyperplasia,metaplasia,and dysplasia.Damage and repair of the dilated biliary mucosa were likely to occur even after the first operation,resulting in carcinogenesis at the site of the cholangiojejunostomy.The second reason is that the reflux of intestinal juice at the cholangiojejunostomy probably played an important role in carcinogenesis.The stasis of bile and intestinal juice in the dilated biliary tract induces bacterial overgrowth and generation of unconjugated secondary bile acids[10].The carcinogenic toxicity of secondary bile acids still remains unclear,but some authors report the following mechanism in mice and its relationship to humans.Secondary bile acids suppress the expression of chemokine ligand 16(CXCL16),which recruits natural killer T cells,by liver sinusoidal endothelial cells.Then,the suppressed expression of CXCL16 weakens immunological defenses and leads to the development of malignancy and progression[11,12].
There have been 41 reported cases of biliary tract cancer after flow diversion surgery for PBM with CBD in the English literature from 1967 to 2016[7,13-41].The characteristics of these patients are shown below(Table 1).Of the 41 cases reported,35 reported details of the interval between age at flow diversion surgery and age at detection of biliary tract cancer.These 35 cases were divided into three groups by age(A,child group,0-15;B,adolescent/young adult group,16-30;and C,adult group,>30 years old),and the interval times are shown in the figure(Figure 5).There were significant differences between Group A and Group B(median 26.5vs4.0 years,P<0.0001),and between Group A and Group C(median 26.5vs8.5 years,P<0.0001),with no difference between Group B and Group C.These data mean that patients who undergo flow diversion surgery in adulthood can develop biliary tract cancer earlier than patients who undergo it in childhood.In adulthood,furthermore,interval time does not always depend on age at flow diversion surgery,and it is short,most often less than 10 years.This fact suggests that the damage to the remaining biliary epithelial cells due to carcinogenic chemicals is greater in adulthood than in childhood.In adulthood,the interval time may depend on the size of the dilated bile duct,on the extent of reflux,on the flow diversion procedures,or on lifestyle.The details remain unknown,and further similar cases need to be studied.
In the future,the current patient has a high probability of re-recurrence of cholangiocarcinoma.Although Tsuchidaet al[42]reported that chemoprevention can be effective for PBM to prevent postoperative carcinogenesis,this is still controversial.

Figure 3 Double balloon enteroscopy shows the cholangiojejunostomy directly.A:There are four-hole anastomoses:Anterior hole,posterior hole,B2 plus B3 hole,and B4 hole,from right to left.A reddish and hemorrhagic tumor protrudes from the posterior hole;B:The tumor extends inside the posterior branch.
CONCLUSION
Follow-up throughout the life of a patient after flow diversion surgery is recommended[4],but this is difficult in some cases.This case suggests the necessity of careful observation after flow diversion surgery,especially when PBM with CBD is detected in adulthood,and when cancer has already developed in the bile duct.
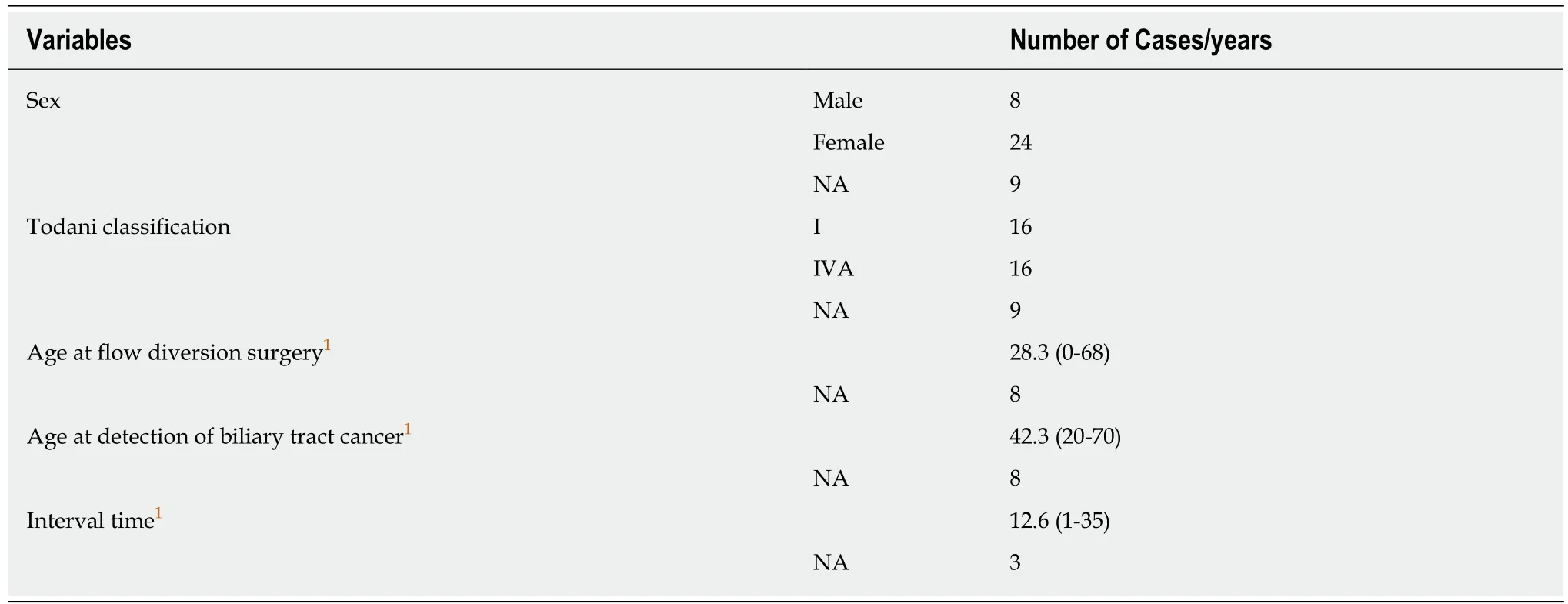
Table 1 Characteristics of the patients with biliary tract cancer after flow diversion surgery

Figure 4 Histological analysis of the tumor.A:Macroscopic findings;B:Hematoxylin and eosin(HE)staining,× 20;C:HE staining,×400.Histological studies show papillary growth and fibrovascular cores in the macroscopically nodular area(yellow arrow),comprising high-grade atypical epithelial cells.There is no invasive carcinoma associated with the intraductal neoplasm.

Figure 5 The graph shows the relationship between age at diversion surgery and interval time.Data represent means and standard deviation.P<0.0001,oneway analysis of variance and Bonferroni’s multiple comparison test.