Use of three-dimensional printing in preoperative planning in orthopaedic trauma surgery: A systematic review and meta-analysis
Catrin Morgan, Chetan Khatri, Sammy A Hanna, Hutan Ashrafian, Khaled M Sarraf
Catrin Morgan, Chetan Khatri, Khaled M Sarraf, Trauma and Orthopaedics, Imperial College NHS Trust, London W2 1NY, United Kingdom
Sammy A Hanna, The Royal London Hospital, Barts Health NHS Trust, London E1 1BB,United Kingdom
Hutan Ashrafian, Department of Surgery and Cancer, Imperial College London, London W2 1NY, United Kingdom
Abstract
Key words: Orthopaedic surgery; Trauma; Three-dimensional printing
INTRODUCTION
With the increasing complexity of operations and surgical decision-making, threedimensional (3D) printing is a novel modality with the potential to make a huge impact in the surgical field. In 1984, the first patent for a 3D printer was filled in the United States by Charles Hall titled, “Apparatus for production of 3D objects by stereolithography”, which was, in effect, the world’s first 3D printer (Patent number:US4575330A). It has been used in a variety of different surgical specialties including plastic surgery, neurosurgery, cardiothoracic surgery, oral and maxillofacial surgery[1,2]. The first reported use in orthopaedics was in 1999 as an aid to preoperative planning in complex spinal surgery[3].
3D printing also known as “rapid prototyping” or “additive manufacturing”creates a 3D model through different techniques. As opposed to traditional manufacturing techniques that are a “subtractive” process (removing excess material),3D printing is an “additive” process. This involves creating 3D objects by adding material layer-by-layer. Firstly, a high-resolution computed tomography (CT) scan of the deformity, fracture or defect is required. Computer-aided design (CAD) software then creates a digitalised representation of an object, which is then converted most commonly into a stereolithograpy (STL) file[4]. STL files “cut up” the digitalised model created by the CAD software, allowing the 3D printer to print the object layer by layer[5].
In orthopaedics, the use of 3D printing can be broadly split into three categories.This includes: (1) The use of 3D printing in pre-operative planning; (2) 3D implants;and (3) 3D patient-specific instrumentation (PSI). In pre-operative planning, 3D printed models of the fracture configuration or pathology can allow surgeons to visualise relevant anatomy and help aid executing complex operations, for example in pelvic trauma surgery[6]. 3D printed implants can be used for direct replacement of a large defect after tumour resection and to aid reconstruction in limb-salvage surgery[7]. PSIs have a wide application across orthopaedics and are largely used for more accurate implant placement, especially in the presence of abnormal anatomy and deformities, as well as developing templates for deformity correction and tumour resection[8].
Despite 3D printing being described as the third industrial revolution, the necessary evidence to justify the expanding investment in 3D printing in surgery remains ambiguous. Whilst the concept of 3D printing is favoured, particularly in those countries with advanced economies, its widespread application to daily clinical practice is relatively unknown. As we approach the end of the second decade following the first use of 3D printing in orthopaedics, an overview of this innovation may allow us better understanding of its potential application in every day practice in orthopaedic trauma.
Studies comparing the use of 3D printing with conventional approaches have suggested an improvement in orthopaedic operative outcomes, as measured by blood loss, use of fluoroscopy and operative time[9-11]. However, the systematic assessment and meta-analysis of 3D printing in orthopaedic trauma as a single entity has not been performed. The aim of this comprehensive systematic review and meta-analysis was to draw evidence from all studies across all areas of orthopaedic trauma, irrespective of age and gender, to assess the overall role of 3D printing in orthopaedic preoperative planning and core surgical outcomes. The primary outcome measures in this review were (1) Operation time; (2) Intra-operative blood loss; and (3)Fluoroscopy used.
MATERIALS AND METHODS
This study was performed in accordance to PRISMA guidelines for the reporting of systematic reviews[12]. The study protocol was pre-defined and registered on PROSPERO and can be accessed at http://www.crd.york.ac.uk/PROSPERO/display_record.php?ID=CRD42018078429.
Inclusion criteria
This paper included: (1) Full text papers in English language; (2) Humans of any age undergoing orthopaedic trauma procedures; (3) Randomised controlled trials (RCTs),case-control studies, cohort studies and case series of greater than 4 patients in orthopaedic trauma; and (4) Studies reporting the use of 3D printing in preoperative planning in orthopaedic trauma surgery.
Exclusion criteria
Studies were excluded if they were (1) Case reports or case series with less than five patients; (2) Abstract only publication; (3) Involved 3D imaging but not 3D printing during the operative procedure; (4) Involved 3D printing but not preoperative planning; (5) Duplicate data set; (6) Studies assessing the use of 3D printing in manufacturing custom implants and PSI; and (7) Non-trauma (elective) orthopaedic surgery.
Search strategy and study selection
We performed a search of Medline, Ovid and Embase from inception to February, 8 2018 and imported citations into EndNote X7 (New York, United States) reference manager software. Duplicate citations were removed and the remaining citations were screened using title and abstract to match the eligibility criteria. Two authors(Morgan C and Khatri C) independently assessed each paper with discrepancies being resolved with discussion with senior authors (Ashrafian H, Hanna SA, Sarraf K).Additional papers that were appropriateviaa manual search were added. The full search strategy can be found in the supplementary materials.
Outcome measures
The primary outcome measures in this review were (1) Operation time; (2) Intraoperative blood loss; and (3) Fluoroscopy used.
Data extraction
Data was extracted and entered to Microsoft Excel (Microsoft Cop. Redmond, WA,United States) by two authors (Morgan C and Khatri C). Demographic data was extracted from each paper including year of publication, country of publication and type of 3D printing technology used. Specifically for the participants, the number of participants, age and gender ratio was determined.
Quality assessment
Two authors (Morgan C and Khatri C) independently assessed the quality of included papers. For randomised controlled trials, the Jadad score was used[13]. This is a wellvalidated score that assesses the methodological quality of clinical trials by assessing the randomisation process and blinding the study has used. The Jadad score uses five questions, with a point scale of zero to five. We classified a score of ≥ 3 as “higher quality” and < 3 as “lower quality”. For all other study types, the Newcastle-Ottawa scale was used[14]. This score assesses studies based on three categories: (1) The selection of the study groups; (2) The comparability of the study groups; and (3) The ascertainment of the outcome measure in cohort studies. We classified studies with ≥7 stars as “higher quality” and < 7 stars as “lower quality”.
Statistical analysis
Meta-analysis was performed through the inverse-variance, random-effects model of DerSimonian and Laird for both continuous and categorical outcomes. Continuous outcomes were analysed by calculating the ratio of means for each study, with expression of uncertainty of each result represented by the 95% confidence intervals(CI). We substituted median for mean in studies where only the median was reported[15]. We performed meta-analysis if two or more separate studies were available. This was accomplished using Stata 15 (StataCorp., College Station, TX,United States). The I2 statistic was used to estimate the degree of heterogeneity between studies, where larger values indicate increasing heterogeneity.
RESULTS
Seventeen studies were found that fulfilled the inclusion criteria, producing a data set of 922 patients (Figure 1). Six of these studies were RCTs, two cohort studies (1 prospective, 1 retrospective) and nine case series (8 prospective, 1 retrospective). The area of orthopaedics and type of pathology varied and are shown in Table 1. The overall mean follow up was 18.16 mo. Data from studies with comparison groups that specifically looked at the primary outcomes were included in the meta-analysis.
Operation time
Operation time was measured in eight of these studies; six were RCTs[6,9-11,16-19]. Metaanalysis of these studies confirmed a significant reduction in operation time of 19.85%in the 3D printing group [95%CI: (-22.99, -16.71)] in comparison to the conventional group (see Figure 2). The heterogeneity was high (I2= 100.0%).
意外的患病,更让他工作中不等不靠,努力跑在时间的前面,重拳打击违法违规行为,让不法分子付出付不起的代价。2015年,郑全意和队员们借助全市强力打击食品非法添加的东风,查处了一个血豆腐添加甲醛的串案,并把涉案者移交公检法机关,在全市首次实现了“行刑合一”惩处食品生产加工领域的不法分子。
Intra-operative blood loss
Intra-operative blood loss was investigated in seven studies; six were RCTs[6,9-11,16-18].Meta-analysis revealed a significant reduction in blood loss of 25.73% (see Figure 3)with the use of 3D printing [95%CI: (-31.07, -20.40)]. The heterogeneity was high (I2=100.0%).
Fluoroscopy used
The number of times fluoroscopy was used was measured in four RCTs[6,9-11]. The use of 3D printing led to a significant reduction of 23.80% (see Figure 4) in the number of times fluoroscopy was used [95%CI: (-38.49, -9.10)]. The heterogeneity was high (I2=100.0%).
DISCUSSION
Our analysis demonstrates that the use of 3D printing in preoperative planning in orthopaedic trauma, can lead to a reduction in operation time, intra-operative blood loss and fluoroscopy used. Our systematic review represents the largest and most comprehensive in this area and is the first meta-analysis to date. Although research in the field consists of small-sized studies, findings confirm the current evidence in these studies of the positive effect of 3D printing in preoperative planning.
Operation time
A shortened operation time of 19.85% with the use of 3D printing confers significant benefits to the patient and costs associated. Increased operative time has been found to be associated with an increased risk of developing post-operative complications,such as wound infections and deep vein thrombosis[29,30]. The reasons behind this are multifactorial and include: (1) the surgeon having a stronger appreciation of pathological anatomy through geometric characterisation by the 3D printed model; as such it allows the surgeon to physically review complex cases. For example, in pelvic surgery it allows the surgeon greater understanding of acetabular fractures and reduces the degree of inter-observer variability in the classification of these injuries[28];(2) It facilitates pre-operative instrumentation decisions; and (3) Facilitates the planning of the surgical approach[10]; for example in trimalleolar fractures, the surgeon is able to determine the size of the internal fixation plate, clarify the placement position of the plate and screws and prebend the plate according to the morphology of the bone[16]; and (4) The 3D model also enables simulation of the surgeryin vitroallowing the surgeon better understanding of fracture reduction, hence leading to a reduction in the operation time (in comparison to the control groups)[11]. Together,these elements of 3D printing that lead to a decreased operative time can translate into cost savings, specifically through decreased staff and operating room overheads.There is evidence to suggest that a decrease in operative time confers cost savings with a 45-min reduction in operation time leading to a saving of almost $2700 per case for a paediatric population[31].
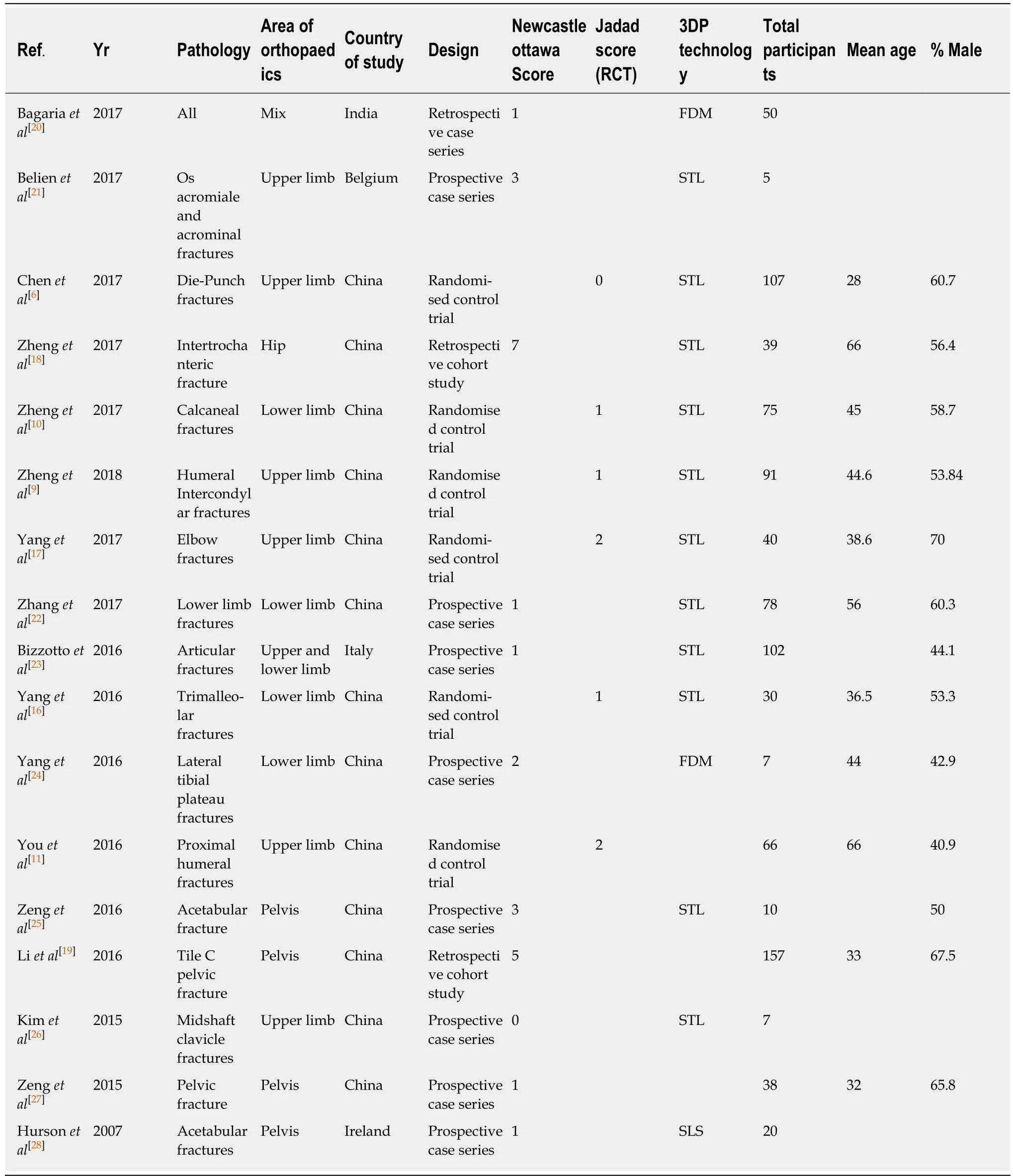
Table 1 Results summary
Intra-operative blood loss
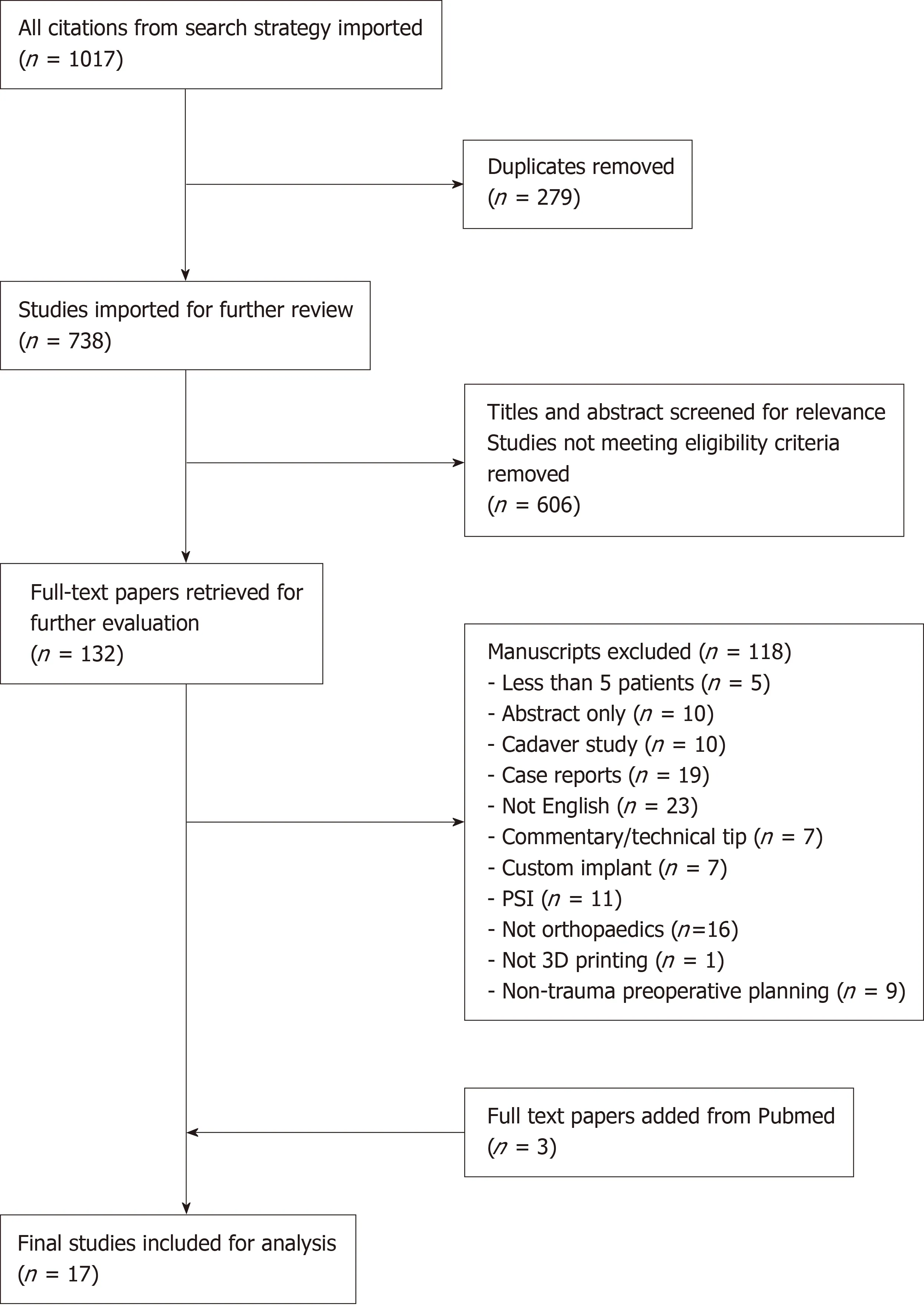
Figure 1 Search strategy.
Reducing blood loss and the need for blood transfusion in orthopaedic surgery remains a concern among surgeons and physicians in the perioperative period[32].Many different methods have been developed including; controlled hypotensive anaesthesia, cell salvage techniques[33], and pharmacological interventions (tranexamic acid)[34]. Our results show a significant reduction in intra-operative blood loss (25.73%)with the use of 3D printing which carries powerful implications for pre- and perioperative planning and practice especially in the context of trauma. A parallel can be drawn with a reduction in blood loss found with the use of robotic surgery[15]. Reasons studies attributed to the reduction of intra-operative blood loss are similar to those for reduction in operation time (better understanding of pathology and ability to plan the operation). The use of 3D printing in pelvic ring fractures demonstrated a reduced volume of fluid infused intra-operatively, with patients less likely to require a surgical drain or blood transfusion post-operatively[19]. Similar findings were reported with the use of 3D models in elbow fractures, it allowed the plate to be chosen and contoured accurately to ensure optimal compactness with the bone surface[17]. This minimised dissection of the surrounding tissue and protected the blood supply surrounding the fracture fragments, hence reducing intraoperative blood loss.
Fluoroscopy used
A small number of studies looked at the number of times intraoperative fluoroscopy was used and overall they reported a reduction in fluoroscopy of 23.80% with the use of 3D printing. This included calcaneal fractures, distal radius fractures and humeral fractures[6,9-11]. A reduction in fluoroscopy carries safety benefits through minimising patient radiation exposure. Radiation exposure remains a significant occupational hazard to the orthopaedic surgeon, radiographers and theatre staff throughout their careers[35]and also to patients subjected to this radiation. Although there is limited literature available on the appropriate amount of intraoperative fluoroscopy use in orthopaedics, a recent paper has reported reference values for common trauma operations[36]. Patient exposure to intraoperative radiation is an important factor to consider especially in the paediatric trauma setting as children are up to ten times more sensitive to radiation damage than adults[37].

Figure 2 Forest plot of operation time with the use of three-dimensional printing.
Cost and production
An obstacle that exists for the transition of 3D printed models from small studies to large scale clinical practice is cost and production. Creating a 3D printed model, is a complex process requiring advanced computer software and a 3D printer. This process does not come without cost and the need for an experienced team that are familiar with the software. Clinically, not all fractures may require a CT scan, a plain radiograph may suffice, therefore the use of 3D printing may be most useful for complex fractures, for example in pelvic trauma. The cost of printing the model seemed to vary greatly from $2-3 per model to $330[17,38]. There is also the cost of the printer to consider with studies reporting the cost to be $1000-2200[9,31]. In the studies reviewed, the time taken to produce the model ranged from 5 h to 72 h, which is a potential limitation to the use of 3D printing in an acute trauma setting[6,18].Nevertheless, an important factor to consider is that 3D printing in orthopaedics is a novel field. Therefore, as 3D printing technology progresses both the cost and production time is likely to reduce. Today, the most basic 3D printer for home use can be purchased for less than $200 compared to when 3D printers were first used in the 1980s costing around $300000 (at that time, corresponding to over $750000 in the current era)[39].
Patient understanding and surgical training
A number of studies in this review conducted patient and surgeon questionnaires on 3D printing[6,9,10,17]. It was found that the 3D models improved patient understanding of the fracture and communication with the doctor, leading to higher compliance with post-operative rehabilitation. Patients felt that conventional medical images such as plain radiograph or CT are too complicated to understand, however 3D models allow better visualisation of the fracture[17]. This technology therefore represents a powerful modality to enhance patient empowerment.
The reduction in the total hours worked by surgical trainees has led to an increase in the use of simulation-based training in orthopaedics[40,41], this has been used in fields such as arthroplasty, arthroscopy and trauma surgery[42,43]. With the increase in operative management for complex deformities, using 3D models enables these deformities to be recreated allowing the trainees to learn how to manage these challenging cases through simulation and apply this knowledge to the operating theatre. The advantages of 3D printing therefore have the potential to decrease surgical learning-curves and possibly improve surgical outcomes.
Strengths and limitations
This is the first comprehensive systematic review and meta-analysis conducted on the use of 3D printing in preoperative planning across all types of orthopaedic trauma surgery on core surgical outcomes. It included 17 studies in which six were randomised control trials. However, the results presented here should be considered in the context of a number of limitations. Where meta-analysis was possible, the heterogeneity was high. However, this was not unexpected given the wide area of orthopaedics (where different specialties are highly distinct), type of pathology and patient demographics. It was not possible to carry out a subgroup analysis due to the limited number of studies in the different subspecialties of orthopaedic trauma. A high level of heterogeneity in the absence of any other clear evidence highlights that this scientific field is still in its infancy where its methodology and practices are highly variable, nevertheless the results of this integrated data does indicate the results of clinical effect in the absence of more robust evidence (which is clearly necessary in future studies).
Our focus on operation time, blood loss and number of times fluoroscopy was used was based primarily on the fact that these were the most commonly reported outcomes in the literature. However, these parameters may not fully demonstrate the true value of 3D printing in orthopaedics, parameters such as post-operative function or complications were not determined.
Case series were included to address the paucity of RCTs inevitably introducing other biases associated with this study design and contributing to the heterogeneity.Of note twenty-three of these studies were carried out in China comprising of 81%(745) of the total number of patients. Apart from the randomised control trials, overall the quality scoring of the studies were low, with all 11 studies scoring six or less in the Newcastle-Ottawa Scale. All six of the randomised control trials were of low quality as determined by the Jadad scale. Reasons for low scores include lack of surgeon blinding, which is unlikely to be possible in clinical trials of 3D printing. In many trials, however, the risk of bias relating to sequence generation, adequate follow up,study dropout rate and assessment of outcome was unclear as sufficient information was not available due to poor reporting. The risk of publication bias should also be considered. The number of participants in these studies were small, with the largest being 157, therefore the possibility of “small study effect” cannot be ignored.
CONCLUSION
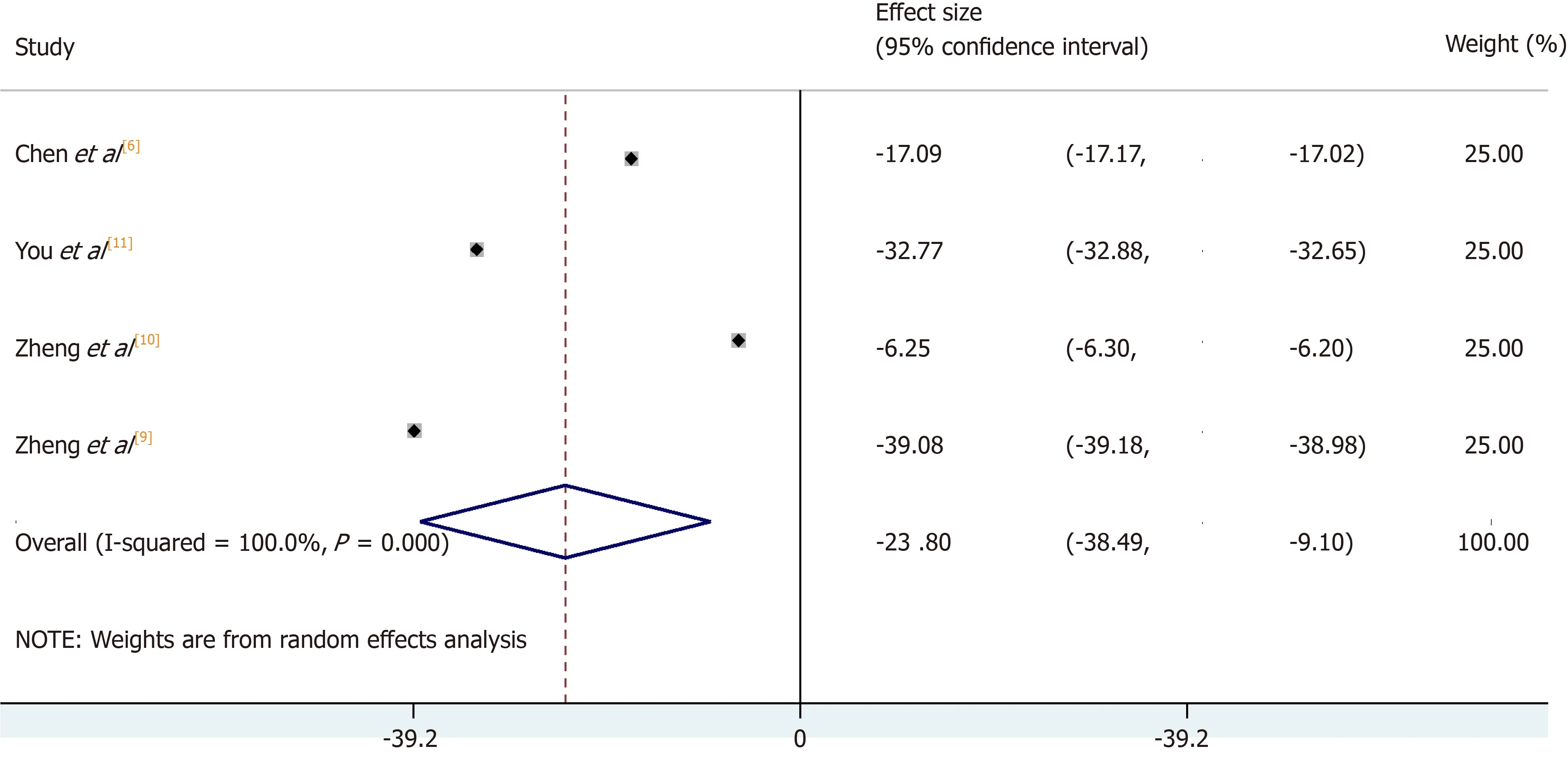
Figure 4 Forest plot of fluoroscopy used with the use of three-dimensional printing.
In summary, our meta-analysis and systematic review on the use of 3D printing in preoperative planning in orthopaedic trauma suggests that 3D printing reduces operative time, intraoperative blood loss and the number of times fluoroscopy is used.3D printing is a rapidly evolving field and it allows surgeons to gain better understanding of complex trauma cases and aid in surgical planning. The increased application of this technology has the potential to revolutionise orthopaedic practice and enhance clinical outcomes. There is however the need for an in-depth costanalysis for the use of 3D printing in surgery, taking into account the production costvspotential savings made by improved intra-operative outcomes. Further studies, in particular more randomised control trials in similar areas of orthopaedics are required to further enhance our knowledge of the role of 3D printing in orthopaedics and its application to daily clinical practice.
ARTICLE HIGHLIGHTS
Research background
With the increasing complexity of operations and surgical decision-making, three-dimensional(3D) printing is a novel modality with the potential to make a huge impact in the surgical field.In orthopaedics, the use of 3D printing can be broadly split into three categories. This includes:(1) The use of 3D printing in pre-operative planning; (2) 3D implants; and (3) 3D patient-specific instrumentation. In pre-operative planning, 3D printed models of the fracture configuration or pathology can allow surgeons to visualise relevant anatomy and help aid executing complex operations. It is however not clear how best to utilise the technique and whether this results in better outcomes.
Research motivation
The focus of this study is the use of 3D printing in preoperative planning in orthopaedic trauma surgery. Studies comparing the use of 3D printing with conventional approaches have suggested an improvement in orthopaedic operative outcomes, as measured by blood loss, use of fluoroscopy and operative time. However, the systematic assessment and meta-analysis of 3D printing in orthopaedic trauma as a single entity has not been performed. The increased application of this technology has the potential to revolutionize orthopaedic practice and enhance clinical outcomes.
Research objectives
The aim of this research was to draw evidence from all studies across all areas of orthopaedic trauma, irrespective of age and gender, to assess the overall role of 3D printing in orthopaedic preoperative planning and core surgical outcomes. The primary outcome measures in this review were (1) Operation time; (2) Intra-operative blood loss; and (3) Fluoroscopy used.
Research methods
This study was performed in accordance to PRISMA guidelines for the reporting of systematic reviews. The study protocol was pre-defined and registered on PROSPERO. A search of Medline, Ovid and Embase from inception to February 8, 2018 was carried out and citations were imported into EndNote X7 (New York, United States) reference manager software. Two authors independently assessed the quality of included papers. FFor randomised controlled trials, the Jadad score was used and for all other study types, the Newcastle-Ottawa scale was used. Meta-analysis was performed through the inverse-variance, random-effects model of DerSimonian and Laird for both continuous and categorical outcomes.
Research results
Seventeen studies (922 patients) met our inclusion criteria and were reviewed. The use of 3D printing across all specialties in orthopaedic trauma surgery demonstrated an overall reduction in operation time of 19.85% [95% confidence interval (CI): -22.99, -16.71], intra-operative blood loss of 25.73% (95%CI: -31.07, -20.40) and number of times fluoroscopy was used by 23.80%(95%CI: -38.49, -9.10). Overall, the quality of the studies was low and it was not possible to carry out a subgroup analysis due to the limited number of studies in the different subspecialties of orthopaedic trauma.
Research conclusions
This meta-analysis and systematic review on the use of 3D printing in preoperative planning in orthopaedic trauma suggests that 3D printing reduces operative time, intraoperative blood loss and the number of times fluoroscopy is used. 3D printing is a rapidly evolving field and it allows surgeons to gain better understanding of complex trauma cases and aid in surgical planning. 3D printing should be considered as an adjunct to improve patient care by minimising operative insult in orthopaedic trauma surgery.
Research perspectives
The study highlights the potential impact 3D printing can have in orthopaedic trauma surgery.Further studies, in particular more randomised control trials in similar areas of orthopaedics are required to further enhance our knowledge of the role of 3D printing in orthopaedics and its application to daily clinical practice. There is also the need for an in-depth cost-analysis for the use of 3D printing in surgery, taking into account the production costvspotential savings made by improved intra-operative outcomes.
 World Journal of Orthopedics2020年1期
World Journal of Orthopedics2020年1期
- World Journal of Orthopedics的其它文章
- Double-row repair of rotator cuff tears: Comparing tendon contact area between techniques
- National trends in total hip arthroplasty for traumatic hip fractures:An analysis of a nationwide all-payer database
- Corrections in alpha angle following two different operative approaches for CAM-type femoral acetabular impingement - Ganz surgical hip dislocation vs anterior mini-open
- Good accuracy of the alpha-defensin lateral flow test for hip periprosthetic joint infection: A pilot study in a retrospective cohort of 52 patients
- Effect of deep transverse friction massage vs stretching on football players’ performance
- Rapid spontaneous resolution of lumbar ganglion cysts: A case report
