Choice and management of negative pressure drainage in anterior cervical surgery
Qi-Hang Su, Kai Zhu, Yong-Chao Li, Tao Chen, Yan Zhang, Jun Tan, Song Guo
Qi-Hang Su, Kai Zhu, Yong-Chao Li, Yan Zhang, Jun Tan, Song Guo, Department of Orthopedics,Shanghai East Hospital, Tongji University School of Medicine, Shanghai 200120, China
Tao Chen, Department of Orthopedics, Shanghai Tongji Hospital, Tongji University School of Medicine, Shanghai 200092, China
Abstract
Key words: Spine; Anterior cervical surgery; Negative pressure; Drainage;Gastrointestinal decompression apparatus; Silica gel negative pressure drainage ball
INTRODUCTION
Anterior exposure of the cervical spine has been performed safely and effectively for decades[1]. First described in 1958[2,3], this approach to the intervertebral discs allowed for treatment of both central and neuroforaminal diseases in the cervical spine. The anterior cervical approach is one of the most commonly used cervical surgical approaches. While routine, this approach to the spine is not without risk. Indications of surgical procedures for certain conditions are still controversial and severe complications to cause neurological dysfunction or deaths may occur[4,5]. Common complications such as dural tear and cerebrospinal fluid leakage[6], esophageal injury[7], vascular injury and stroke[8], airway obstruction[9], Hoarseness and vocal code paralysis[10], dysphagia[11], C5 palsy[12], and adjacent segment disease[13]have been reported. Dyspnea is often caused by compression of the hematoma, edema of the larynx, and compression of the bone graft prolapse. Fanget al[14]retrospectively analyzed 3163 cases of anterior cervical surgery and found dyspnea caused by trachea compression of cervical hematoma in 16 (0.51%) of those cases. Sagiet al[15]retrospectively analyzed 311 patients who had undergone anterior cervical surgery and found that 6.1% of those had respiratory tract complications crisis, 1.9% needed tracheal intubation, while one (0.13%) case died.
Therefore, postoperative unobstructed drainage is an important measure for avoiding hematoma formation and preventing complications from anterior cervical surgery[16]. Common drainage methods include skin graft drainage, semi-drainage,and negative pressure drainage. Negative pressure drainage is able to swiftly and sufficiently drain blood from the body, thus avoiding the formation of hematoma[17].This means that negative pressure drainage is more commonly used in cervical surgeries.
Therefore, it is crucial to choose the safest and most reliable negative pressure drainage method correctly. In clinical settings, the most common negative pressure drainage device in anterior cervical surgery is the silica gel negative pressure drainage ball. While routine, the incidence of airway complication is still very high[9]. Therefore,in recent years, our team has attempted to use the gastrointestinal decompression apparatus to carry out negative pressure drainage in anterior cervical surgery. In this study, the drainage performance of two kinds of commonly used methods, the silica gel negative pressure drainage balls (from two different manufactures) and gastrointestinal decompression apparatus, were tested. Meanwhile, clinical data from patients using different drainage devices were collected to undertake a retrospective analysis. We hypothesized that the gastrointestinal decompression apparatus would be better for patients undergoing anterior cervical surgery in terms of enhancing drainage and reducing postoperative complications as well as improving prognosis.
MATERIALS AND METHODS
Subjects
Data from patients who had undergone anterior cervical surgery using the silica gel negative pressure drainage balls between January 2007 and January 2012, and those who had undergone anterior cervical surgery using the gastrointestinal decompression apparatus between January 2012 and January 2018 in our department were retrospectively collected and analyzed, which were searched in the Picture Archiving and Communication System database. The inclusion criteria were as follows: (1) Patients aged between 20 and 90 years old; and (2) Patients who had undergone routine anterior cervical surgery by Dr. Tan due to cervical spondylosis and had negative pressure drainage with either the silica gel drainage ball or the gastrointestinal decompression apparatus. The exclusion criteria were: (1) Patients who had died of critical diseases which were not related to the surgery after their operation and so did have lost to follow-up; (2) Patients who had received cervical vertebra surgery previously; and (3) Patients who had severe underlying diseases of non-cervical spondylosis during their hospital stay, which would have influenced the researchers’ correct assessment of surgical prognosis.
Materials
Two types of silica gel negative pressure drainage balls (200 mL; bought from Guangzhao Medicine Supplies Factory and Shanghai Chengyi Industry, respectively)were utilized. We also utilized one type of gastrointestinal decompression apparatus(1000 mL; bought from Shanghai Caoyang Medicine Supplies Factory), the body of which is made of polyethylene conforming to the requirements of YY0114-2008. The spring is stainless steel, while the connecting tube is a rubber blood transfusion tube which conforms to GB4491-2003.
Test method
The silica gel negative pressure drainage balls and gastrointestinal decompression apparatus were emptied fully and injected with 0 mL, 25 mL, 50 mL, 75 mL, 100 mL,125 mL, 150 mL, 175 mL, 200mL, 225 mL, 250 mL, 275 mL, and 300 mL of water or air.Following this, the negative pressures of the three drainage devices were respectively measured (Figure 1).
Statistical analysis
The effects of five types of cervical vertebra diseases (cervical spondylosis, ossification of the posterior longitudinal ligament, cervical disc herniation, cervical hyperextension injury and traumatic disc herniation, and cervical tumor) and two kinds of negative pressure drainage (the silica gel negative pressure drainage ball and gastrointestinal decompression apparatus) on early complications were statistically described and analyzed using logistic regression model. Patient characteristics were summarized using frequencies for the categorical variables as well as with arithmetic means for the continuous variables. Risk factors for early complications were determined using logistic regression analysis (V20.0, SPSS).
RESULTS
This study included data from 1328 patients with an average age of 63 years. Patient demographics are summarized in Table 1. Figure 2 shows the age distribution.
The logistic regression model found no significant difference in the incidences of surgical complications among the gender and age groups (P> 0.05). However, the influence of different negative pressure drainage devices on surgical complications was found to be statistically significant [P< 0.05, odds ratio (OR) = 0.324, 95%confidence interval: 0.186-0.563]. The incidence of surgical complications using the silica gel negative pressure drainage ball was 3.086 (1/OR) times higher than that which occurred when using the gastrointestinal decompression apparatus.Meanwhile, the OR of different cervical diseases was very high, which may be due to the huge difference of distribution of diseases (Table 2).

Figure 1 The silica gel negative pressure drainage ball and the gastrointestinal decompression apparatus. A: The silica gel negative pressure drainage ball; B:The gastrointestinal decompression apparatus.
The test results of different devices are showed in Figure 3. Following the injection of water or air into the three negative pressure drainage devices, negative pressure generally decreased as the injection volume increased. The negative pressure of the three negative pressure devices changed dramatically when 0-75 mL of water or air was injected, whilst when the next 75-125 mL of water or air was injected, the negative pressure changes of the three negative pressure devices were smaller. When silica ball one was injected with 150 mL of water or air, the negative pressure increased temporarily and then decreased rapidly to zero. The negative pressure change of silica ball two was similar to that of silica ball one. However, as the injected water or air increased, the negative pressure of the gastrointestinal decompression apparatus could still decrease steadily and maintain a certain value when 300 mL of water or air was injected. These results also suggested that the influence of air and liquid on the negative pressure of the drainage device is approximately equivalent.
DISCUSSION
The importance of negative pressure in trauma treatment has been shown in many studies[18-25]. The negative pressure drainage device reduces its internal air pressure to be lower than the external atmospheric pressure mainly through elastic deformation of its own material in order to expand its original cavity volume. This pressure difference is the direct power of the negative pressure drainage and allows blood to be drained from the incision. However, as the drained volume increases, the pressure difference drops gradually and finally reaches zero, at which point the drainage device stops. This means that the longer this negative pressure continues, the more beneficial and safer it is for patients.
At present, the commonly used negative pressure development and blood collector systems include silica gel balls, gastrointestinal decompression apparatus, vacuum bottles, and negative pressure suction devices. And the simplest and most economical and common devices are still silica gel balls. However, the silica gel ball has a small drainage volume and a short drainage duration, and the negative pressure changes rapidly. Therefore, it is very necessary and important to find a negative pressure drainage system for the better drainage volume and duration. Although the gastrointestinal decompression apparatus is not initially designed for the anterior cervical surgery, we think it is better for patients undergoing anterior cervical surgery than that using the silica gel balls.
Our results demonstrated that the gastrointestinal decompression apparatus has a large drainage volume and a long drainage duration, and that the negative pressure decreases slowly along with the increase of drainage volume. In terms of the rapid change of the negative pressure of the silica ball, once this ball is even slightly affected by external factors (such as the ball’s leakage), it may easily cause poor drainage efficiency and complications. In contrast, the compensation ability of the gastrointestinal decompression apparatus, which has a smoother change of the negative pressure, is superior. Meanwhile, the results of this clinical analysis showed that the gastrointestinal decompression apparatus is superior to silica gel drainage balls in terms of enhancing drainage effect, reducing the incidence of postoperative complications, decreasing mean postoperative hospital stay, and improving patients’prognoses.
In fact, obstruction of the external tube on negative pressure drainage using either the silica gel drainage ball or the gastrointestinal decompression apparatus is very likely to happen. Although the gastrointestinal decompression apparatus is able toenhance drainage effect and reduce nurses’ workloads (For silica gel drainage ball,nurses need to frequently renew the negative pressure balls), postoperative care still must be strengthened to keep the external tube unobstructed all the time, and to avoid external tube drainage obstruction which can be caused by the patient turnover and other factors.
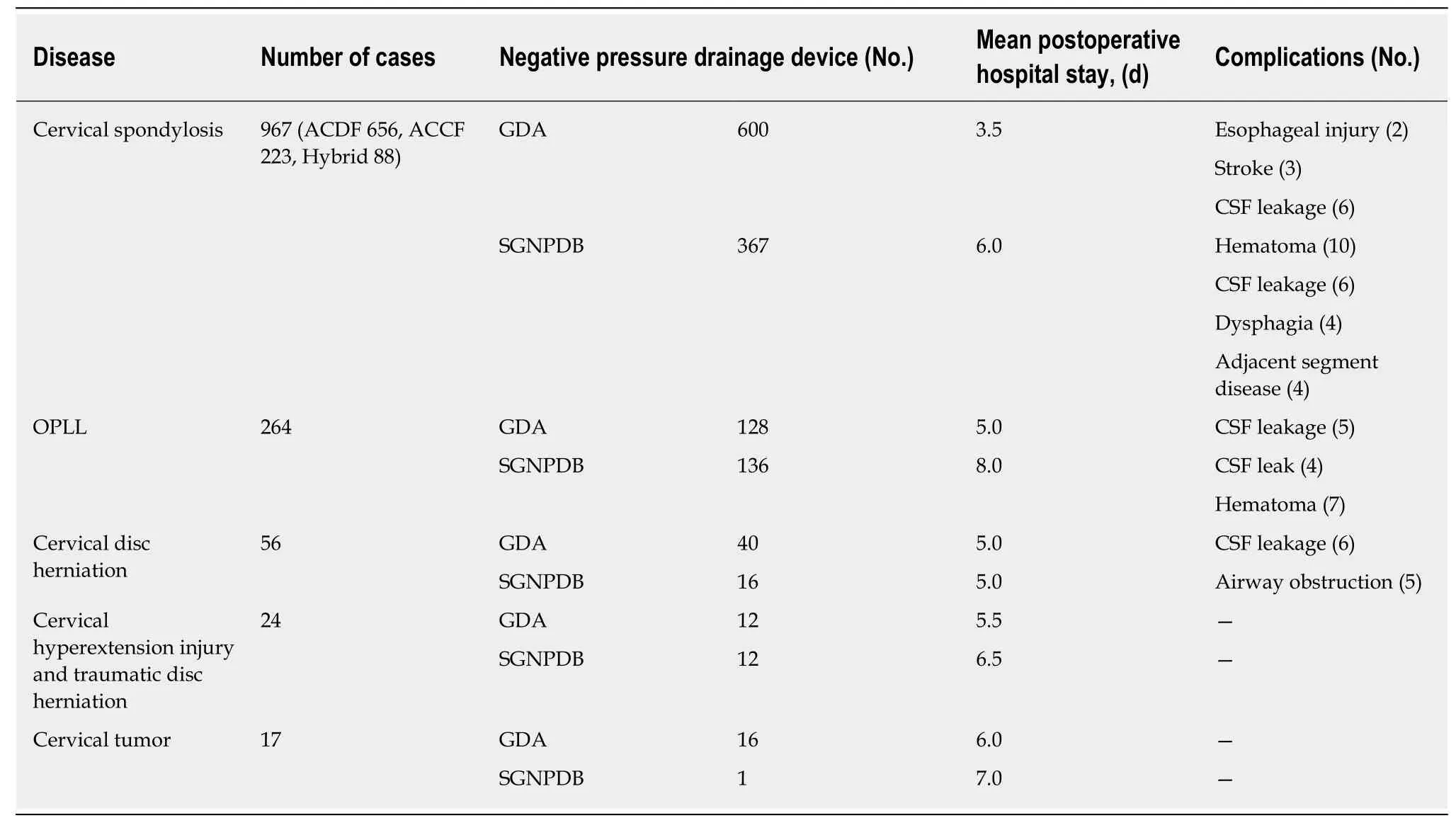
Table 1 Patient demographics (n = 1328)
Attention should be paid to two aspects in the postoperative examination of the negative pressure drainage tube. First, the patency of the drainage tube should be carefully checked. In clinical practice, the drainage tube is always connected with the negative pressure drainage ball. This means that the flowing of bloody fluid into the drainage tube from the incision as well as the blood reflux after pressing the drainage tube indicates that the negative pressure drainage tube is unobstructed. Second, it is necessary to check that there is continuous negative pressure in the drainage tube,since if negative pressure in the drainage tube disappears, an internal condensation hematoma can be formed. In such circumstances, even if the negative pressure suction is applied again, drainage will not be effective. Additionally, it should be noted that once the incision is closed, the internal components of that incision cannot be adjusted, meaning that it is crucial to properly position the working section and drainage area so as to maintain the persistence of negative pressure.
This study had some limitations. First, our study focused primarily on the comparison in two aspects of the drainage effect and clinical data between the two common drainage devices, without considering other new types of drainage devices.It thus remains to be clarified whether there are more economical, efficient, and safe drainage devices. Second, only two indexes of drainage volume and duration were discussed in the study. It is not known yet with respect to the issue that whether a greater negative pressure of drainage and longer duration may result in a better therapeutic result for each patient. Generally speaking, greater negative pressure and prolonged duration may contribute to reducing the incidence of hematoma and lightening the workload of nurses. However, it needs to be further studied concerning the need to pursue greater negative pressure blindly and the required duration of drainage for patients with cerebrospinal fluid leakage. Third, all patients who met pre-set inclusion criteria extracted from our department were enrolled simply in our study without strict and accurate classification. Consequently, the uneven distribution of disease types, surgical methods, drainage methods, age, and other factors would have a certain impact on the results of the experiment. Therefore, the results of statistical analysis in this study can only be used as a reference for research. More indepth research and analysis in combination with clinical practice are required to confirm whether gastrointestinal decompressor is superior to silica gel drainage balls or not. In addition, since this study was designed as a retrospective study, there would be some errors in the recording of clinical data. Simultaneously,gastrointestinal decompressor for drainage in cervical spine surgeryviaanterior approach is a unique innovative approach developed by our team. All the subjects of study were collected from our department. It remains to be explored whether gastrointestinal decompressor may exert a better drainage effect when applied by other surgeons or in other hospitals. In the future, our team will continue to conduct prospective and multi-center studies in accordance with the principle of ethics and without harming the interests of patients.
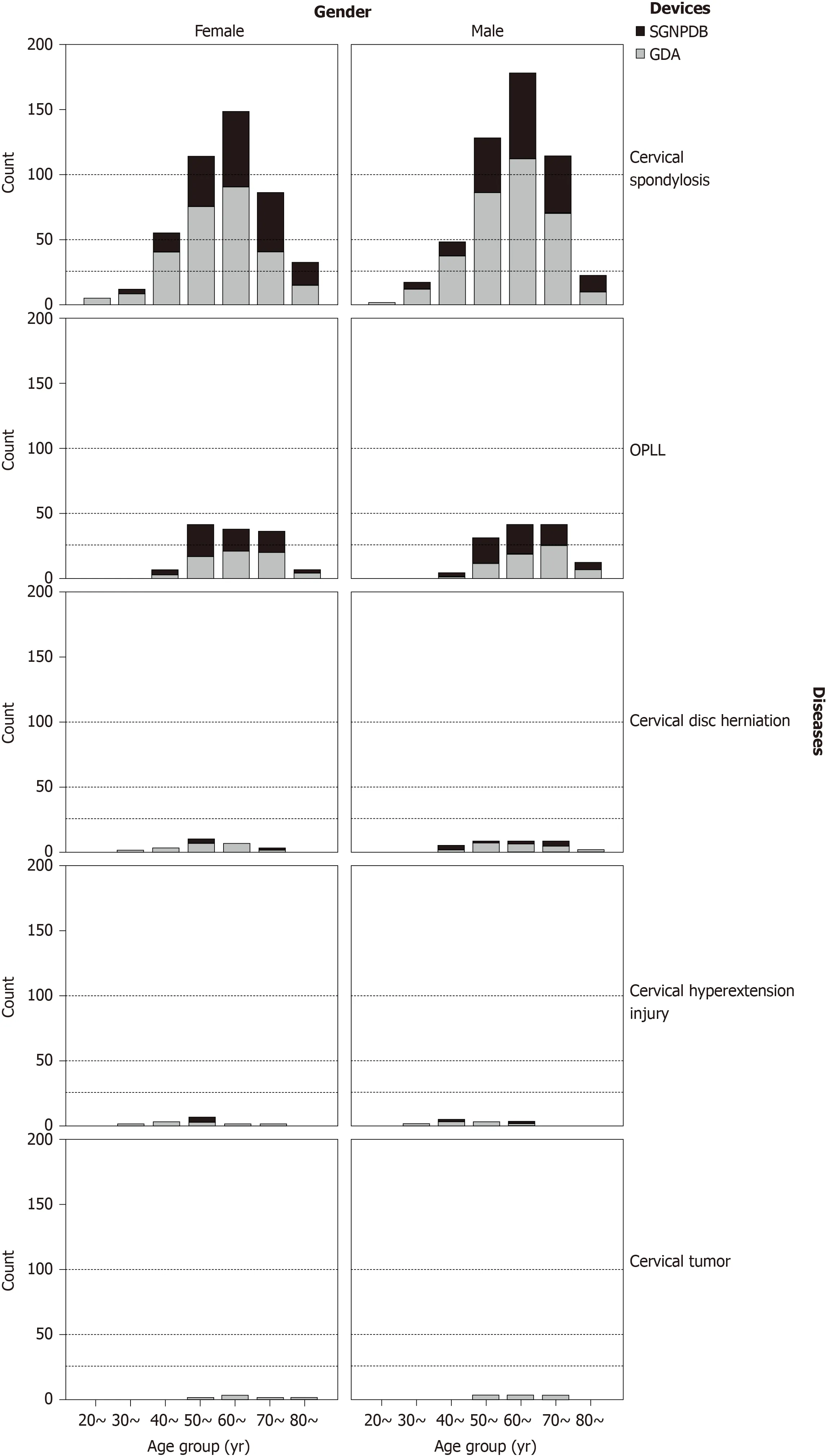
Figure 2 Distribution of age groups by gender, disease, and drainage device. OPLL: Ossification of posterior longitudinal ligament.
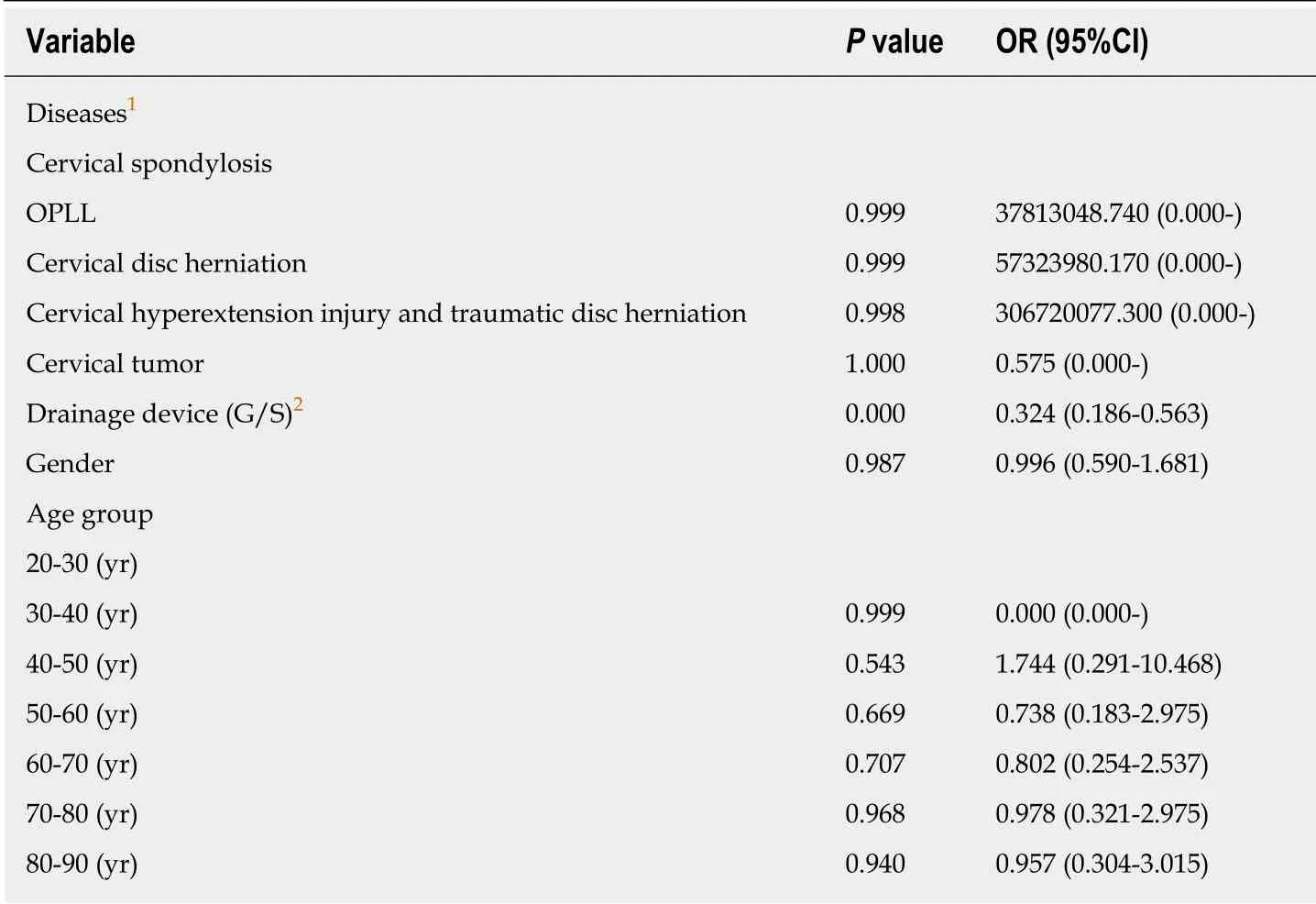
Table 2 Results of logistic regression analysis
In conclusion, while negative pressure drainage tubes are widely used in clinical settings and are familiar to surgeons, serious complications caused by their improper use are not uncommon. It is therefore necessary to emphasize the importance of the unobstructed drainage of drainage tubes in anterior cervical surgery. Unobstructed drainage under the correct level and placement is necessary, while reliable negative pressure drainage, such as the gastrointestinal decompression apparatus, should be used to ensure the persistence of negative pressure. Ineffective negative pressure drainage is worse than natural drainage.
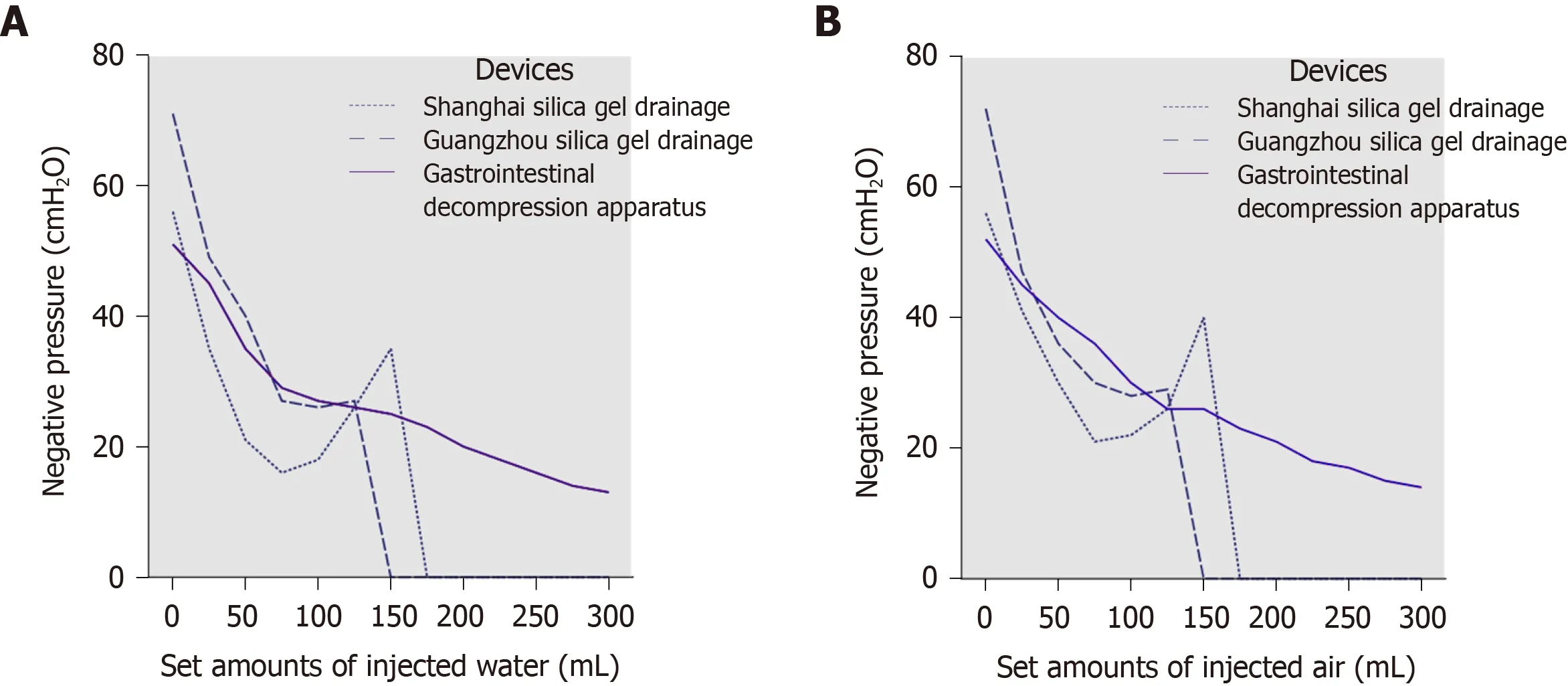
Figure 3 The test results of different devices. A: The negative pressures of the three drainage devices with the injection of water; B: The negative pressures of the three drainage devices with the injection of air.
ARTICLE HIGHLIGHTS
Research background
Postoperative unobstructed drainage is an important measure for avoiding hematoma formation and preventing complications from anterior cervical surgery. Therefore, it is crucial to choose the safest and most reliable negative pressure drainage method correctly.
Research motivation
In clinical settings, the most common negative pressure drainage device in anterior cervical surgery is the silica gel negative pressure drainage ball. While routine, the incidence of airway complication is still very high.
Research objectives
Our team has attempted to use the gastrointestinal decompression apparatus to carry out negative pressure drainage in anterior cervical surgery. In this study, the authors aimed to discuss the characteristics and key points of clinical management of two types of commonly used negative pressure drainage systems in clinical settings.
Research methods
Two types of commonly used silica gel negative pressure drainage balls and a type of gastrointestinal decompression apparatus were fully emptied and then injected with different amounts of water and air. Following this, the negative pressure values of the three devices were measured. Meanwhile, we undertook a retrospective analysis of the clinical data of 1328 patients who had been treated with different negative pressure drainage apparatuses during their anterior cervical surgery.
Research results
As the amount of injected air or water increased, the negative pressure of the silica gel negative pressure drainage ball decreased rapidly, dropping to zero when 150 mL of water or air was injected. In contrast, the negative pressure of gastrointestinal decompression apparatus decreased slowly, maintaining an ideal value even when 300 mL of water or air was injected.And statistical analysis demonstrated that patients who had been treated with the gastrointestinal decompression apparatus were less likely to develop severe complications than those who had been treated with the silica gel negative pressure drainage ball (P< 0.05).
Research conclusions
This study showed that the gastrointestinal decompression apparatus has the advantages of large suction capacity, long duration of continuous negative pressure, and good drainage effect,all of which are the favorable factors for the use of this apparatus for negative pressure drainage in anterior cervical surgery.
Research perspectives
Multi-center prospective controlled trials with multi-factor analyses and assessments, larger sample size, and prolonged follow-up period are needed for future investigations.
 World Journal of Clinical Cases2020年11期
World Journal of Clinical Cases2020年11期
- World Journal of Clinical Cases的其它文章
- Tumor circulome in the liquid biopsies for digestive tract cancer diagnosis and prognosis
- Isoflavones and inflammatory bowel disease
- Cytapheresis for pyoderma gangrenosum associated with inflammatory bowel disease: A review of current status
- Altered physiology of mesenchymal stem cells in the pathogenesis of adolescent idiopathic scoliosis
- Association between liver targeted antiviral therapy in colorectal cancer and survival benefits: An appraisal
- Peroral endoscopic myotomy for management of gastrointestinal motility disorder
