Risk scores, prevention, and treatment of maternal venous thromboembolism
Wei Zhang, Jian Shen, Jing-Li Sun
Wei Zhang, Jian Shen, Jing-Li Sun, Department of Obstetrics and Gynecology, General Hospital of Northern Theater Command (Heping Campus), Shenyang 110000, Liaoning Province,China
Abstract
Key words: Pregnancy; Puerperium; Venous thromboembolism; Risk factors; Prevention;Anticoagulation
INTRODUCTION
Venous thromboembolism (VTE) is an acute type of non-suppurative venous inflammation with secondary intravascular thrombosis. VTE includes pulmonary embolism (PE) and deep venous thrombosis (DVT), both of which have the same predisposing factors and are two clinical manifestations of VTE at different sites and different stages. The shedding of the DVT thrombus and its transfer to the lungs may cause PE and is strongly lethal. According to foreign reports, the risk of VTE in pregnant women is approximately 0.8‰-2‰, which is 3-7 times higher than that of non-pregnant women. The risk of VTE during puerperium is 2-4 times that during prenatal periods[1]. The incidence of DVT is three times that of PE, and PE accounts for 9% of maternal deaths[2]. To reduce the incidence of pregnancy-related VTE, Western countries have developed guidelines to evaluate maternal women according to risk factors, to identify high-risk groups, and to provide early preventive treatment.
At present, the preventive treatment for pregnancy-related VTE in China is in its infancy, and there is no uniform or standardized industry guide. Drug prevention and treatment of pregnancy-related VTE rely highly on foreign guidelines; however, due to the differences in ethnicity and national conditions, there are many controversies over the indications for drug treatment, drug selection, and dose selection for anticoagulant therapy[3]. Therefore, the standardized prevention and treatment of thrombosis in women during pregnancy represent an urgent issue faced by many Chinese doctors. In the present study, a total of 7759 patients who gave birth at our hospital from June 2018 to June 2019 were investigated in terms of the status of VTE prophylactic treatment, with an aim to provide reference for the clinical prevention and treatment of this condition.
MATERIALS AND METHODS
Study subjects
The clinical data from 7759 patients who gave birth at our hospital from June 2018 to June 2019 were studied. All patients were pregnant for 28 wk, and 3812 patients were followed until 42 d postpartum; the clinical data were complete.
Survey content
The survey included pr egnancy-related VTE risk factors, pregnancy-related VTE risk scores and grading, preventive drug anticoagulation, drug side effects, and thrombosis (follow-up was continued until 42 d postpartum).
Evaluation criteria
Risk factors:According to the "Clinical Management Recommendations for Thromboembolic Diseases during Pregnancy" [American College of Obstetricians and Gynecologists (ACOG), 2011][4]and "Guidelines for the Diagnosis and Treatment of Venous Thromboembolic Diseases during Pregnancy and Puerperium" [Royal College of Obstetricians and Gynaecologists (RCOG), 2015][5], the risk factors affecting pregnancy-related VTE were evaluated.
Pregnancy-related VTE risk scores and grading, drug prevention anticoagulation:The RCOG guidelines for scoring, grading standards, and drug anticoagulation programmes were adopted.
Drug side effects:Prenatal and postpartum haemorrhage, thrombocytopenia, and coagulopathy caused by drugs were recorded.
Incidence:VTE was diagnosed based on the symptoms and by venous colour Doppler ultrasound of the lower extremities 42 d after delivery.
Statistical analysis
Statistical analyses were performed using SPSS 11.5 statistical software.
RESULTS
Risk factors for pregnancy-related VTE
The RCOC guidelines divide risk factors affecting VTE into three broad categories:Pre-existing risk factors, obstetric risk factors, and new or transient risk factors.
According to the survey results, the most prevalent pre-existing factors were obesity and advanced age; the most common obstetric factors were caesarean section and preeclampsia; and the new or transient factors were mainly hyperemesis gravidarum and hospitalized miscarriage prevention. The detailed results are shown in Table 1.
Pregnancy-related VTE risk score, grading, and preventive drug anticoagulation
According to the RCOC guidelines and the VTE risk assessment form, for pregnant women without contraindications of anticoagulation, thrombosis prevention started during early pregnancy for those with a prenatal VTE risk score ≥ 4 points,thrombosis prevention started at 28 wk for those with a prenatal VTE risk score of 3 points, and thrombosis prevention lasted at least 10 d postpartum for those with a postpartum VTE risk score ≥ 2 points.
According to the results of the survey, 81 patients had a VTE risk score ≥ 4 at the time of admission, and 158 had a score of 3. Except for two patients with contraindications for thrombocytopenia, only 44 (approximately 18.81%) patients received prophylactic anticoagulant therapy during pregnancy (Tables 2-5). There were 3536 patients with a score ≥ 2 after delivery. During hospitalization, clinicians gave the patients low-molecular-weight heparin to prevent thrombosis. After discharge, only 824 (approximately 23.30%) patients continued to take medication for 10 d.
Drug side effects
There was no drug-related prenatal or postpartum haemorrhage. Thrombocytopenia and coagulopathy occurred in 44 patients who took prenatal medications and in 824 patients who took postpartum medications.
Incidence
No prenatal VTE occurred. Among the 4403 patients in the low-risk group with a postpartum score < 2 points, 2017 were followed until 42 d postpartum, and one case of lower extremity venous thrombosis was found (the patient had no symptoms).
Of the 3536 patients in the high-risk group with a postpartum score ≥ 2, 1795 were followed until 42 d postpartum. Among them, 824 patients received drug prophylaxis for 10 d, and no VTE was found. A total of 971 patients received drug prophylaxis only during hospitalization. They did not continue to take medication after discharge.Among them, one patient had PE secondary to lower extremity venous thrombosis,and one patient had intracranial venous sinus thrombosis.
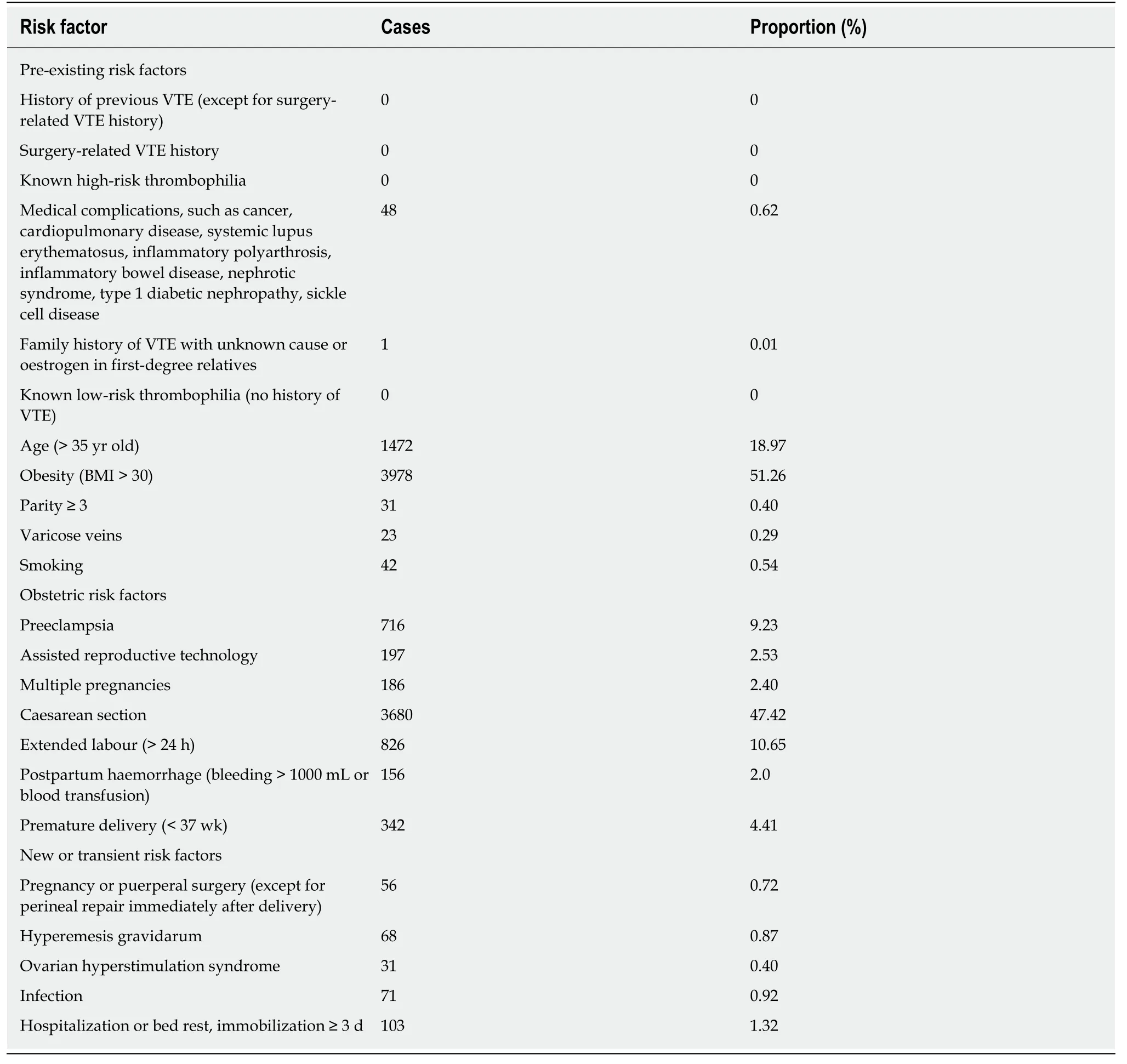
Table 1 Pregnancy-related venous thromboembolism risk factors
DISCUSSION
The classic Virchow theory states that the hypercoagulable state of blood, venous blood flow, and venous wall damage are the three major pathological causes of VTE[6].These three points are reflected in pregnancy. The blood is hypercoagulable during pregnancy. During late pregnancy, the enlarged uterus compresses the inferior vena cava, affecting venous return and causing blood flow to stagnate. During the delivery process, caesarean section and vaginal midwifery techniques cause venous vascular injury. Furthermore, different degrees of dehydration and activity reduction during the puerperium period also increase the risk of VTE. These are also the causes of maternal VTE.
The clinical symptoms of VTE during pregnancy lack specificity, and some patients with VTE may have no clinical symptoms. However, because it can be complicated by PE, VTE is strongly lethal. Treatment after a clear diagnosis is often unsatisfactory.Therefore, for VTE, prevention should be more important than treatment. At present,a number of studies have confirmed that prophylactic anticoagulant therapy can effectively reduce the incidence of VTE in high-risk populations[7-9]. Therefore,according to the risk factors for VTE in the early identification of high-risk groups,early drug prophylaxis is particularly important to reduce the incidence of VTE and maternal mortality.
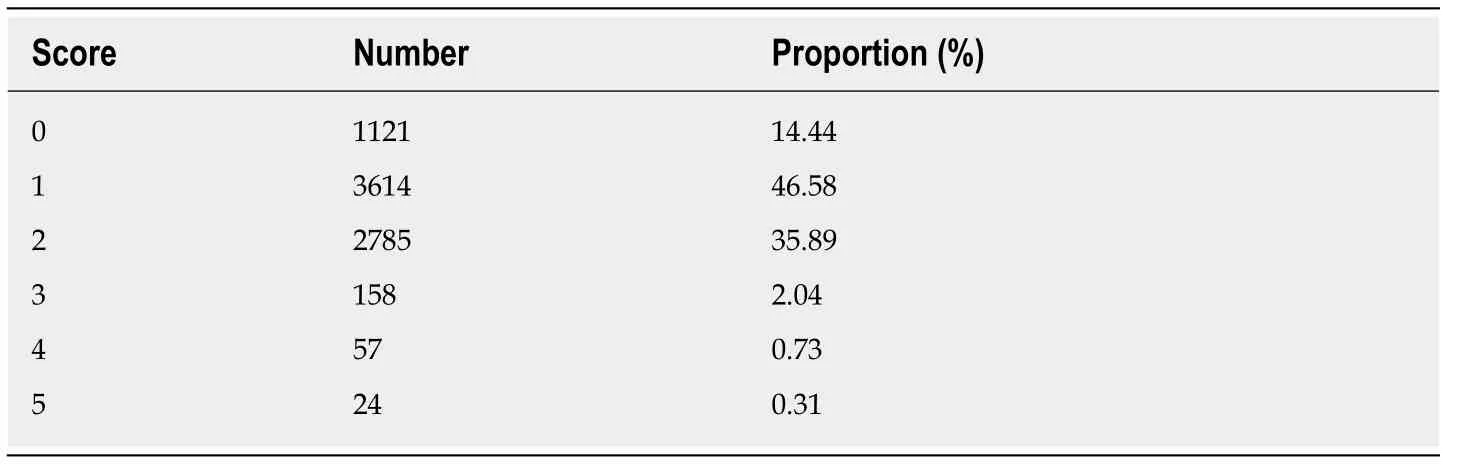
Table 2 Pregnancy-related venous thromboembolism risk scores upon admission
Risk factors for pregnancy-related VTE
The occurrence of pregnancy-related VTE is associated with many risk factors, which are mainly divided into pre-existing risk factors, obstetric risk factors, and new or transient risk factors. Pre-existing risk factors include age, obesity, and history of previous thrombosis. Obstetric risk factors include caesarean section, preeclampsia,and assisted reproduction. New or transient risk factors include surgery during pregnancy or puerperium, hyperemesis during pregnancy, and hospitalization or bed rest.
According to the survey results shown in Table 1, the characteristics of pregnancyrelated VTE risk factors in our hospital were as follows: (1) There was a high caesarean section rate. Although several measures have been taken in recent years to reduce the rate of caesarean section, the caesarean section rate remains high. Due to maternal wound pain and the effect of anaesthetic drugs after caesarean section,patients cannot get out of bed for a short time, or the amount of activity is small. The blood is hypercoagulable for a long time, and it is more prone to venous embolism and PE. The relative risk of VTE in women after caesarean section is 2 to 6.7 times that of vaginal delivery[10-12], which is an important risk factor for pregnancy-related VTE;(2) There were many patients with excessive body weight. With improvements in the maternal living standards in China and individual's incorrect living habits, nutrition is supplemented carelessly during pregnancy, and obesity is increased. Numerous studies have shown that obesity is a risk factor for pregnancy-related VTE[13,14]. A Danish study reported that obesity could increase the risk of VTE by a factor of five[15],and the risk increased with weight gain[7]; (3) There was an increase in maternal age.With the advancement of society, the transformation of the concept of fertility, and the implementation of the “two-child policy”, the number of elderly pregnant women in China has also increased. Studies have shown that the relative risk of VTE in pregnant women over 35 years old has increased approximately 2-fold. A large cohort study in the United States found that maternal women aged 35-44 were twice as likely to develop VTE as non-pregnant women aged 25-34. For older women, there was no significant difference in the risk of prenatal VTE, and the risk of postpartum VTE was 1.2 times that of pregnant women aged 25-34[16]; and (4) In addition, the increase in the number of complications during pregnancy, the extensive application of assisted reproductive technology[17], the increase in the number of selective twin pregnancies,the misunderstanding that threats of abortion and premature delivery require bed rest, and bad habits such as "confinement in childbirth" during the puerperium period increase the risk of VTE. The characteristics of pregnancy-related VTE risk factors in our hospital are also in line with Guet al[18]'s point of view.
It can be seen from the studies described above that in order to reduce the occurrence of pregnancy-related VTE, women should be instructed to have reasonable nutrition during pregnancy, to perform proper exercise, and to maintain a certain amount of exercise in order to avoid excessive weight gain during pregnancy.Reasonable medical treatment should be implemented, unnecessary treatments should be reduced in order to prevent miscarriage, and prolonged bed rest should be avoided. The benefits of vaginal delivery should be promoted, vaginal delivery should be encouraged, the number of caesarean sections without medical indications should be reduced, and the rate of caesarean section should be reduced. At the same time, publicity and education should be promoted, and getting out of bed early after childbirth should be encouraged during maternity.
Pregnancy-related VTE risk score, grading, and prophylactic anticoagulant therapy
Prophylactic anticoagulant therapy can reduce morbidity and mortality due to VTE in pregnant women. The ACOG and RCOG guidelines both emphasize the assessment of maternal VTE risks and preventive anticoagulant therapy based on the results. For the selection of anticoagulant drugs, the RCOG guidelines recommend low-molecular-weight heparin (LMWH). The advantages are as follows: (1) LMWH cannot pass through the placental barrier, is not secreted into milk, and does not affect foetal development and breastfeeding. LMWH is a class B drug for pregnancy in the US Food and Drug Administration classification, and maternal applications are relatively safe; (2) LMWH has high bioavailability (bioactivity of subcutaneous injections of 80%to 100%) and a long half-life (3-5 h); and (3) compared with unfractionated heparin,with LMWH, the incidence of bleeding during pregnancy, osteoporosis, and thrombocytopenia is low[19-23]. Therefore, the RCOG guidelines recommend LMWH as the drug of choice for prenatal and postpartum prevention of thrombosis.
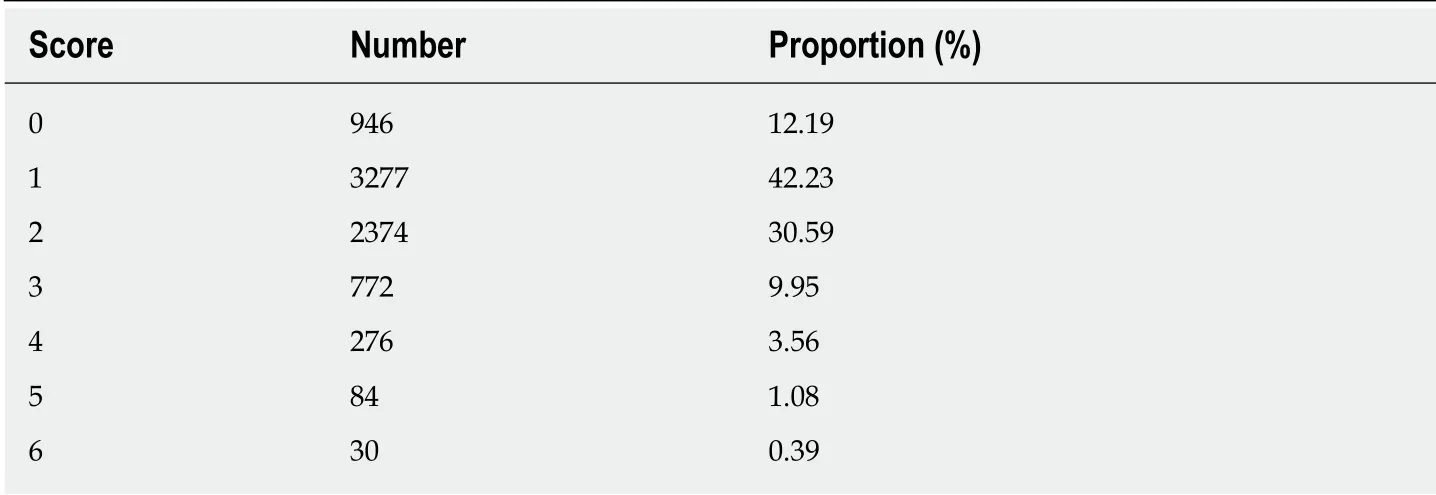
Table 3 Pregnancy-related venous thromboembolism risk scores after delivery
According to the survey, except for patients with drug contraindications, only 44 of the patients with a prenatal score ≥ 3 were treated with prophylactic anticoagulant therapy, and only 824 of the patients with a postpartum score ≥ 2 continued treatment after discharge until 10 d postpartum. The current situation of inadequate VTE prevention and treatment in our hospital is concerning. The reasons for this inadequacy mainly include: (1) Insufficient knowledge of the risk of pregnancyrelated VTE, with the belief that there is no need to use drugs; (2) Patients are examined in other hospitals and undergo no VTE risk assessments during pregnancy;(3) Clinicians worry that medication will increase the risk of bleeding and therefore do not recommend medication to patients; (4) Maternal women are worried about medication affecting foetal development and breastfeeding; (5) Maternal and family members do not apply anticoagulant drugs themselves; and (6) The high costs.
To improve the lack of preventive anticoagulant therapy for pregnancy-related VTE, the following recommendations are made: First, clinicians should emphasize the importance of pregnancy-related VTE, understand the necessity and importance of preventive anticoagulant therapy, and clarify that LMWH does not increase the risk of bleeding for patients who are not contraindicated. At the same time, the introduction of preventive treatment guidelines for pregnancy-related VTE is needed as soon as possible, and medical institutions at all levels should popularize VTE risk assessment,grading, and preventive treatment. Second, pregnant women should be educated to understand the dangers of VTE, the need for preventive anticoagulant therapy, and the safety of drugs in order to improve maternal compliance with drugs. Furthermore,personnel should teach pregnant women how to properly inject anticoagulation drugs.
Incidence
This survey shows the following: (1) VTE was not found in 7759 pregnant women before delivery, and three cases of VTE occurred in 3812 patients who were followed during the postpartum period; this again proved that the incidence of VTE in puerperium was higher than that prenatally[1], reminding obstetricians to pay more attention to the prevention of VTE during puerperium; (2) Studies have found that VTE during puerperium usually occurs 1-9 d after delivery[24]. The anticoagulant therapy for the cases of PE and intracranial venous sinus thrombosis in this investigation was less than 10 d, indicating that early termination of treatment may miss the best time for drug prevention. Thus, sufficient drug prevention and treatment are recommended for high-risk groups.
In summary, in China, pregnancy-related VTE is often neglected because of its relatively low incidence, but with improvements in maternal living standards and changes in fertility policies and fertility perspectives, the incidence of pregnancyrelated VTE is now increasing. Moreover, VTE may be complicated by PE, which is highly lethal and harmful, and requires the attention of the whole society.Prophylactic anticoagulant therapy is safe and effective for people at a high risk for VTE[25,26]. Therefore, for pregnancy-related VTE, prevention should be more important than treatment and pregnancy-related VTE risk assessment, and preventiveanticoagulation guidelines suitable for pregnant women in China should be issued as soon as possible. Maternal and child hospitals at all levels should conduct risk assessments of pregnant women during early pregnancy. For high-risk pregnant women, the knowledge on the dangers and prevention of VTE should be popularized,improper living habits should be corrected, various medical complications and pregnancy complications during pregnancy should be actively treated, and preventive anticoagulant therapy should be administered according to the risk assessment results to reduce the incidence of pregnancy-related VTE and ensure maternal life safety.
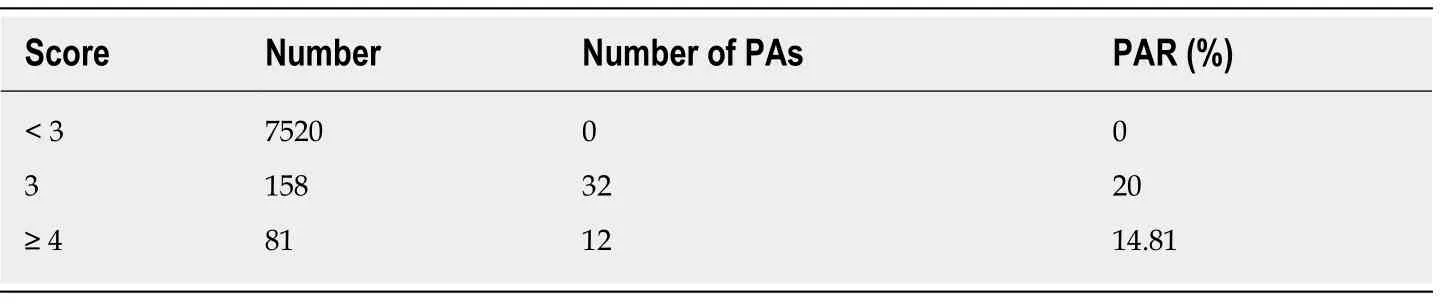
Table 4 Prophylactic anticoagulant application during pregnancy
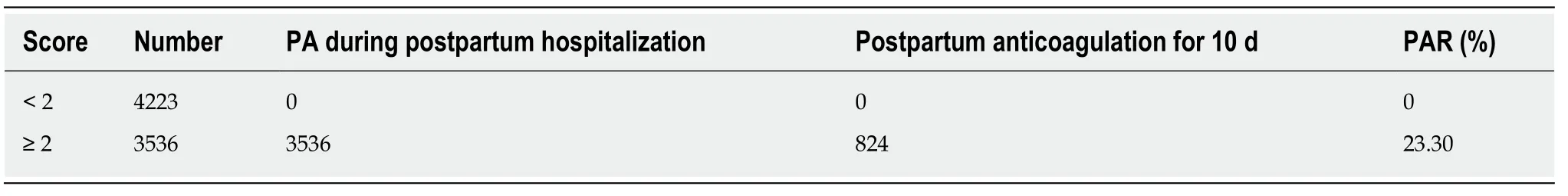
Table 5 Prophylactic anticoagulant application after childbirth
ARTICLE HIGHLIGHTS
Research background
The preventive treatment for pregnancy-related venous thromboembolism (VTE) in China is in its infancy. There is no uniform or standardized industry guide. Due to the differences in ethnicity and national conditions, there are many controversies over the indications for drug treatment, drug selection, and dose selection for anticoagulant therapy.
Research motivation
The standardized prevention and treatment of thrombosis in women during pregnancy represent an urgent issue.
Research objectives
In this study, the authors aimed to investigate the risk scores, prevention, and treatment of maternal VTE to promote the prevention and standardized treatment of maternal thrombosis.
Research methods
Totally 7759 patients who gave birth were retrospectively analysed. The risk factors for pregnancy-related VTE, prenatal and postpartum VTE risk scores, prophylactic anticoagulant therapy, side effects after medication, and morbidity were analysed.
Research results
The VTE risk factors were mainly caesarean delivery, obesity, and advanced maternal age.Among the patients who did not present with VTE before delivery, the authors found one case each of pulmonary embolism secondary to lower extremity venous thrombosis, intracranial venous sinus thrombosis, and asymptomatic lower extremity venous thrombosis during the postpartum follow-up.
Research conclusions
Among 7759 pregnant women, approximately 1/30 (prenatal) and 1/2 (postpartum) belonged to the high-risk group of pregnancy-related VTE, which is a subject of clinical intervention. Due to poor patient compliance, 18.41% (prenatal) and 23.30% (postpartum) of the high-risk patients received drug prophylaxis and treatment. VTE poses a serious threat to maternal safety, and the society should increase its vigilance against pregnancy-related VTE.
Research perspectives
Early detection of high-risk groups for VTE should be performed, and preventive anticoagulant therapy should be promptly implemented to reduce the incidence of pregnancy-related VTE and reduce maternal mortality.
 World Journal of Clinical Cases2020年11期
World Journal of Clinical Cases2020年11期
- World Journal of Clinical Cases的其它文章
- Tumor circulome in the liquid biopsies for digestive tract cancer diagnosis and prognosis
- Isoflavones and inflammatory bowel disease
- Cytapheresis for pyoderma gangrenosum associated with inflammatory bowel disease: A review of current status
- Altered physiology of mesenchymal stem cells in the pathogenesis of adolescent idiopathic scoliosis
- Association between liver targeted antiviral therapy in colorectal cancer and survival benefits: An appraisal
- Peroral endoscopic myotomy for management of gastrointestinal motility disorder
