Collision tumor of squamous cell carcinoma and neuroendocrine carcinoma in the head and neck:A case report
Shi-Hai Wu,Department of Radiation Oncology,the Second Clinical Medical College of Jinan University,Shenzhen People’s Hospital,Shenzhen 518020,Guangdong Province,China
Bao-Zhu Zhang,Department of Oncology,The People’s Hospital of Baoan,Shenzhen,The Affiliated Baoan Hospital of Southern Medical University,Shenzhen 518020,Guangdong Province,China
Ling Han,Department of Otorhinolaryngology,the Second Clinical Medical College of Jinan University,Shenzhen People’s Hospital,Shenzhen 518020,Guangdong Province,China
Abstract
Key words:Collision tumor;Squamous carcinoma;Neuroendocrine carcinoma;Chemoradiotherapy;Head and neck;Case report
INTRODUCTION
Collision tumor of squamous cell carcinoma (SCC) and neuroendocrine carcinoma(NEC) in the head and neck appears rare[1].This type of tumor in the nasal cavity and paranasal sinus is an even less likely occurrence[2].A multidisciplinary approach including surgery,chemotherapy,and radiotherapy should be carefully designed once the diagnosis is confirmed.The real challenge is how to treat two synchronous malignancies.Here,we present a case of SCC and NEC colliding in the nasal cavity and paranasal sinus to promote the understanding of collision carcinoma.
CASE PRESENTATION
Chief complaints
A 47-year-old female patient presented with frequent intermittent bleeding in the right nasal cavity for 6 mo.
History of present illness
The symptom of nosebleed was exacerbated with the passage of time.The patient had no fever,headache,chest tightness,or shortness of breath.
History of past illness
The patient used to be in good health.No history of major past illnesses was found.
Personal and family history
No relevant personal or family history was found.
Physical examination
No obvious abnormalities were found in physical examination.
Laboratory examinations
No obvious abnormalities were found in laboratory examinations.
Imaging examinations
A computed tomography (CT) scan revealed a 4.1 cm × 2.85 cm × 4.3 cm heterogenous mass of the right nasal and paranasal region,which invaded the nasal septum,right inferior middle turbinate,and right lateral wall of maxillary sinus bone,expanded to the right orbital base,and compressed the right internal rectus muscle and the right optic nerve (Figure1).The neck and abdominal ultrasound showed no metastasis signs.
FINAL DIAGNOSIS
Biopsy pathology of nasal mass specimen revealed poorly differentiated SCC with necrosis.Postoperative pathology of the specimen revealed poorly differentiated SCC with neuroendocrine carcinoma as a collision tumor (Figure2A).CK5/6 was diffusely positive in the squamous differentiation area and negative in neuroendocrine differentiation cells (Figure2B).P40 was also diffusely positive in the squamous differentiation area (Figure2C).CD56 was positive in neuroendocrine components(Figure2D and E).Chromogranin A and synaptophysin expression was negative(Figure2E and F).
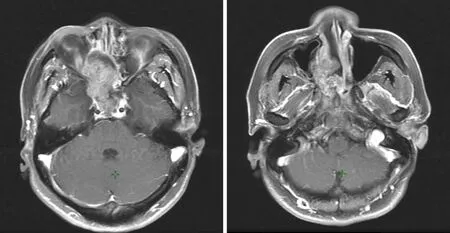
Figure1 Images before surgery showing a mass in the nasal cavity and paranasal region.
TREATMENT
She received operation in August 2018.A CT scan after the surgery revealed residual lesions in the primary tumor region (Figure3A and B).Then concurrent chemoradiotherapy was performed with radiotherapy 68.0Gy and chemotherapy of lobaplatin and VP-16 for four cycles.The chemotherapy regimen was lobaplatin (55 mg,day 1) and VP-16 (100mg/m2,day 1-3).Follow-up at 3 mo after completion of the full course of treatment showed that the patient experienced a complete response(Figure3A and B).
OUTCOME AND FOLLOW-UP
Positron emission tomography-CT taken in August 2019 (12 mo after diagnosis)revealed no signs of recurrence or metastasis (Figure3C).
DISCUSSION
Different terms,including collision/mixed/composite/combined tumor,have been employed to describe tumor consisting of two malignant components.The more troublesome is that the definition of collision tumor has been a matter of debate for years.In 2000,the World Health Organization (WHO) classifications of tumors of endocrine organs suggested that collision tumors are those in which either component occupies at least 30% of the tumor tissues[3,4].However,it might be an arbitrary criterion since the 30% cutoff has not been proven by reliable clinical data.The more malignant component in collision tumor,even if its share is less than 30%,tends to alter the biological behaviors.Furthermore,in the WHO classification of thyroid and lung tumors[5,6],mixed NEC and non-NEC tumors were not defined by a minimum percentage.We agree to the proposition of Yuet al[7]that collision carcinoma should meet the following conditions:Two malignant neoplasms of different pathological types derive simultaneously from the same location of human body and appear like a mass to the naked eye,with no evidence that one neoplasm migrates from the other.
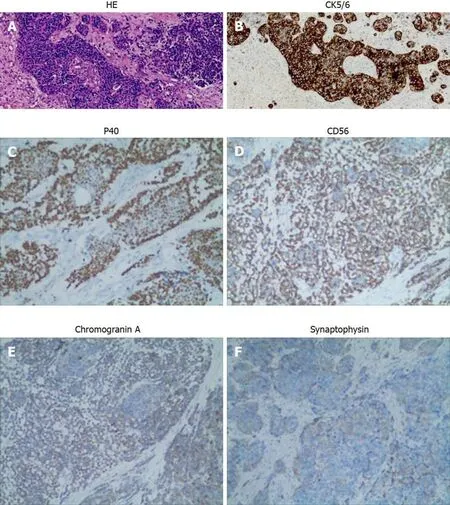
Figure2 Immunohistochemical images.A:Hematoxylin and eosin (HE) staining showed typical squamous and neuroendocrine differentiation areas of the neoplasm;B:CK5/6 was diffusely positive in the squamous differentiation area and negative in neuroendocrine differentiation cells;C:P40 was diffusely positive in the squamous differentiation area;D:CD56 was positive in neuroendocrine components;E:Chromogranin A expression was negative;F:Synaptophysin expression was negative.Original magnification,× 200.
According to our definition of collision tumor,we reviewed 26 well-documented cases of collision tumor of NEC and SCC in the head and neck from 1978 to 2019 (key words:Collision or mixed or composite or combined carcinoma,and the head and neck).Combining the data with our patient,the resulting group of 27 patients is large enough to allow some meaningful analysis.Of all cases,23 were male and 4 were female.The sex ratio of men to women is 5.75:1,which displays a significant difference.The mean age of the 25 patients was 58.37 years (range:32-83 years).Their clinical pathological features,treatments,and outcomes are summarized in Table1.As to tumor sites,20 (74.1%) originated from the larynx,4 (14.8%) from the nasal and paranasal cavity,1 from the palatine tonsil,and 1 from the soft palate.Fourteen(55.5%) patients were heavy smokers,which keeps consistent with the association between cigarette usage and head-neck cancer.Of all cases,7 received surgery (S)alone;7 received chemotherapy (C) and radiotherapy (R);6 received S + R + C;5 received S + R;1 received S + C;and 1 received no treatment for high performance status (grade 3).Follow-up information was available for 23 patients (Table1).Eight patients died of diseases (tumor) from 3.5 to 39 mo after diagnosis (mean survival,24.1 mo),and 8 were clinically disease-free,from 6 to 60 mo (mean survival:18.9 mo)following diagnosis.Seven patients were living with unresectable tumor,from 12 to 39 mo (mean survival,28.8 mo),after diagnosis.There were only 2 patients who developed local relapse,and coincidentally,both of them received C + R treatment but no surgery.Four patients had recurrent regional lymph nodes metastases,7 developed remote metastasis,including 3 affecting the bone,1 lung,1 lung and bone,1 bone and liver,and 1 right breast mass.
One difficulty existing in collision tumor is to establish accurate preoperative diagnosis.To obtain two malignant neoplasms by single biopsy is like to kill two birds with one stone.A definite diagnosis most depends on careful microscopic observation of surgical specimens,especially with the application of immunohistochemistry.Another problem is that the outcome of collision tumor of SCC and NEC appear very poor.As far as we know,there have been two reports of collision carcinoma involving NEC and SCC in the nasal and paranasal region.However,it is the first case who achieved a complete response.Ferlitoet al[8]raised the point that radical surgery takes little effect in improving local tumor control of collision tumor of the larynx.Besides,laryngectomy will result in voice loss and control only the primary lesion.Therefore,a combination of systematic chemotherapy and radiotherapy is recommended for small cell carcinoma.National Comprehensive Cancer Network Guidelines of Neuroendocrine Tumors (version 2015) suggest that patients with locoregional unresectable neuroendocrine tumors receive R + C;moreover,therapeutic manner of small cell carcinoma of the lung,which combined R with systemic chemotherapy,is worth learning.
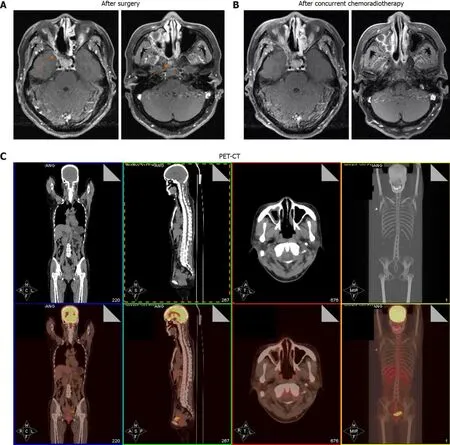
Figure3 The patient has a complete response after chemoradiotherapy.A:Images after surgery showing postoperative residual lesions (orange arrows);B:Images after surgery showing that a complete response was achieved;C:The latest positron emission tomography-computed tomography showing no signs of recurrence or metastasis.
Due to the rarity of collision carcinoma of NEC and SCC in the head and neck,the treatments should be carefully designed for two different malignancies.Our case indicated that high attention should be paid to the malignant degree of both components and individual characteristics,and certain patients may benefit from postoperative concurrent radiotherapy and chemotherapy.
CONCLUSION
In a word,we have described a case of collision carcinoma of SCC and NEC in the nasal cavity and paranasal sinus.The existed literature of collision tumor in the headand neck region has been analyzed to understand this disease.Treatments including surgery and chemoradiotherapy may lead to a good survival for patients.More cases of collision carcinoma need to be reported and summarized.
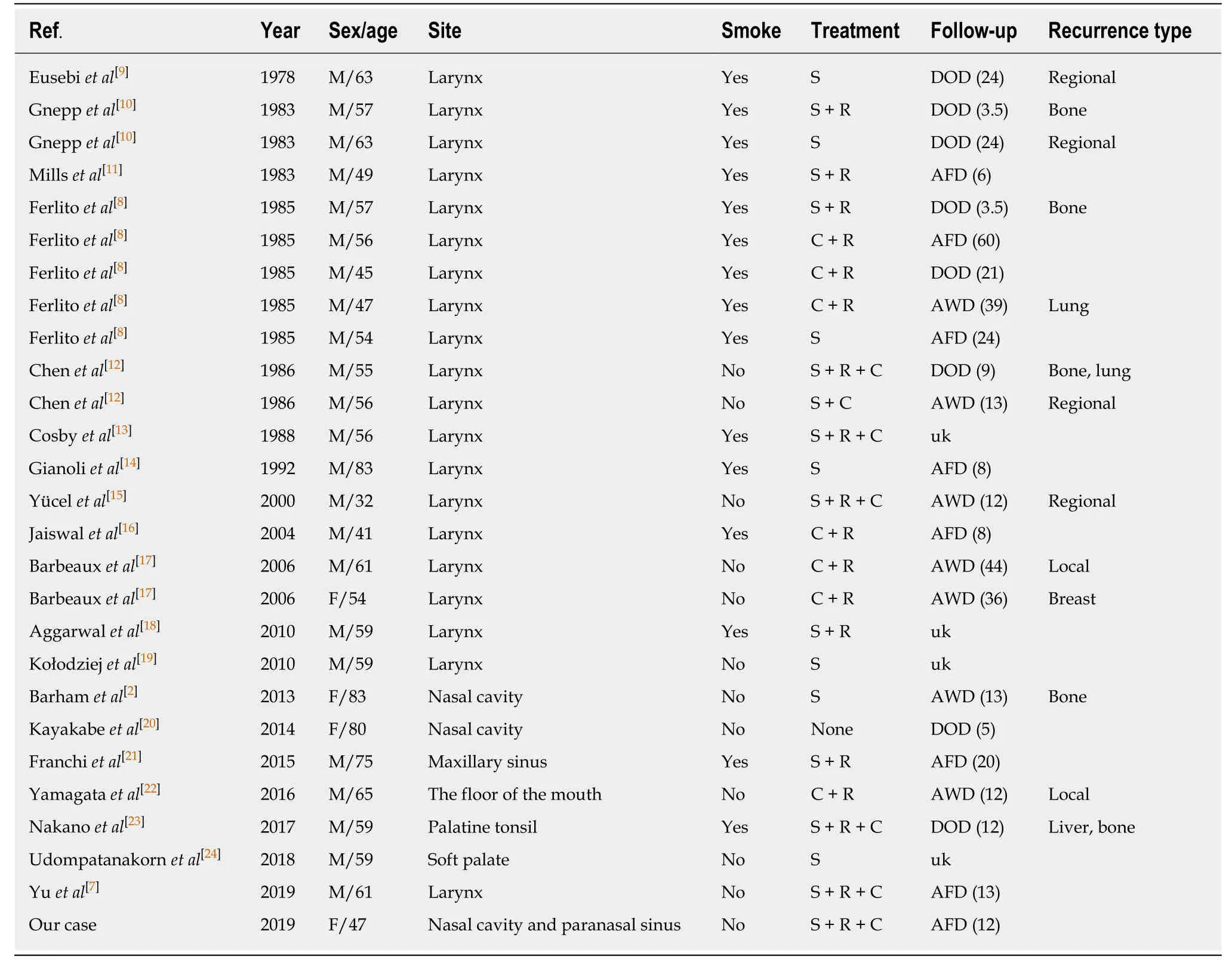
Table1 Summary of 27 cases of collision carcinoma of neuroendocrine carcinoma and squamous cell carcinoma in the head and neck
 World Journal of Clinical Cases2020年12期
World Journal of Clinical Cases2020年12期
- World Journal of Clinical Cases的其它文章
- Assessment of diaphragmatic function by ultrasonography:Current approach and perspectives
- Computer navigation-assisted minimally invasive percutaneous screw placement for pelvic fractures
- Research on diagnosis-related group grouping of inpatient medical expenditure in colorectal cancer patients based on a decision tree model
- Evaluation of internal and shell stiffness in the differential diagnosis of breast non-mass lesions by shear wave elastography
- Real-time three-dimensional echocardiography predicts cardiotoxicity induced by postoperative chemotherapy in breast cancer patients
- Lenvatinib for large hepatocellular carcinomas with portal trunk invasion:Two case reports
