Pelvic lipomatosis and renal transplantation:A case report
Jie Zhao,Ying-Xin Fu,Gang Feng,Chun-Bai Mo
Jie Zhao,Ying-Xin Fu,Gang Feng,Chun-Bai Mo,Department of Kidney Transplant,Tianjin First Central Hospital,Tianjin 300192,China
Abstract
Key words:Pelvic lipomatosis;Kidney transplantation;Uremia;Hydronephrosis;Bladder;Urinary obstruction;Case report
INTRODUCTION
Pelvic lipomatosis is a rare disease of unknown etiology,characterized by the overgrowth of pelvic adipose tissue that causes compression of the urinary tract including the bladder and ureters,rectum and blood vessels[1].These patients progressively develop obstructive uropathy,and 40% deteriorate into renal failure after an average period of five years[2-4].At present,there are no reports of renal transplantation due to uremia caused by pelvic lipomatosis.The bladder and iliac vessels are entirely wrapped in this abnormal fat,making it difficult to dissociate iliac vessels and bladder during renal transplantation.Urinary tract obstruction may occur again after renal transplantation.The ideal management of patients with pelvic lipomatosis after renal transplantation is not yet well-established due to the lack of literature and follow-up data.Here,we report a 37-year-old male patient with pelvic lipomatosis who received a successful living donor renal transplantation.
CASE PRESENTATION
Chief complaints
A 37-year-old male patient presented to our hospital with complaints of fatigue and vomiting for two weeks on November 18,2014.
History of present illness
On admission,a computed tomography (CT) scan showed bilateral severe hydronephrosis and a compressed and thick-walled bladder and extra fat tissues in the pelvis (Figure 1).The patient underwent cystoscopy,which showed an elongation of the prostatic urethra and elevation of the bladder neck.There were several bullous lesions over the wall of the neck and the trigone of the bladder.The bilateral ureteral orifices were not identified.A double “J” ureteral stent could not be placed appropriately.Tissue biopsy of the bladder demonstrated cystitis glandularis(Figure 2A).Bilateral percutaneous nephrostomy was performed under ultrasonographic guidance.Anterograde urography revealed bilateral hydronephrosis and tortuous dilated ureter,symmetrical compression and elevation of the bladder (a pear-shaped bladder) (Figure 3).Thus,a diagnosis of pelvic lipomatosis was confirmed.Despite an output of 1000-1500 mL urine in 24 h,renal function did not improve.The patient was diagnosed with end-stage renal disease and underwent hemodialysis.
History of past illness
He also had a history of persistent suprapubic pain and nocturia (2-3 times) for more than four years and a single episode of gross hematuria.
Physical examination
On admission,his height was 170 cm and weight was 71 kg,with a body mass index of 24.The physical examination revealed a palpable suprapubic mass and mild edema of both lower legs.
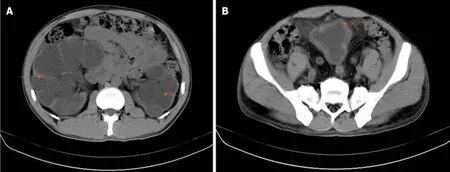
Figure 1 Computed tomography examination.A:Computed tomography showed bilateral hydronephrosis (orange arrow);B:A thick walled urinary bladder(orange arrow) with increased fat density around the bladder.
Laboratory examinations
His serum creatinine was 1500 µmol/L and hemoglobin was 79 g/L.
Imaging examinations
Anterograde urography revealed bilateral hydronephrosis and tortuous dilated ureter,symmetrical compression and elevation of the bladder (a pear-shaped bladder)(Figure 3).
FINAL DIAGNOSIS
End-stage renal disease,pelvic lipomatosis,hydronephrosis.
TREATMENT
Bilateral nephrectomy and living donor renal transplantation (kidney obtained from his brother) were performed on July 22,2015.The operation was complicated as the iliac vessels and bladder were completely wrapped in excessive abnormal fat.The external iliac artery and vein were located using ultrasonographic guidance.The adipose tissue around the right bladder was removed as far as possible,and the graft ureter was reimplanted into the bladder,using the Lich-Gregoir technique.Histopathological examination of the fat showed a benign lipomatous lesion(Figure 2B).The double “J” stents were removed three months after the operation.Serum creatinine was 120 µmol/L after transplantation.

Figure 3 Anterograde urography revealed bilateral hydronephrosis (thin orange arrow) and tortuous dilated ureter (orange arrow),symmetrical compression and elevation of the bladder (a pear-shaped bladder) (thick orange arrow).
OUTCOME AND FOLLOW-UP
At six months postoperatively,mild hydronephrosis in the graft kidney was identified by magnetic resonance urography (Figure 4A),and graft function was stable.However,B-ultrasound showed moderate hydronephrosis at 22 mo after transplantation.Graft percutaneous nephrostomy was performed under ultrasonographic guidance for urinary diversion (Figure 4B).During the four-year follow-up period,the patient was in a stable condition and serum creatinine was 121µmol/L.
DISCUSSION
Pelvic lipomatosis is a rare condition defined as a non-malignant overgrowth of normal fat in the pelvis.It was previously reported that the incidence of pelvic lipomatosis was 0.6-1.7 per 100000 hospital admissions in the United States[5].Clinical manifestations are due to various compression phenomena spanning the rectum(constipation,tenesmus),the urinary tract (lower urinary tract symptoms),and venous structures (lower limb edema and thrombosis).The best definitive diagnostic procedure is CT,which demonstrates increased adipose tissue surrounding the bladder and rectum.A pear-shaped bladder and hydronephrosis are common findings on the CT urogram and are important characteristic indications of pelvic lipomatosis[2].
However,the etiology of pelvic lipomatosis is unknown.To date,various methods to treat pelvic lipomatosis,including steroids,long-term antibiotics,weight reduction,and radiation therapy have been proven to be ineffective[1].The recommended management strategy includes close monitoring of the development and progression of hydronephrosis and renal function.When obstruction develops,an appropriate diversion can be performed by ureteral reimplantation,nephrostomy,ureterostomy or a conduit[6].Kleinet al[7]reported that urinary diversion was eventually required in 39% of patients during a 7.5-year follow-up period[7].The surgical removal of adipose tissue surrounding the bladder does not lead to a radiological abnormality or remission of the condition[8].
When bilateral hydronephrosis progresses,40% of patients deteriorate into renal failure after an average period of five years and kidney transplantation can be considered.Even though excision of the pelvic fat and dissection of adhesions of the external vessels and bladder may be difficult,transplantation is not entirely impossible.Reconstruction of the urinary tract can be considered according toconventional ureteral bladder replantation.The recurrence of graft urinary obstruction associated with pelvic lipomatosis is also possible.However,there are no literature reports on the recurrence of ureteral obstruction after renal transplantation.The recommended management strategy includes close monitoring of the graft renal function,and if progression due to obstruction is observed,urinary diversion should be considered.
We are also concerned that the graft renal vein and external iliac vein may be compressed by excess adipose tissue after the operation,leading to thrombosis.Currently,there are several reports of deep venous thrombosis in patients with pelvic lipomatosis[9-11].Schechter[9]reported a patient with venous thrombosis of the left iliac vein as a result of pelvic lipomatosis.Therefore,we administered aspirin to prevent venous thrombosis,and no thrombosis was found during the follow-up period.
CONCLUSION
When patients with pelvic lipomatosis develop renal failure,renal transplantation could be a feasible treatment strategy.
 World Journal of Clinical Cases2020年16期
World Journal of Clinical Cases2020年16期
- World Journal of Clinical Cases的其它文章
- Novel computerized psychometric tests as primary screening tools for the diagnosis of minimal hepatic encephalopathy
- Steroid-responsive pancreatitides
- Application of molybdenum target X-ray photography in imaging analysis of caudal intervertebral disc degeneration in rats
- Accuracy study of a binocular-stereo-vision-based navigation robot for minimally invasive interventional procedures
- Value of virtual bronchoscopic navigation and transbronchial ultrasound-guided sheath-guided exploration in diagnosis of peripheral lung cancer
- Significance of serum fibroblast growth factor-23 and miR-208b in pathogenesis of atrial fibrillation and their relationship with prognosis
