动脉瘤栓塞手术液固两相流数值模拟分析
张洋 樊俊杰 陈盈盈 陈广新 王汝良 任春娜
摘 要: 不同程度动脉瘤栓塞的红细胞颗粒运动状况数值模拟,应用液固两相流计算流体力学仿真,血液流動采用瞬态,血管壁采用刚性壁模拟。通过仿真计算,最终获取动脉瘤栓塞程度不同的两相流的血流状况:动脉瘤栓塞程度不同,导致动脉瘤内红细胞体积分数分布不同,血流速度分布、壁面切应力分布不同,栓塞也导致红细胞聚集现象不同。
关键词: 动脉瘤栓塞;多相流;红细胞聚集
中图分类号: TP391.4 文献标识码: A DOI:10.3969/j.issn.1003-6970.2020.07.029
本文著录格式:张洋,樊俊杰,陈盈盈,等. 动脉瘤栓塞手术液固两相流数值模拟分析[J]. 软件,2020,41(07):143-147+169
Numerical Simulation of Liquid-solid Two-phase Flow in Aneurysm Embolization
ZHANG Yang1, FAN Jun-jie2, CHEN Ying-ying3, CHEN Guang-xin3, WANG Ru-liang4, REN Chun-na3
(1. Department of Laboratory Medicine, Second Affiliated Hospital, Mudanjiang Medical College, Heilongjiang, Mudanjiang 157011;2. School of Health Management, Mudanjiang College of Medicine, Heilongjiang, Mudanjiang 157011;3. College of Medical Imaging, Mudanjiang Medical College, Heilongjiang, Mudanjiang 157011;4. Department of Radiology, Red Flag Hospital, Mudanjiang Medical College, Heilongjiang, Mudanjiang 157011)
【Abstract】: The Movement of Red Blood cell particles in different degrees of aneurysm embolization was simulated by liquid-solid flow simulation, transient blood flow simulation and rigid wall simulation, respectively. Finally, the blood flow of two-phase flow with different degrees of aneurysm embolization was obtained by simulation calculation. The different degrees of aneurysm embolization resulted in different distributions of red blood cell volume fraction, blood flow velocity and wall shear stress, embolization also causes different aggregations of red blood cells.
【Key words】: Aneurysm; Embolization; Multiphase flow; Erythrocyte aggregation
0 引言
颅内动脉瘤(Intracranial aneurysm,IA)是多种因素导致的动脉壁的异常瘤样扩张,常发生于颅内大动脉的分叉及弯曲处,破裂会导致蛛网膜下腔出血,具有极高的致死率及致残率。影响动脉瘤生长和破裂的因素主要包括先天生理性、病理性及血流动力学因素。对于IA的治疗主要包括开颅夹闭术及血管内介入栓塞两种方法[1-3]。无论是哪种方法,由于动脉瘤自身的复杂性及不完全闭塞的发生,即使是有经验的临床医生,术后的复发率依旧很高[4-7]。栓塞手术由于创伤小,操作相对简单等优势和栓塞材料及技术的不断发展进步逐渐被广泛应用于临床。但同时由于弹簧圈具有可压缩性使得动脉瘤复发的可能性大大增加,有研究表明栓塞程度是动脉瘤复发的重要影响因素,Brzegowy等人回顾性分析破裂与未破裂前交通动脉瘤的栓塞治疗,同样得出影响颅内动脉瘤复发的最大因素就是栓塞密度,初始栓塞的不完全极易引起动脉瘤的复发[8-9]。栓塞程度低,弹簧圈会随着血流的冲击逐渐压缩,进而向远侧移位、复发。赵庆平等提出瘤腔内的血流速度与瘤腔大小呈负相关,即栓塞程度越低,腔内血流速度加快时,血液对壁面产生的力就可能导致动脉瘤的复发[10]。但这些研究并未明确指明血流动力学因素在不同栓塞程度下的变化。近年来随着计算机的发展及有限元软件的开发,尤其是计算流体动力学数值模拟方法的应用,使得血流建模能更好解释血流动力学在IA发病机制中的作用[11-16]。因此为了探究不同栓塞密度下血流动力学的具体变化,建立了不同栓塞程度的模型,来为临床医生制定更好的栓塞策略提供指导。
1 材料与方法
1.1 个体化模型构建
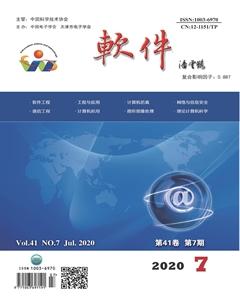
本文研究采用牡丹江医学院附属红旗医院影像科提供的一例真实基底动脉顶端动脉瘤患者的DICOM格式的头部CTA影像资料。动脉瘤CTA影像显示位置如图1所示。
在MIMICS软件(Materialise公司,比利时)中,对DICOM格式数据进行阈值分割、三维重建,然后利用3-matic(Materialise公司,比利時)软件对获取的初步模型去除细小分支血管、保留载瘤动脉血管,截取出、入口平面,最后对三角面片进行光滑,获取动脉瘤的理想模型[17-18](图2)。
为了比较不完全栓塞、完全栓塞、栓塞手术前的动脉瘤血流动力学参数的差异,本文在栓塞数千的动脉瘤模型基础上构建了中度栓塞和完全栓塞的模型(图3)。
1.2 网格划分
利用ANSYS FLUNET MESHING软件对术前动脉瘤模型、不完全栓塞动脉瘤模型、完全栓塞动脉瘤模型进行四面体网格划分,为保证计算精度,边界层6层加密。
1.3 血液两相流控制方程
血液为有形成分与血浆组成。血浆占血液总体积的55%,而悬浮在血浆中的有形成分主要是红细胞、白细胞、血小板三类,其中红细胞占95%[19-20]。在液固两相流模型中,考虑到血细胞中绝大部分是红细胞而在计算中忽略其它有形成分的影响,假设血液是由红细胞悬浮于血浆构成的两相流系统。液相(连续相):血浆设为不可压缩的牛顿流体。固相(离散相):红细胞设定为球形刚性颗粒,颗粒液固两相流的控制方程为[21-25]:
1.4 边界条件与参数设定
利用ANSYS FLUENT计算流体力学分析软件进行瞬态仿真计算。边界条件设定为:入口为速度入口,液相与固相采用相同的速度波形。速度入口曲线如图4所示。
2 计算结果
2.1 红细胞体积分数
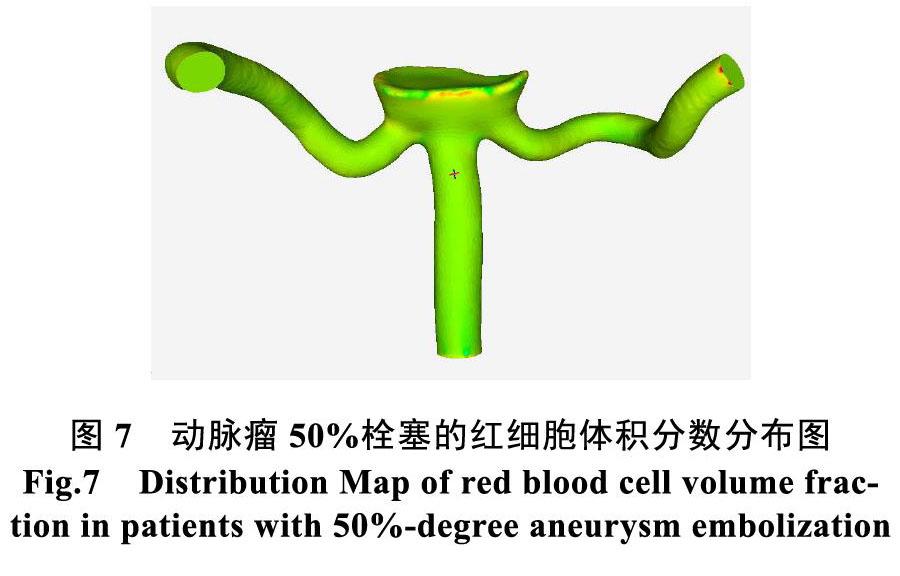
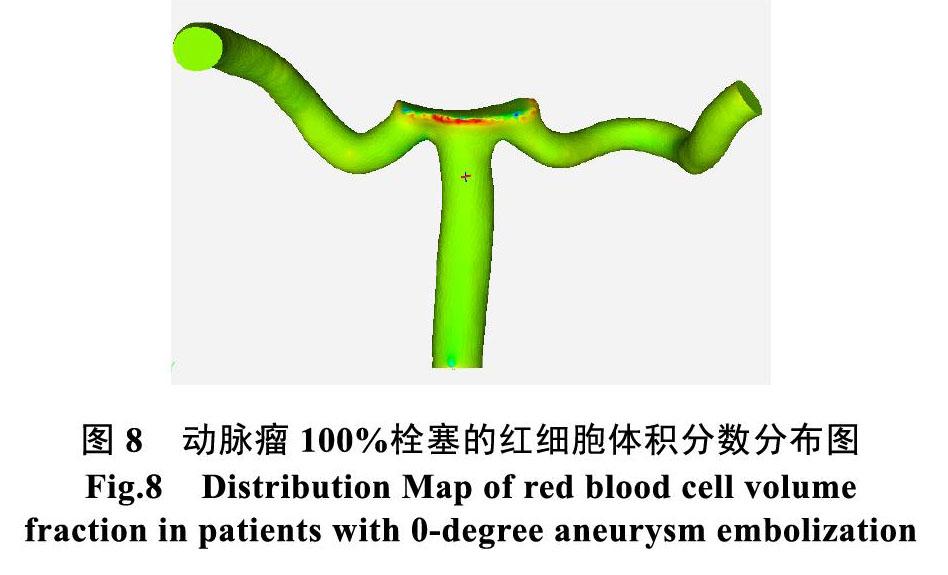
图5为动脉瘤入口红细胞速度达到峰值时刻图,选取红细胞速度达到峰值时刻的动脉瘤0度栓塞、50%栓塞、100%栓塞的动脉瘤红细胞体积分数图进行分析(图6、图7、图8)。由图可见,在动脉瘤栓塞0度时,动脉瘤的红细胞在瘤颈处出现局部、少量的聚集现象,这一点符合真实临床诊断,动脉瘤50%栓塞在瘤壁顶端形成较明显的聚集情况,而动脉瘤100%栓塞在瘤壁顶端形成更为明显的聚集情况。动脉瘤的红细胞聚集则形成血栓。
2.2 血液速度场
本文通过计算,比较了三种不同程度栓塞的动脉瘤流场分布,如图9、10、11所示,动脉瘤0度栓塞、动脉瘤50%栓塞、动脉瘤100%栓塞均出现不同程度的涡流,流体从载瘤管方向冲向瘤颈远端,然后顺着瘤壁形成涡流,涡流的中心偏向瘤颈的远端,载流管内的有形颗粒进入流体内部并在涡流中心停留堆积,最终形成血栓。50%程度栓塞时,瘤内的速度相较于0程度栓塞较快,说明栓塞起到了提高瘤内的血液流动能力,而相较于100%栓塞程度的动脉瘤,50%不完全栓塞的动脉瘤的流线存在不稳定现象。
2.3 壁面剪切应力分布
为便于观察,在瘤颈处选择一点为观察点。图12、图13、图14为动脉瘤0度栓塞、动脉瘤50%栓塞、动脉瘤100%栓塞的观察点壁面切应力随时间变化曲线。由三个图可见,动脉瘤瘤壁的壁面压力随时间变化,但随着动脉瘤的栓塞程度变化为栓塞程度越大,壁面压力越大,说明栓塞有助于改变壁面压力程度。瘤顶附近的剪切应力不足 , 将导致了血管内皮 细胞出现变形和功能退化, 所以瘤顶区域为高危易破裂的区域,栓塞手术可降低破裂风险。
3 结论与展望
本文通过对动脉瘤0度栓塞、50%栓塞、100%栓塞进行了多项流颗粒物数值模拟,得出以下结论:
(1)动脉瘤栓塞程度越高越有利于红细胞在动脉瘤中的浓度极化,形成血栓。
(2)动脉瘤栓塞程度越高,越降低流场的涡流程度。
(3)动脉瘤的栓塞程度越高,可提高瘤壁的壁面剪切应力,降低动脉瘤破裂风险。
本文的创新之处在于在动脉瘤数值模拟中考虑了红细胞颗粒运动的影响,分析了红细胞运动在动脉瘤栓塞手术中的浓度极化现象。本文不足之处在于样本量不足,因此,在下一步研究中应增加临床样本量;此外,考虑到实验技术条件所限,本文计算采用的时血管刚性壁,血管壁实际为弹性壁,在下一步研究中,将拓展到超弹性结构的血管壁与血液双向流固耦合分析。
参考文献
-
Wang Hua-Wei, Sun Zheng-Hui, Wu Chen et al. Surgical management of recurrent aneurysms after coiling treat?ment[J]. Br J Neurosurg, 2017, 31: 96-100.
-
Phan Kevin, Huo Ya R, Jia Fangzhi et al. Meta-analysis of stent-assisted coiling versus coiling-only for the treatment of intracranial aneurysms[J]. J Clin Neurosci, 2016, 31: 15-22.
-
Gawlitza Matthias, Soize Sebastien, Januel Anne-Christine et al. Treatment of recurrent aneurysms using the Woven EndoBridge(WEB): anatomical and clinical results[J]. J Neurointerv Surg, 2018, 10: 629-633.
-
Huang De-Zhang, Jiang Bin, He Wei et al. Risk factors for the recurrence of an intracranial saccular aneurysm following endovascular treatment[J]. Oncotarget, 2017, 8: 33676- 33682.
-
Yu Le-Bao, Fang Zhi-Jun, Yang Xin-Jian et al. Management of Residual and Recurrent Aneurysms After Clipping or Coiling: Clinical Characteristics, Treatments, and Follow-Up Outcomes[J]. World Neurosurg, 2019, 122: e838-e846.
-
Zhang Donghuan, Wang Honglei, Liu Tianyi et al. Re-Recurrence of Intracranial Aneurysm with Proximal Vascular Stenosis After Primary Clipping and Secondary Endovascular Embolization: A Case Report and Literature Review[J]. World Neurosurg, 2019, 121: 28-32.
-
Kim S-T, Baek J W, Jin S-C et al. Coil Embolization in Patients with Recurrent Cerebral Aneurysms Who Previously Underwent Surgical Clipping[J]. AJNR Am J Neuroradiol, 2019, 40: 116-121.
-
Brzegowy Pawe?, Kucyba?a Iwona, Krupa Kamil et al. Angiographic and clinical results of anterior communicating artery aneurysm endovascular treatment[J]. Wideochir Inne Tech Maloinwazyjne, 2019, 14: 451-460.
-
Chueh Ju-Yu, Vedantham Srinivasan, Wakhloo Ajay K et al. Aneurysm permeability following coil embolization: packing density and coil distribution[J]. J Neurointerv Surg, 2015, 7: 676-81.
-
Zhao Qingping, Chen Guangzhong, Li Tielin, Zhao Wei, Yuan Yuan, Feng Yanqiu. Hemodynamic analysis of embolization density and recurrence of intracranial aneurysm[J]. Chinese Journal of neuropsychiatric diseases, 2013, 39(06): 339-343
-
Liang Li, Steinman David A, Brina Olivier et al. Towards the Clinical utility of CFD for assessment of intracranial aneurysm rupture-a systematic review and novel parameter- ranking tool[J]. J Neurointerv Surg, 2019, 11: 153-158.
-
Valen-Sendstad Kristian, Bergersen Aslak W, Shimogonya Yuji et al. Real-World Variability in the Prediction of Intracranial Aneurysm Wall Shear Stress: The 2015 International Aneurysm CFD Challenge[J]. Cardiovasc Eng Technol, 2018, 9: 544-564.
-
Roloff Christoph, Stucht Daniel, Beuing Oliver et al. Comparison of intracranial aneurysm flow quantification techniques: standard PIV vs stereoscopic PIV vs tomographic PIV vs phase-contrast MRI vs CFD[J]. J Neurointerv Surg, 2019, 11: 275-282.
-
Frolov S V, Sindeev S V, Liepsch D et al. Experimental and CFD flow studies in an intracranial aneurysm model with Newtonian and non-Newtonian fluids[J]. Technol Health Care, 2016, 24: 317-33.
-
Botti Lorenzo, Paliwal Nikhil, Conti Pierangelo et al. Modeling hemodynamics in intracranial aneurysms: Comparing accuracy of CFD solvers based on finite element and finite volume schemes[J]. Int J Numer Method Biomed Eng, 2018, 34: e3111.
-
Xiang J, Tutino V M, Snyder K V et al. CFD: computational fluid dynamics or confounding factor dissemination? The role of hemodynamics in intracranial aneurysm rupture risk assessment[J]. AJNR Am J Neuroradiol, 2014, 35: 1849-57.
-
Resnick Nitzan, Yahav Hava, Shay-Salit Ayelet et al. Fluid shear stress and the vascular endothelium: for better and for worse[J]. Prog. Biophys. Mol. Biol., 2003, 81: 177-99.
-
Davies Peter F, Hemodynamic shear stress and the endothelium in cardiovascular pathophysiology[J]. Nat Clin Pract Cardiovasc Med, 2009, 6: 16-26.
-
Shojima Masaaki, Oshima Marie, Takagi Kiyoshi et al. Magnitude and role of wall shear stress on cerebral aneurysm: computational fluid dynamic study of 20 middle cerebral artery aneurysms[J]. Stroke, 2004, 35: 2500-5.
[20] Boussel L, Rayz V, Mcculloch C, et al. Aneurysm Growth Occurs at Region of Low Wall Shear Stress: Patient-Specific Correlation of Hemodynamics and Growth in a Longitudinal Study[J]. Stroke, 2008, 39(11): 2997-3002.
[21] Reneman Robert S, Arts Theo, Hoeks Arnold P G, Wall shear stress--an important determinant of endothelial cell function and structure--in the arterial system in vivo. Discrepancies with theory[J]. J. Vasc. Res., 2006, 43: 251-69.
[22] Yeow Siang Lin, Leo Hwa Liang, Is Multiple Overlapping Uncovered Stents Technique Suitable for Aortic Aneurysm Repair?[J]. Artif Organs, 2018, 42: 174-183.
[23] Suzuki Tomoaki, Stapleton Christopher J, Koch Matthew J et al. Decreased wall shear stress at high-pressure areas predicts the rupture point in ruptured intracranial aneurysms[J]. J. Neurosurg., 2019, undefined: 1-7.
[24] Omodaka Shunsuke, Sugiyama Shin-Ichirou, Inoue Takashi et al. Local hemodynamics at the rupture point of cerebral aneurysms determined by computational fluid dynamics analysis[J]. Cerebrovasc. Dis., 2012, 34: 121-9.
[25] Dabagh Mahsa, Nair Priya, Gounley John et al. Hemo-
dynamic and morphological characteristics of a growing cerebral aneurysm[J]. Neurosurg Focus, 2019, 47: E13.
[26] Zhang Yisen, Jing Linkai, Zhang Ying et al. Low wall shear stress is associated with the rupture of intracranial aneurysm with known rupture point: case report and literature review.[J]. BMC Neurol, 2016, 16: 231.
[27] Liu Xiuxian. Hemodynamic study of surgical treatment of intracranial aneurysm[D]. Southeast University, 2017
[28] Chang Yu, Liu Chang, Zhang Qi, Shi Yue, Gao Bin. Hemodynamic study on the influence of Subarachnoid Aneurysm on the risk of cerebral aneurysm rupture[J]. Journal of Beijing University of technology, 2017, 43(07): 1079-1085. Computational fluid dynamics analysis[J]. Cerebrovasc. Dis., 2012, 34: 121-9
[29] Murayama Yuichi, Fujimura Soichiro, Suzuki Tomoaki et al. Computational fluid dynamics as a risk assessment tool for aneurysm rupture.[J]. Neurosurg Focus, 2019, 47: E12.
[30] Sheng Bin, Wu Degang, Yuan Jinlong et al. Hemodynamic Characteristics Associated With Paraclinoid Aneurysm Recurrence in Patients After Embolization[J]. Front Neurol, 2019, 10: 429.