Intraorbital wooden foreign bodies: case series and literature review
Ya-Yan You, Bing-Jie Shi, Xin-Yan Wang, Jin Chen, Zheng-Rong Wang, Xing-Hua Wang,Fa-Gang Jiang
Department of Ophthalmology, Union Hospital, Tongji Medical College, Huazhong University of Science and Technology, Wuhan 430022, Hubei Province, China
Abstract
● KEYWORDS: orbit; foreign body; wooden; trauma; infection
INTRODUCTION
Intraorbital foreign bodies (IOFBs) are typically caused by a high-velocity trauma to the orbit but may also occur after relatively trivial trauma[1], constitute 16.7% of orbital injuries[2-4]. While most IOFBs are metallic or glass particles,intraorbital wooden foreign bodies (IOWFBs) are relatively rare[5]. However, compared with metals and glasses, IOWFBs could induce much higher risk if misdiagnosed or missed diagnosis, and severe intraorbital complications, such as orbital cellulitis, abscess formation, exophthalmos, and extraocular muscle damage might occur[6].
The diagnosis of IOWFBs is sometimes difficult due to insufficient information regarding history of trauma, as well as the insufficiency in the external signs. In addition, radiologic diagnosis of IOWFBs is always uncertain and quite difficult,because the low density of IOWFBs is similar to air and adipose tissue on initial computed tomography (CT)[4].Therefore, IOWFBs are frequently omitted and may not be confirmed until days or months after the initial injury. For better understanding and management of IOWFBs, we report here a review that included literature from PubMed and Web of Science as well as our five cases (Tables 1[6-48]and 2). The purpose is to provide comprehensive information regarding the clinical manifestations, diagnosis, and surgical treatment of IOWFBs.
METHODS OF SEARCH
Relevant literatures were reviewed through a search of the PubMed and Web of Science database (1971 to December 01,2019). The search terms included “intraorbital foreign body”;“intraorbital plant foreign body” or “intraorbital organic foreign body” or “intraorbital wooden foreign body” and “case report” or “case series”. After removal of the review articles and duplicate publications, 72 articles were included. The full texts were reviewed, 24 articles excluded with reasons:full text is not English, or full text is not available, or the study was performed in animals, or non-wooden intraorbital foreign body. Finally, we included 43 case reports with 46 patients (Table 1), and five case series with 108 patients who had IOWFBs (Table 3). Informed consent was obtained from the patient for publication of this case report details.
ORIGINAL CASE REPORTS
Case 1 A 30-year-old man presented to the local hospital with pain and complete ptosis in his left eye after a fall in a farmland. There was no light perception in his left eye and the wound was visible in the lower eyelid (Figure 1A). No foreign body was found on CT, and then the emergency debridement was performed. Since a purulent fistula was exhibited after surgery, he was admitted to our hospital three days later. A low-density foreign body was found in the reexamination CT (Figure 1B), which was also confirmed in magnetic resonance imaging (MRI; Figure 1C).Aspergillusinfection was confirmed based on a fungal test. Eventually, a branch approximately 5 cm long were removed, and the sinus was repaired surgically under general anesthesia (Figure 1D).The patient’s wound was healed one week postoperatively, but the complete blindness, ptosis and eyeball fixation continued without any improvement.
Case 2 A 33-year-old man had complaints of right eyelid swelling and binocular diplopia for 2wk after an accident fall in an orchard. The wound in the lower eyelid of his right eye had been sutured in the local hospital (Figure 2A). The patient’s best-corrected visual acuity was 20/25 OD and 20/20 OS. The right eye had a fistula with mucinous secretions in the lower eyelid, with conjunctival congestion, subconjunctival hemorrhage, exophthalmos, and ocular movement restriction.Surgical exploration was still performed due to the clinical manifestations, although no foreign body was found in CT and MRI (Figure 2B, 2C). Ultimately, 19 branches and debris were successfully removed (Figure 2D).
Case 3 A 46-year-old man suffered an injury caused by a wooden chopstick in a fight 2d prior. He was transferred to our hospital with a round wound above the inner canthus of the right eyelid (Figure 3A), accompanied by pain in eye movement, facial numbness, difficulty in mouth opening and weakness in mastication. Ophthalmologic examination revealed conjunctival congestion and chemosis, extraocular movement restriction with mild proptosis, and 25/20 visual acuity. CT showed a low-density tubular foreign body extended from the right orbit to the masseter muscle (Figure 3B). MRI also showed the trajectory of this low-signal foreign body (Figure 3C). With general anesthesia, a cross-orbital wooden chopstick was successfully extracted (Figure 3D).
Case 4 A 9-year-old boy was transferred from a local hospital for “potential IOFBs” following a penetrating injury to the right eyelid by a bamboo stick. Ophthalmic evaluation revealed a swollen right upper eyelid with a 2-cm sutured wound, and severe ptosis that covered two-thirds of the cornea (Figure 4A). CT suggested two wooden foreign bodies in the orbit(Figure 4B), but MRI was negative (Figure 4C). Unexpectedly,during surgical exploration, four wooden debris (three large and one small) were removed from the orbit (Figure 4D). No complications were observed after half a year follow-up.
Case 5 A 3-year-old girl presented to our hospital with a 2×1 cm2mass on the left upper eyelid (Figure 5A). Her parents reported that she had been stabbed by a sesame stick on her left upper eyelid, 2y prior. According to the orbital CT and B-ultrasound examination (Figure 5B, 5C), and combined with trauma history and presentation, wooden foreign bodies were suspected in the orbit. During surgery, two pieces of sesame stem residue and the eyelid abscess were removed (Figure 5D).The patient exhibited no complications in the follow-up after three months.
The following information of 51 patients was extracted from our case and the published case reports: sex, age, the eye,cause, duration, clinical features, entry site, extraorbital tissue injury, number of surgeries and imaging findings.
DISCUSSION AND LITERATURE REVIEW Demographic Date
Frequency/incidence Although IOFBs occur with a frequency of 16.7% orbital injuries, the incidence of IOWFBs in general population are not available.
Sex and age IOWFBs have been reported to mainly occur in young and middle-aged men[19,49-50]. Of the 51 patients with IOWFBs, 35 (68.6%) were male and 16 (31.4%) were female(Table 2); the mean age was 27.3±18.2y (range 1-66y).
Cause of Injuries and Original Traumatic Entrance Of the 51 patients in this review, the main causes of injuries in IOWFBs were falls and stabs, accounting for 49% (n=25/51)and 41.2% (n=21/51), respectively (Table 2). The most original traumatic entrances of the 51 patients were eyelid (n=36/51,70.6%) and conjunctiva (n=7/51, 13.7%; Table 2), which were consistent with Shelstaet al[5](9/23, 39.1% in eyelid and 10/23,43.5% in conjunctiva) and Liet al[51](11/14, 78.6% in eyelid and 3/14, 21.4% in conjunctiva; Table 3).
Clinical Features
Presenting symptoms Periorbital redness and swelling,conjunctival congestion and chemosis, ptosis, proptosis,extraocular movement restriction, and visual impairment have been reported as common clinical manifestations of IOWFBs[41]. Consistent with these manifestations, the 51 cases revealed that the most common manifestation of IOWFBs was extraocular movement restriction (n=27/51, 52.9%), followed by visual impairment (n=25/51, 49.0%; Table 2); blindness may occur in patients with severe injuries, as reported inprevious literatures[7-8,13,36-37,46,48]and in our report (Case 1;Table 1). Less common clinical manifestations included diplopia(n=9/51, 17.6%) and mass (n=4/51, 7.8%; Table 2). These results revealed that the clinical manifestations of IOWFBs were diversified and non-specific.

Table 1 Summary of the 51 cases of intraorbital wooden foreign bodies (continued)
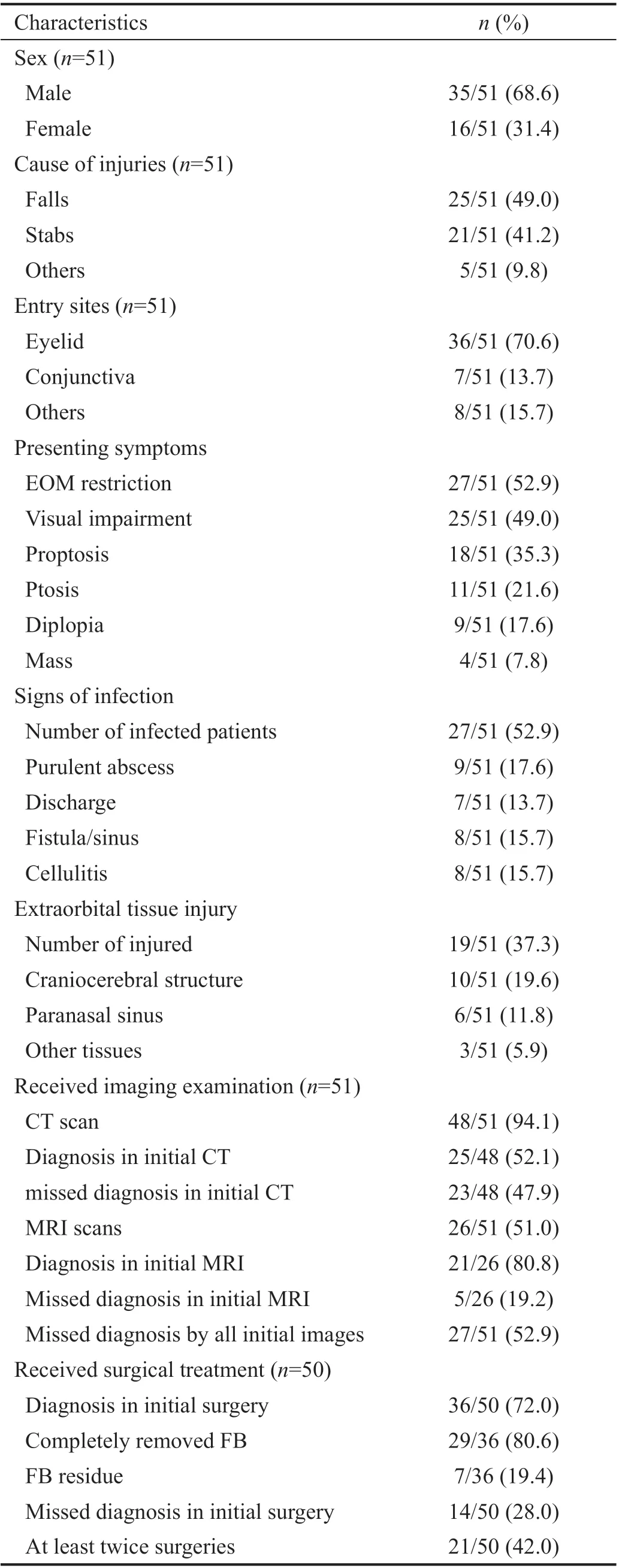
Table 2 Characteristics of 51 cases of intraorbital wooden foreign bodies
Signs of infection The organic nature and porosity of wood make it easy for microorganism to adhere and grow[12,23],retained wooden foreign bodies may cause suppuration[6].Among the 51 cases, 27 of 51 patients (52.9%) were infected,the signs of infection included purulent abscess (n=9/51,17.6%), discharge (n=7/51, 13.7%), fistula/sinus (n=8/51,15.7%) and cellulitis (n=8/51, 15.7%; Table 2). Consequently,it is essential to intervene in time when IOWFBs were suspected, as more than half of the IOWFBs may develop orbital infection.
Extraorbital Tissue Injury IOWFBs may extend to extraorbital tissue and cause serious complications, as shown in Case 3. Our review showed that 37.3% of the 51 patients had extraorbital tissue injuries; the most common extraorbital location invaded by IOWFBs was the craniocerebral structure(n=10/51, 19.6%), followed by paranasal sinus (n=6/51, 11.8%;Table 2). Therefore, the eyeball and the periocular tissue should be thoroughly examined when foreign bodies invade the orbit. If the extraorbital tissue is affected, consultations of neurologists or otolaryngologists are needed.
Imaging Diagnosis Since IOWFBs present non-specific clinical manifestations, missed diagnosis in the early stage of trauma is not rare. Reports by Liu[52], Shelstaet al[5], and Liet al[51]revealed preoperative missed diagnosis rates were 88.9%, 13.0%, and 21.4%, respectively (Table 3). Therefore,imaging modalities such as CT and MRI are needed in the discovery of IOWFBs; other imaging modalities, such as X-ray and ultrasound, are occasionally used[53-54].
X-ray and ultrasound X-ray is not often used to detect IOWFBs because wood cannot be identified by this modality.Notably, the 4 of 51 patients[20-21,31,41]initially underwent X-ray,but no foreign bodies were found. Ultrasound has an advantage in the diagnosis of long-lasting IOWFBs[55], as shown in Case 5 (Table 1). The imaging findings include irregular spaceoccupying lesions of granulation tissue, low echo purulent cavity[55]or strong echo spots within the lesion. However,ultrasound is rarely used in the clinical diagnosis of IOWFBs because foreign bodies are not always visible and cannot be accurately located in examinations[31].
Computerized tomography CT is regarded as the gold standard[44-45,47,53], even though the review showed that initial CT scan missed up to 47.9% (n=23/48) of IOWFBs (Table 2),which slightly differed from the 35% reported by Shelstaet al[5](Table 3). Studies have shown that manifestation of wood on CT varies with the interval since the trauma. In the acute stage,wood appears as a low-density similar to air, which is also common in orbital trauma. Thus, it is difficult to identify in the initial visit, especially for small pieces of wood. However, in the subacute stage, wood becomes moderate density similar to orbital fat[2,6,49]. In the chronic stage, wood shows high density which is markedly visible on CT[6].
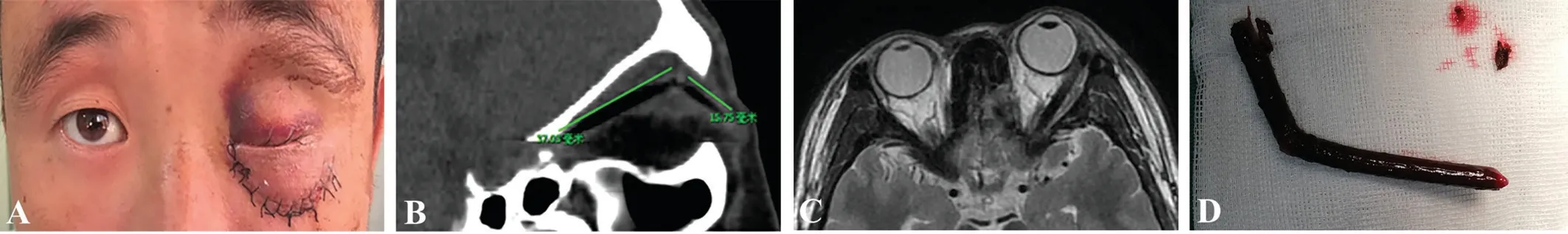
Figure 1 A 30-year-old man with an IOWFB in his left eye after falling in a field A: His left eye exhibited redness and swelling with a fistula that exuded discharge at the lower eyelid wound and the eye also demonstrated ptosis; B: The sagittal CT scan showed a thin tubular extremely low-density shadow (similar to gas shadow) in the orbit; C: A hypointense shadow appeared on T2-weighted images; D: A branch approximately 5 cm long was taken out.

Figure 2 A 33-year-old man with IOWFBs in his right eye after falling A: Initial physical examination showed the palpebral fissure had become small and a skin suture was observed in the right lower eyelid with a fistula that exuded discharge; B: CT images revealed fracture of the right orbit and maxillary sinus, gas shadow accumulation around the right orbit, tortuosity of the right optic nerve, and swelling of extraocular muscles; C: MRI detected swelling of the right eyelid with effusion of the right maxillary sinus, as well as increased and mixed signal on T2-weighted images; D: 19 branches and debris of different sizes were taken out successfully.

Figure 3 A 46-year-old man injured by a wooden chopstick from fighting A: A 46-year-old man with a round wound above the inner canthus of the right eyelid; B: CT images showed a tubular shadow in the right orbit, which was inclined downward from the inner canthus along the inner rear of the eyeball and extended to the masseter muscle; the images also showed fracture of the inferior orbital wall and outer wall of the right maxillary sinus; C: MRI examination showed a rod-shaped low signal shadow from the right orbit to the masseter muscle; D: An 8.6-cm wooden chopstick was removed through debridement.

Figure 4 The photograph of a 9-year-old boy who was stabbed by a bamboo stick A: A swollen right upper eyelid with a 2-cm healed wound and upper eyelid ptosis that covered two-thirds of the cornea; B: CT scan manifested two slightly high-density nodular shadows located posterosuperior to the eyeball, which were 2×4 mm2 and 1×2 mm2 respectively; C: MRI revealed that the soft tissue in the upper part of the eyeball and the subcutaneous tissue of the upper eyelid were both thickened, and T2-weighted images showed that this thickening was uneven;D: Four wooden debris (three large and one small) were removed.

Figure 5 A 3-year-old girl presented with an eyelid mass for 2y A: A 3-year-old girl developed eyelid mass 2y after being stabbed by a sesame rod with the 2×1 cm2 lump on the left upper eyelid; B: Coronal CT scan showed the swollen eyelid soft tissue with a small dot-like dense shadow; C: B-ultrasound images were suggestive of an 11.1×5.7 mm2 low echo mass with irregular shape and clear boundary; D: Two pieces of sesame stem residue were removed.

Table 3 Summary of case series of intraorbital wooden foreign bodies
Magnetic resonance imaging The wood appears hypointense relative to intraorbital fat on all MRI scans, regardless of its hydration[40]. Although we found that 19.2% (n=5/26) of IOWFBs in this review were still omitted in the initial MRI examination (Table 2). However, MRI scans are superior to CT in diagnosis of small pieces of wood, especially T1-weighted images[48,56]. Both T1-weighted and proton density sequences show brighter images of fatty tissue, compared with T2-weighted sequences. Thus, the contrast between fatty tissue and wood is more obvious because the adipose tissue is brighter[56]. Furthermore, T1-weighted images require less scanning time than proton density or T2-weighted images,which could reduce the probability of motion artifacts during imaging[56]. Therefore, T1-weighted images are better than proton density or T2-weighted images for diagnosis of IOWFBs. Overall, MRI should be performed if a wooden foreign body is suspected despite a negative CT[38].
Missed diagnosis by all initial images The overall rate of missed diagnosis of IOWFBs by all initial imaging examinations (including X-ray, ultrasonography, CT, or MRI)was 52.9% (n=27/51; Table 2). It emphasizes that IOWFBs cannot be completely excluded despite the negative imaging.Long-term follow-up and the re-examination of imaging should be suggested.
Treatment Strategy Surgery remains the preferred treatment for IOWFBs. In this review, surgeries were performed in 50 of 51 patients with IOWFBs. Of these, the rate of missed diagnosis and the rate of residual foreign bodies before the initial surgeries were 28.0% (n=14/50) and 19.4% (n=7/36),respectively (Table 2). Just as foreign bodies were not noticed during the debridement in local hospital in our Case 1 and 2.About 42.0% (n=21/50) of patients received at least twice surgeries (Table 2). Therefore, in terms of surgery, we suggest:First, the original traumatic entrance, the top of a fistula, the center of a granuloma and abscess can be chosen for the initial surgical incision; Second, since the wood usually shatters,meticulous exploration needs to continue despite the discovery of a foreign body; Last, if a fistula or an abscess exists,complete removal of the necrotic tissue, irrigation of antibiotic saline and placement of a drainage strip is essential.
Management However, there were several suggestions for the treatment of IOWFBs patients. First of all, we should evaluate the severity of trauma patient at the first visit. For the patients with orbital or ocular open wound, we should consider emergency surgery of debridement and suture.However, CT examination should be suggested for the patient with suspicious orbital foreign bodies. Furthermore, MRI examination should be recommended for the patients who was suspected of IOWFBs and ruled out of metal foreign body by CT examination. Second, attention should be paid to the details of foreign body removal surgery. Careful exploration and thorough removal of necrotic tissue during the surgery could help avoid residual foreign bodies. Meanwhile, intraoperative irrigation with antibiotic saline and postoperative anti-infection treatment could reduce postoperative infection and improve the prognosis of patients. Last but not least, we should notice the postoperative infection and suspicious residual of broken or decomposed foreign bodies after surgery. The re-examination of CT and MRI imaging should be suggested if the sign of infection presents, such as fistula or abscess. Also, long-term follow-up is necessary for the local chronic inflammatory and formation of foreign body granuloma.
CONCLUSION
IOWFBs are uncommon in patients with orbital trauma, and are mainly encountered in young men. Due to the diversity in the clinical manifestations and imaging characteristics of IOWFBs, misdiagnosis and missed diagnosis often occur during the initial visit. An accurate diagnosis requires a detailed trauma history, careful ocular examination, as well as empirical reading of imaging examinations. Although CT is regarded as the gold standard, MRI scans are superior to CT in diagnosis of small pieces of wood. Surgery is the preferred treatment, in which the surgeons should carefully remove all foreign bodies and residual fragments will result orbital infection. Postoperative sinus drainage and systemic antibiotic treatments are necessary.
ACKNOWLEDGEMENTS
Foundations:Supported by the National Natural Science Foundation of China (No.81900912); Project of Natural Science Foundation of Hubei Province (No.2019CFB700).
Conflicts of Interest:You YY, None; Shi BJ, None; Wang XY, None; Chen J, None; Wang ZR, None; Wang XH, None;Jiang FG, None.
 International Journal of Ophthalmology2021年10期
International Journal of Ophthalmology2021年10期
- International Journal of Ophthalmology的其它文章
- Exosomal miR-29b found in aqueous humour mediates calcium signaling in diabetic patients with cataract
- Intraluminal stenting versus external ligation of Ahmed glaucoma valve in prevention of postoperative hypotony
- Visual acuity after intravitreal ranibizumab with and without laser therapy in the treatment of macular edema due to branch retinal vein occlusion: a 12-month retrospective analysis
- Dexamethasone intravitreal implant (Ozurdex) in diabetic macular edema: real-world data versus clinical trials outcomes
- Comparative analysis of the clinical outcomes between wavefront-guided and conventional femtosecond LASlK in myopia and myopia astigmatism
- Reliability of the ocular trauma score for the predictability of traumatic and post-traumatic retinal detachment after open globe injury
