Recurrent hyphema after trabeculectomy: an atypical case of Swan syndrome
Pierre Leroux, Amina Rezkallah, Laurent Kodjikian,2, Olivier Loria,2, Thibaud Mathis,2,Philippe Denis,3
1Department of Ophthalmology, Croix-Rousse University Hospital, Hospices Civils de Lyon, University of Lyon, Lyon 69004, France
2University of Lyon 1, UMR-CNRS 5510 Matéis, Villeurbanne 69100, France
3Stem Cell and Brain Research Institute, INSERM U1208,Bron 69500, France
Dear Editor,
Trabeculectomy is the gold standard surgery for treatment of glaucoma. Early complications include wound leaks, responsible for ocular hypotony and serous choroidal detachment, and bleb fibrosis. Postoperative hyphema is also a well-known complication, most frequently induced by iris bleeding from the peripheral iridotomy. In most cases, bleeding occurs in the first months after surgery. We report here the case of an atypical anterior chamber bleeding occurring years after trabeculectomy. The bleeding was attributed to a neovessel observed at the scleral wound, making for an unusual presentation of Swan syndrome.
Ethical Approval The study was conducted in accordance with the principles of the Declaration of Helsinki. The informed consent was obtained from the patient.
A 21-year-old woman was referred to our glaucoma tertiary center in January 2021 for recurrent episodes of blurred vision associated with peaks of ocular hypertension. She had a history of bilateral juvenile glaucoma diagnosed in 2012.She underwent bilateral trabeculectomy with mitomycin in 2012. Best corrected visual acuity (BCVA) was 20/20 in her right eye (RE) and was limited to light perception in her left eye (LE). She had no history of high blood pressure. Her treatment included topical bimatoprost and timolol in fixed association. Her usual right and left intraocular pressures (IOP)were around 20 mm Hg with a central corneal thickness of 600 µm in both eyes. The cup/disc ratio was 0.8 in the RE and 1.0 in the LE. Prior to her referral to our department, she had consulted in an Emergency Ophthalmologic Department in November 2020 for intermittent episodes of blurred vision and pain in her RE. IOP was 25 mm Hg. Slit lamp examination had revealed the presence of anterior chamber cells. A diagnosis of anterior uveitis was made, and she was treated with topical dexamethasone. One week later, IOP in her RE had lowered to 20 mm Hg. In January 2021, she still complained of recurrent episodes of blurred vision and pain in her RE, and consulted in our glaucoma center. BCVA of the RE was 20/20. IOP was 23 mm Hg. Slit-lamp examination was initially normal. After few minutes, hematic cells in the anterior chamber suddenly appeared, originating from the upper trabeculum, and quickly settling into a hyphema. The filtration bleb remained wellshaped. Gonioscopy of the scleral ostium revealed a dilated scleral vessel bridging across the scleral wound (Figure 1) and actively leaking hematic cells. Based on this observation, we attributed her recurrent ocular hypertension peaks and blurred vision episodes to a Swan syndrome. The causal neovessel in the scleral ostium was cauterized by three spots of focal argon laser (size 50 µm, power 300 mW). Follow-up at 1wk, 1 and 3mo showed no recurrence of hematic cells in the anterior chamber, and the patient had no other episodes of blurred vision or pain. At 3mo follow up, IOP in the RE was 14 mm Hg and gonioscopic examination showed a cauterized vessel in the scleral ostium (Figure 2).
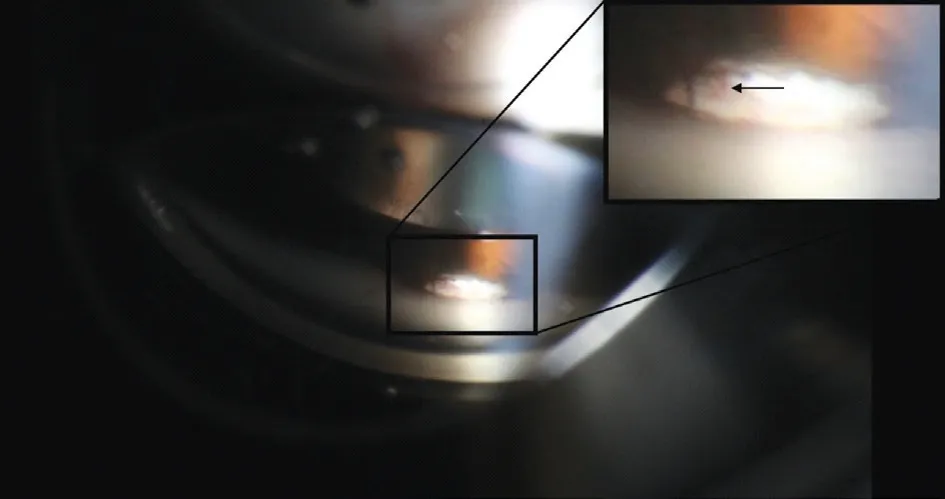
Figure 1 Gonioscopic view of the causal vessel in the scleral ostium before laser treatment (black arrow).
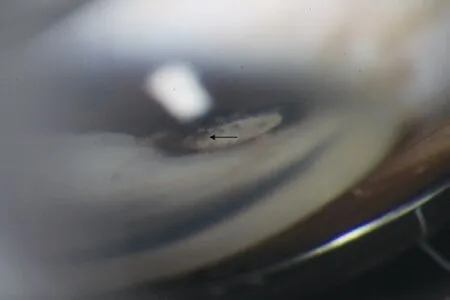
Figure 2 Gonioscopic view of the cauterized vessel in the scleral ostium after laser treatment (black arrow).
This unusual case of recurrent anterior chamber bleeding was caused by a scleral vessel bridging across the filtering ostium.This has been previously described as Swan syndrome[1].Past episodes were initially attributed to anterior uveitis, but the anterior chamber cells observed at that time were most likely red blood cells, which can be hard to differentiate from inflammatory cells in the absence of hypopyon or settled hyphema. The first examination in November 2020 was most likely performed after several hours of bleeding, and no active leak was noted. Upon examination in our center, red blood cells suddenly erupted from the upper iridocorneal angle,which would be very unusual for inflammatory cells. The gonioscopic view confirmed the scleral ostium origin of those red blood cells. The initial effectiveness of topical steroid treatment may seem in favor of the anterior uveitis diagnosis.However, as the bleeding was transient, hematic cells and symptoms would have disappeared without any treatment.Bleeding was responsible for ocular hypertension, as hematic cells can obstruct the trabeculum meshwork and induce an IOP peak (25 mm Hg in our case) and ocular pain. If bleeding is frequent, it can lead to poor control of IOP (20 mm Hg).By cauterizing the causal vessel and stopping the bleeding,hematic cells gradually stopped obstructing the trabeculum meshwork, allowing better IOP control (14 mm Hg).
In confirmed case of uveitis, a general workup is performed,and the standard treatment includes topical steroids even in the absence of obvious etiology[2]. In cases of hyphema, an etiology must be sought. Causes of bleeding include neovascular glaucoma, traumatism, or mispositioned minimally invasive glaucoma surgeries (MIGS) devices[3-4]. Gonioscopy is key in identifying the source of bleeding. There are very few reports of recurrent anterior chamber bleeding after ocular surgery. It was reported by Swan in 1973 after uncomplicated cataract surgery[5-6]. The suspected cause was a neovascularization coming from an ingrowth of episcleral vessels through the cataract scleral wound. To this day, only one case of Swan syndrome following trabeculectomy has been described in the literature and did not include any illustration[7]. Alniemiet al[1]also reported a case of recurrent hyphema after a combined trabeculectomy and cataract procedure, due to a bridging vessel at the sclerostomy margin. In Swan syndrome, the origin of the leaking vessel is thought to be the superficial episcleral plexus[5]. In post-cataract surgery cases, Jarstad and Hardwig[8]described abnormal neovascularization of the cataract incision,attributed to poor wound apposition[5]. In all reported cases,symptoms began at least 5y after surgery. The mechanism leading to neovascularization may imply chronic ischemia of the sclerostomy margin or the cataract scleral wound.Indeed, no neovascularization are observed after clear corneal incisions[9], as avascular properties of the cornea most probably prevent this complication. Concerning the management of Swan syndrome, focal argon laser to cauterize the causative bleeding vessel appears to be the safest and least invasive treatment[9]. Recurrence of bleeding after laser procedures has been reported[5]. Cryopexy, surgical excision of the blood vessels or limbal sutures have also been described[5-6,10].
The originality of our case is that the symptomatic anterior chamber bleeding occurred after a stand-alone trabeculectomy procedure. There was no history of trauma, and examination revealed no rubeosis iridis and no sign of retinal vein occlusion. The bleeding suddenly occurred during the eye exam, probably triggered by sudden IOP increase from gonioscopy, highlighting its paroxystic nature. The recurrent episodes may be explained by general factors, such as arterial hypertension peaks, intensive efforts, or repeated forward bending. Repeated elevations of IOP, in patients having an otherwise effective filtering surgery, must be investigated as they can lead to permanent optic nerve damage and quality of life alteration. Recurrent hyphema can induce IOP elevation,and in most circumstances gonioscopic examination is helpful to identify the source of bleeding. In some cases, it can originate from neovessels bridging across the sclerostomy,also known as Swan syndrome. Recurrences can be prevented,and IOP durably controlled by a safe and fast treatment of the causal wound vessel using focal argon laser.
ACKNOWLEDGEMENTS
Conflicts of Interest:Leroux P, None; Rezkallah A, None;Kodjikian L, None; Loria O, None; Mathis T, None; Denis P, None.
 International Journal of Ophthalmology2021年10期
International Journal of Ophthalmology2021年10期
- International Journal of Ophthalmology的其它文章
- Exosomal miR-29b found in aqueous humour mediates calcium signaling in diabetic patients with cataract
- Intraluminal stenting versus external ligation of Ahmed glaucoma valve in prevention of postoperative hypotony
- Visual acuity after intravitreal ranibizumab with and without laser therapy in the treatment of macular edema due to branch retinal vein occlusion: a 12-month retrospective analysis
- Dexamethasone intravitreal implant (Ozurdex) in diabetic macular edema: real-world data versus clinical trials outcomes
- Comparative analysis of the clinical outcomes between wavefront-guided and conventional femtosecond LASlK in myopia and myopia astigmatism
- Reliability of the ocular trauma score for the predictability of traumatic and post-traumatic retinal detachment after open globe injury
