Air tamponade with inverted internal limiting membrane flap technique for macular hole retinal detachment in high myopia with posterior staphyloma
Hai-Cheng She, Yue Qi, Zi-Bing Jin2, Ning-Li Wang2, An-Li Duan
1Beijing Tongren Eye Center; Beijing Tongren Hospital, Capital Medical University; Beijing Ophthalmology and Visual Science Key Lab, Beijing 100730, China 2Beijing Institute of Ophthalmology; Beijing Tongren Eye Center; Beijing Tongren Hospital, Capital Medical University; Beijing Ophthalmology and Visual Science Key Lab, Beijing 100730, China
Abstract
INTRODUCTION
Currently, vitrectomy with internal limiting membrane(ILM)peeling and silicone oil tamponade is widely used for treatment of macular hole retinal detachment(MHRD).A line of studies have demonstrated that vitrectomy with ILM pealing has a good result in terms of retinal reattachment rate[1-5],while the post-operative best-corrected visual acuity(BCVA)and the macular hole(MH)closure rate remain not satisfactory[4,6].Alternatively, inverted ILM flap technique has been reported to treat refractory MH successfully[7-9].Several pilot studies also have used this technique in MHRD[10-14].It has been reported that compared with the ILM peeling technique, inverted ILM flap technique improved the anatomic and functional outcomes of MHRD in high myopic eyes[11-16].The traditional choices of intraocular tamponades for myopic MHRD usually include silicone oil and gas, such as C3F8or SF6.Silicone oil and gases have improved the success rate of complicated retinal detachment.Air tamponade has been reported to have similar effect for idiopathic MH and simple rhegmatogenous retinal detachment comparing to gases[17-18],while there has been no report using air for MHRD yet.Laietal[10]has reported using ILM repositioning, autologous blood and C3F8temponade for MHRD.The ILM stuffed in the MH and blood clot were considered to keep the MH closed.In China, we have experienced a 3a period without commercially available gases for vitreous tamponade, prompting us to test air tamponade for the surgical treatment of MHRD in patients with high myopia.
In this study, we have used pars plana vitrectomy(PPV)with inverted ILM flap, autologous blood transplantation and air tamponade to treat MHRD in high myopia, and evaluated the efficacy and safety of this method, providing a new insight for development of more efficient surgical approach targeting MHRD.
SUBJECTS AND METHODS
SubjectsThis restrospective study included consecutive patients who presented with decreased visual acuity due to MHRD in highly myopic eyes and underwent vitrectomy from September 2018 to August 2019 at the retina service of Beijing Tongren Hospital.The Medical Ethics Committee of Beijing Tongren Hospital approved the study protocol, which is in accordance with Declaration of Helsinki.All patients signed the informed concents before surgery.The inclusion criteria were: 1)MH retinal detachment; 2)Eye axis more than 26mm; 3)Posterior staphyloma; 4)Follow up for at least 6mo.Patients with MH and retinal detachment but who were not high myopic were excluded.
SurgicalTechniquesA standard, 23-gauge PPV was performed.All the surgeries were performed by the same experienced surgeon under local or general anesthesia.A standard cataract surgery was performed first if necessary.After core vitrectomy, 0.1-0.2 mL of triamcinolone acetonide(TA)was used to visualize the vitreous.Posterior hyaloid membrane was removed from the macular surface with aspiration with the vitrector or forceps.
After peripheral vitrectomy was performed, ILM was visualized by indocyanine green(ICG), and if an epiretinal membrane(ERM)was present, it was peeled.The ILM was peeled off approximately 1-1.5 disc diameters(DD)in a circular fashion around the MH, while the fastest portion of the ILM flap was left attached to the edge of MH.The ILM flap was trimmed to a little bit bigger than the MH with vitrector and inverted to cover the MH when the diameter of the MH is smaller than 1/4 of one DD.Or, when the diameter of the MH is equal to or bigger than 1/4 DD, ILM was trimmed except about 2/3-3/4 of a circle of a small amount of it was inverted toward the center of the MH.The second method was similar with ILM stuffing, only that no pressure was put on retinal pigment epithelium(RPE).The ILM inverting process were aimed to use ILM to cover the whole MH while no redundant ILM was stuffed.Then, a small amount of venous blood was placed on the inverted flap to stabilize it.
The subretinal fluid was drained through an intentional retinal hole while retinal detachment was far more exceeded the retinal arch, or not drained while retinal detachment was limited at the posterior pole.Fluid-gas exchange was carried out with air tamponade in the vitreous cavity.After surgery, the patients were asked to keep prone position for about 5-7d when there was still air left in the vitreous cavity.
FollowupBCVA was recorded by decimal method and converted into the logarithm of the minimum angle of resolution(LogMAR).Optical biometry(IOL Master 500, Carl Zeiss; Germany), color fundus photography(Topcon TRC-50; Tokyo, Japan)and retinal optical coherence tomography(OCT)(Stratus OCT, Carl Zeiss; USA, or Optovue, RTVue XR100-2; USA)were performed for each patient before the surgery.MH was confirmed by OCT and fundus examination.Patients were at least followed up at 1wk, 1, 3 and 6mo after the surgery.At each postoperative follow up, BCVA, slit-lamp examination, fundus examination and OCT were performed.
RESULTS
Twenty-four eyes of 24 patients were included in this study.There were 4 males and 20 females.The average age of the patients was 55±7.9 years,ranging from 42-74 years.Preoperatively, there were 22 phakic eyes and 2 pseudophakic eyes.Mean axial length was 29.79±1.79 mm with a range of 27.33-33.68 mm.The mean BCVA(LogMAR)was 1.36±0.40, ranging from 0.52-2.00.All eyes had posterior scleral staphyloma.Twenty-one patients(88%)had different degrees of choroidal atrophy.Three patients(13%)only had tessellated fundus.All eyes had posterior scleral staphyloma.Retinal detachment was extended beyond the retinal vascular arch in 7 eyes(29%).Only one had subretinal band, while in all the remaining eyes, proliferative vitreoretinopathy(PVR)was A or B.
At 1wk after the surgery, 21 eyes(88%)achieved closure of MH, and 16 eyes(67%)had retina reattachment.Thirteen eyes(54%)had both closed MH and reattached retina.Eight eyes(33%)had subretinal fluid with closed MH.Two eyes(8%)had unclosed but smaller MH and reattached retina.No further treatment was performed in these eyes since the retina was reattached.Only one eye(4%)had MH with detached retina.The patient received 16% perfluoropropane(C3F8, 0.5mL)intravitreal injection immediately in other hospital and were asked to keep prone position for additional 1wk.The retina was attached, and MH was closed in this eye at the 6mo follow up.
At 6mo follow up, all eyes achieved anatomical success, that is, either closed MH or retinal reattachment.Twenty-one eyes(88%)had closed MH and 20 eye(83%)had retinal reattachment.Seventeen eyes(71%)had both complete MH closure and retinal reattachment.Three eyes(13%)had unclosed MH with reattached retina, including one eye which had re-opened MH at 1mo follow up.Four eyes(17%)had persistent subretinal fluid with closed MH.Subretinal fluid in eyes with closed MH reduced with longer follow up time.
At 6mo follow up, BCVA(LogMAR)was 0.65±0.34, ranging from 0.15-1.3, which equals to 0.05 to 0.7 decimal method.The BCVA at 6mo follow up had significant improvement comparing to baseline(t=-5.81,P<0.001; Figure 1).An improvement of 2 or more lines of BCVA was achieved in 12 eyes(50.00%).
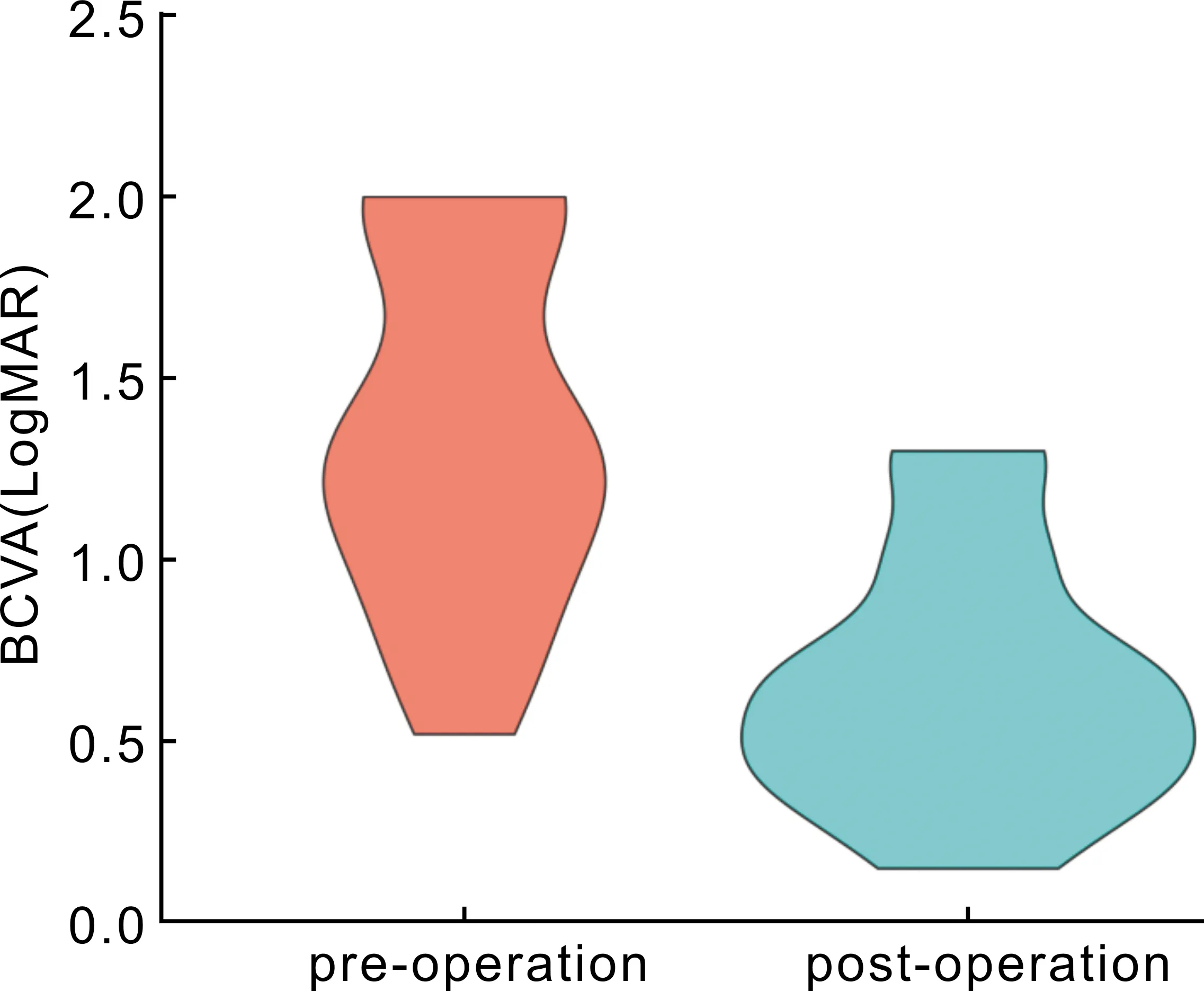
Figure 1 Statistical analyses of BCVA before and 6mo after surgery.
No increased intraocular pressure had been observed during 6mo postoperative follow up.No other serious postoperative complications were observed after surgery.No eyes need a second vitrectomy.
DISCUSSION
In this study, we have reported a retrospective case series of 24 cases of MHRD in myopic eyes treated with PPV combined with inverted ILM, autologous blood transplantation and air tamponade.
To our knowledge,this is the first report that use air as tamponade for MHRD treated with PPV.In the present study, the complete closure rate of MHs is 88% and the complete retinal reattachment rate is 83%.The results are similar to gases and silicone oil tamponade in previous studies of MHRD[1-4,6].In the previous reports, which used inverted ILM flap technique for MHRD, the tamponades were mostly silicone oil or gases[9,11-14,16-17,19].Previous studies have used long-lasting tamponade for myopic MHRD, because it is a concern that the atrophic RPE would barely be able to have enough pump force to keep the neural retina attached.In this study, air tamponade is successfully used after PPV for MHRD probably due to the following reasons.First, the closure of MH is achieved by inverted ILM, not the adhesion between RPE and neural retina.Longer tamponade time might not mean better adhesion.It has been reported by Michalewskaetal[8]that in high myopic MH, with the inverted ILM technique, the closure of the MH began in the inner retinal layers, and the architecture gradually filled with tissue.Blood clot has helped to stable the inverted ILM temporarily before the patient can keep face down position after the surgery; Second, higher surface tension of air or gas may be better than silicone oil to close the MH; Third, we have used TA to visualize posterior vitreous and remove it as much as possible.Theoretically, there is no necessity for longer tamponade, such as silicone oil, to resist the possibility of PVR and traction caused by proliferation membrane.Of cause all the above-mentioned reasons that support air as tamponade for MHRD would not obstruct gas, such as SF6, C2F6or C3F8, to achieve similar if not better results as tamponade.We had one case that had unclosed MH with retinal detachment at 1wk post-operation follow up, and the MH was closed successfully by C3F8intra-vitreous injection, we would consider gas tamponade to have better results in terms of MH closure rate.
The inverted ILM flap technique was first reported by Michalewskaetal[8]to treat MHs with a diameter greater than 400 μm.It has been indicated that inverted ILM technique can improve the closure rate of MH and increase postoperative visual function.With the increase of clinical cases, this technique has been gradually applied in the treatment of myopic MH[20]and MHRD to improve the closure rate of MH[5,7-9,11-15].MH closure rate has ranged from 75%-100% with the inverted ILM flap technique plus vitrectomy, while it has ranged from 25%-89% with just ILM peeling plus vitrectomy in MHRD patients[5,8-9,19].Some studies have shown that by using the inverted ILM flap technique, postoperative BCVA has also been significantly better than using traditional ILM peeling technique[16,21].All of these indicate that inverted ILM flap technique is a good choice for the treatment of MHRD.
In our study, different ILM inverting techniques were chosen according to the size of MH.When the ILM flap is much bigger than the MH, the flap might have tendency to roll and be hard to be flattened.If the flap is not big enough, it could not cover the whole MH.These all may lead to the failure of the operation.The inverted ILM technique has been first reported by Michalewskaetal[8].It involved peeling the ILM in a circular fashion and trimming ILM with a vitreous cutter until only a remnant of it was left around the MH.Then forceps were used to massage and inverted the ILM from all sides to cover the MH.In our case series, for those with a MH lager than 1/4 DD, this method had been used.Others have reported ILM inverting technique using an ILM flap of 1-1.5 diameter of the MH[7,12].For smaller MH, that is, less than 1/4 DD, we have used the latter method.The trimmed ILM is similar with or just a little bit bigger than the MH and we only used this method in small MH so that the inverted flap is small, and it has less chance to roll during the procedure.The purpose of using different method to invert ILM, is to make sure that there is enough ILM to cover the MH while no redundant ILM stuffed in it.It is believed that after ILM is inverted to cover a MH, glial cell migrated to fill in the space and help the recovery of the morphology of the macula[7].
All MHs were covered with patients’ own blood after ILM was inverted.After general anesthesia, patients were always asked to stay in supine position for several hours, which might lead to liquid accumulation at the posterior pole and cause the ILM flap to float away.In this study, the complete closure rate of MHs was 88%.BCVA was significantly better after surgery than at baseline.An improvement in BCVA by 2 or more lines was achieved in 50% eyes.Autologous blood clot might have contributed to the comparatively good result by temporarily fixing the inverted ILM to the expected position.
In this study,88% MHs could be healed in 1wk.While the recovery of visual function was slow.Visual function recovery was not satisfactory at early period after surgery.At 6mo after surgery, visual function had improved significantly.The change of visual acuity is related to the gradual absorption of subretinal fluid.With the decrease of subretinal fluid, the visual acuity of patients gradually improved.This indicated that PPV plus ILM invert and air tamponade could preserve the retinal function and improve the long-term prognosis.
The biggest limitation of the current study is lack of control groups.PPV combined with ILM pealing are comparatively widely accepted surgical steps to treat MHRD.While autologous blood and air tamponade are steps that are reasonable but need to be proven effective by control groups.Given the nature of MHRD, it is hard to include too many patients.Comparing to other literatures reporting PPV for MHRD, the number of cases included in our study is acceptable.A prospective randomized control study is indicated in the future to draw more definitive conclusion.
In conclusion, MHRD in highly myopic eyes can be successfully treated by PPV plus ILM flap,autologous blood and air tamponade.Further prospective clinical studies may be necessary to address the key question whether these procedures are the best choice for MHRD.