Roles of fermented plant-, dairy- and meat-based foods in the modulation of allergic responses
Muhama Haf iz A Rahim*, Nur Hazlin Hazrin-Chong, Hanis Hazeera Harith,Wan A Al Qar Ima Wan-Mohtar, Rashiah Sukore
a Faculty of Food Science and Technology, Universiti Putra Malaysia, 43400 Serdang, Selangor, Malaysia
b Department of Biological Sciences and Biotechnology, Faculty of Science and Technology, Universiti Kebangsaan Malaysia, 43600 Bangi, Selangor, Malaysia
c Faculty of Medicine and Health Sciences, Universiti Putra Malaysia, 43400 Serdang, Selangor, Malaysia
d Functional Omics and Bioprocess Development Laboratory, Institute of Biological Sciences, Faculty of Science, Universiti Malaya, 50603 Kuala Lumpur, Malaysia
e Laboratory of Food Safety and Food Integrity, Institute of Tropical Agriculture and Food Security, Universiti Putra Malaysia, 43400 Serdang, Selangor, Malaysia
Keywords:Allergy Fermented food Milk-based allergens Plant-based allergens Animal-based allergens
A B S T R A C T This review attempts to delineate the effects and roles of fermented foods on allergic responses (AR),specif ically from milk, plant, and meat sources. Evidence for AR alleviation and aggravation were noted for many different fermented food groups. Positive outcomes on AR through fermented foods could be linked to microbial hydrolysis of food allergens, improvement in gut microbiota robustness, and modulation of the immune system that promotes a balance between T helper 1 (Th1) and Th2 cells. Studies on plant-based,non-protein rich fermented foods tend to show more favourable results compared to those on meat-based or protein-rich group. The usage of specif ic and known starter cultures are helpful in alleviating AR, as in the case for many yogurt, Kef ir or Dahi products. Suff icient fermentation time was also deemed important,exemplif ied in studies that showed ineff icient AR reduction through consumption of fresh cheese. However,formation of new allergens through fermentation of certain meat-based foods, or by using specif ic fermenting microbes (e.g. Penicillium sp.), is possible. Thus, combination of starter cultures and food substrates must be considered in preventing or eliminating AR from intake of these foods. This review may aid consumers to make informed decision during the consumption of fermented food.
1. Introduction
Fermented foods are physiochemically-altered foods resulting from microbial activities performed in a regulated environment.Through fermentation, health-promoting properties otherwise inaccessible in the original (unfermented) state of some foods are improved. Beneficial properties of fermented foods include an increase in nutritional bioavailability, safety, sensory quality, and nutrients, and a decrease in the production of harmful substances like antinutrients and toxins [1]. In recent years, fermented foods have risen in popularity partly due to substantial global marketing of the foods’ health benefits and perceived naturalness [2]. For instance,there is an increase in demand for kombucha, a type of fermented tea inoculated with bacterial and yeast biofilms known as SCOBY(Symbiotic Culture of Bacteria and Yeast) [3]. This biological activity leads to kombucha’s improved antimicrobial, antioxidant, antiinflammatory, anticarcinogenic, and antidiabetic properties that are not usually present in unfermented teas [4].
The consumption of fermented foods has been shown to confer various health benefits, owing to the activities performed by fermenting microorganisms, including probiotics. Note that although all fermented foods contain fermenting microorganisms (either viable or non-viable when consumed), not all fermented foods contain probiotics. The term ‘probiotics’ in foods refers explicitly to live and characterized microbial strains, which are added in known quantities and approved of their safety and efficacy. Various health benefits have been associated with microorganisms found in fermented foods in humans, including regulating and supporting the immune system and metabolic activities, maintaining organ fitness, and even improving mental health [5-7]. The gut microbiome can affect the functioning of our nervous, immune and hormonal systems—also commonly known as the ‘microbiota-gut-brain axis’ [8]. Changes in the gut microbiome composition are induced as the microbes convert food components into beneficial substances or metabolites. These molecules can be in the form of short-chain fatty acids (SCFAs), biogenic amines(e.g. histamine), or amino-acid-derived metabolites (e.g. gammaaminobutyric acid) that modulate various systems in the human body, including neurotransmission and immunity [9,10]. In addition,certain fungi (e.g.Aspergillusspp.) can convert food substrates into prebiotics (e.g. oligosaccharides) that promote the growth of beneficial microorganisms [11], or produce pharmaceutically essential compounds such as statins [12]. Further, vitamin B12was found in vegetables and legumes fermented by lactic acid bacteria (LAB) and propionic acid-synthesizing bacteria that are otherwise very limited in unfermented produce [13].
A key health-benefiting aspect of fermented foods through probiotic or fermenting microbial actions is their ability to reduce and/or inhibit allergic responses (AR). AR is defined as the adverse mechanism by a person’s immune system to remove allergens from the body. Allergens are often composed of proteins and are inert,but are recognized as antigens or ‘invaders’ by the immune system.This recognition causes an imbalance of T cells subtypes 1 and 2(Th1/Th2 switch), resulting in the release of Th2-pro interleukin (IL),chemokines, and antibodies such as IgE antibodies by B cells. These compounds then aggravate AR by stimulating other immune cells (e.g.mast cells and other granulocytes), which altogether ‘attack’ the allergen and causes AR symptoms (e.g. dermatitis, rhinitis, asthma, eczema) to manifest [14-16]. Since probiotics found in fermented foods are linked to immunomodulation through microbiota-gut-brain axis signalling, it is hypothesized that consumption of such foods could alleviate AR, likely by immunomodulation and improvement of barrier function [17].
Nevertheless, there are cases where the intake of certain fermented foods, particularly those originating from animals, could aggravate AR. This complication might be due to the production of new allergens by microbes during food fermentation (via the creation of new epitopes by proteolytic enzymes) or components present on the microbes themselves. This negative evidence of fermented foods consumption against AR suggests that not all fermented foods work in favor of eliminating AR. Thus, this review aims to delineate varieties of fermented foods and their role(s) in AR across different models(human, animals, cell lines) and systems (in vivo,in vitro) reported in the literature. The review will focus on 3 major food categories,i.e. milk-, plant- and animal-based (specifically meat) fermented foods. Indeed, our evaluation shows that fermented foods across the 3 categories have diverse AR outcomes (Fig. 1). Overall, fermented foods from one type may be more effective in mitigating AR than another.

Fig. 1 The AR based on different fermented food types. Different line colours denominate different allergic outcomes of fermented food.
2. Milk-based fermented products and their relationship with AR
2.1 Fermented milk
One of the most important classes of food in allergy studies is milk and milk-based products. Cow’s milk, among others (e.g. sheep,goats, and buffalo), is the most prevalent cause of AR in infants and children. Allergic individuals perceive some milk compounds(e.g. caseins,β-lactoglobulin,α-lactalbumin, serum albumin,immunoglobulins) as allergens in their body which signal their immune system to overreact. This reaction thus elicits symptoms ranging from mild reactions like wheezing, itching, coughing to more severe outcomes, including mouth swelling and anaphylaxis [18].However, some AR to milk (e.g. diarrhea, bloating, nausea, abdominal cramps) can be confused with reactions due to lactose intolerance [19].Nevertheless, it is important to note that certain microorganisms in fermented milk can minimize lactose or other non-tolerated milk components through enzymatic digestion.
Previous studies showed that fermented milk products confer varying degrees of AR (Table 1). Approximately half of the studies reported unclear AR to fermented milk, thus require further investigation. Another half of the studies generally reported AR reduction with fermented milk consumption, while a few studies reported AR aggravation. Intake of fermented milk supplemented with probiotics and/or prebiotics has been shown to improve allergic conditions in human infants by modulating the gut microbiota and immune system [20]. This outcome was also seenin vivo,whereby a reduction of AR symptoms was reported in ovalbumin(OVA)-induced mouse models with the intake of probiotic-fermented milk [21,22]. Milk fermentation leads to the production of bioactive compounds that work favorably against AR to milk [23,24]. These compounds, mainly in the form of “encrypted” peptides, are generated through the cleavage of milk proteins such as casein and whey by the LAB proteolytic system [25]. These newly formed peptides have been associated with various health benefits such as antimicrobial,metal-chelating (for increased microelemental nutrient absorption),antioxidant, and immuno-modulating properties. LAB inoculated into milk has also been shown to cleave milk allergens, includingα- andβ-caseins,α-lactalbumin, andβ-lactoglobulin, thereby eliminating or reducing potential AR associated with milk [26].
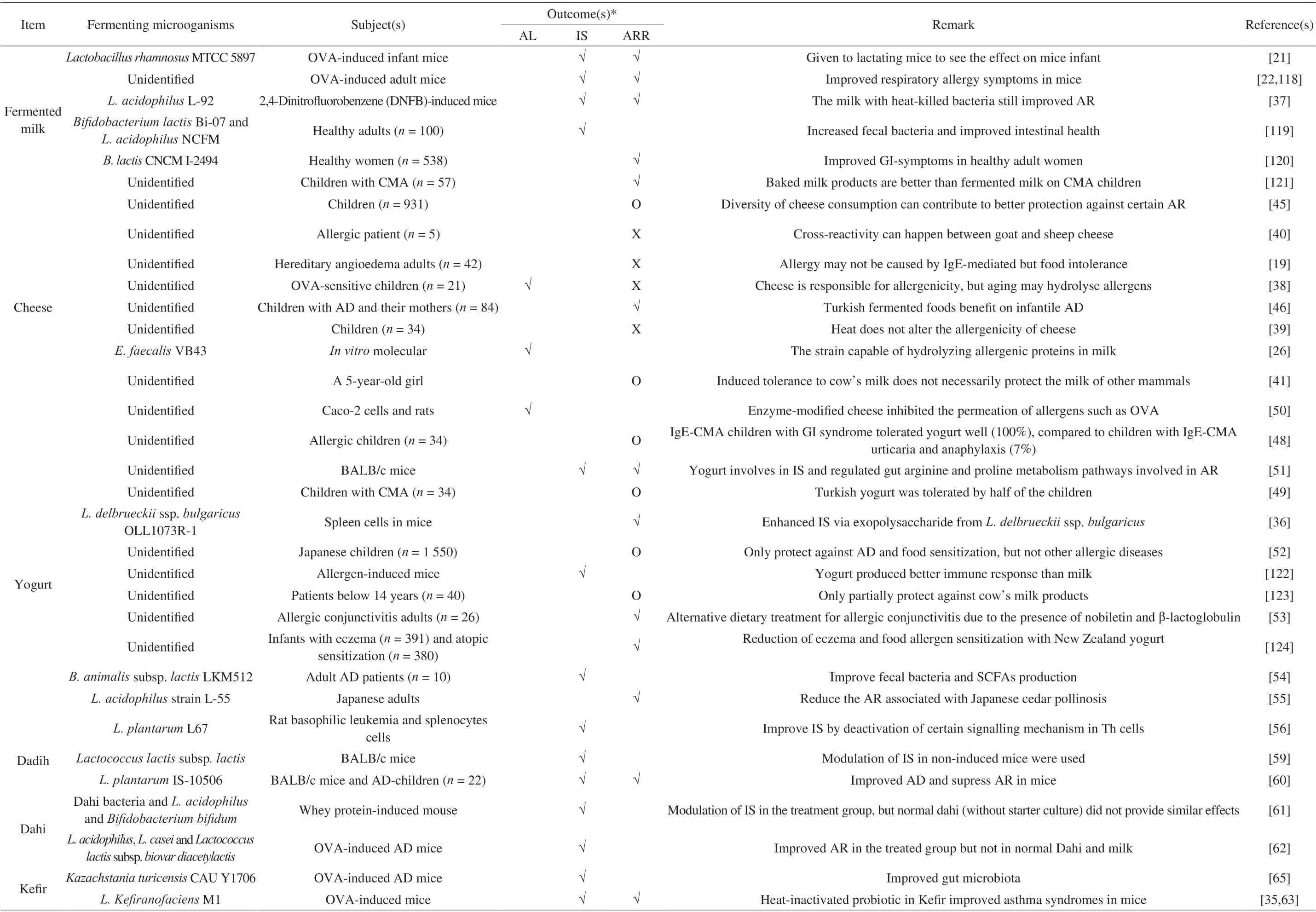
Table 1 The roles of different fermented milks in AR.
Despite the benefits of LAB supplementation in milk against AR,some clinical studies did not observe similar benefits on cow’s milk allergy (CMA) [27], eczema [28] and atopic dermatitis (AD) [29-31],although the severity may be reduced [32-34]. Notably, a common denominator for many of these studies is that probiotics were used without prior fermentation of the milk. This may suggest that fermentation plays a more critical role over probiotic supplementation in lessening AR to milk. van de Heijning et al. [20] concluded that fermented milk is still superior to normal milk in alleviating AR through microbial actions mentioned earlier, even without probiotics administration. This is supported by other studies which reported prevention of AR even when the microorganisms are no longer active(e.g. through heat-inactivation) [35,36] or when the metabolites alone(e.g. exopolysaccharides) are present [37].
2.2 Cheese
Similar to fermented milk, studies on cheese consumption and AR demonstrated mixed results. Previous reports indicated that certain types of cheese, i.e. semi-hard Grana Padano [38], baked cheese [39],goat’s cheese [40], and sheep’s milk ricotta cheese [41] did not reduce milk allergenicity. Even extensively heated (i.e. baked) cow’s milkderived cheese still retained the cheese allergenicity despite showing reduced AR to some extent [39]. Multiple evidences showed that allergy to goat and sheep’s milk cheese is prevalent despite having tolerance to cow’s milk [40-43]. This observation suggests differences in the immunoreactivity of allergens in milk (e.g. caseins) across different species despite evidence of cross-reactivity occurring within the same protein group [44].
Conversely, other studies have reported more positive outcomes with cheese consumption and AR. For example, in a large-scale study involving 931 participants in European countries, it was found that early childhood intake of certain cheeses (hard-pressed, semi-pressed,soft, blue, fresh cheese, and cheese from the farm) protects against AD and food allergy (FA) in their first 6 years of life [45]. Interestingly,the study concluded that subjects who consumed diverse types of cheese are better protected against these AR symptoms. Similar conclusions were made by Celik et al. [46], where consumption of various fermented foods (including cheese) during pregnancy can help reduce the risk of AD in their infants, compared to consumption of only one type of fermented food. This may be attributed to the diversity of fermenting microorganisms which increased the robustness of the gut microbiome via ‘functional redundancy’. The term‘functional redundancy’ refers to different species of microorganisms sharing the same function (e.g. casein hydrolysis), thus allowing metabolism of food components and important metabolite production to persist in the gut even when the growth or activity of a particular working microbial group is diminished.
Another notable aspect of cheese that is linked to AR reduction is cheese maturation. The aging of cheese has been reported to reduce allergenicity in both adults and children compared to fresh cheese [26,38,47]. More extended periods of cheese fermentation before consumption allow fermenting microorganisms to grow and hydrolyze potential allergens in cheese. Further, inoculating cheese with specific allergen-metabolizing microorganisms, e.g.Enterococcus faecalisVB43 [26] from LAB, may drive allergen degradation more rapidly. Thus, even though cheese, in general, has been associated with aggravation of AR, certain aspects, including cheese diversity and prolonged cheese fermentation, may increase its tolerability by sensitive individuals.
2.3 Yogurt
While there is mixed evidence for cheese, evidence on yogurt suggests more positive effects in alleviating AR. In the early 2000s,yogurt was shown to reduce allergic symptoms by lowering the production of IgE, Th2-associated mediators, and modulating the immune responses [14]. Apart from being very well-tolerated, (i.e. not likely to cause an AR) [48,49], yogurt was shown to reduce existing AR such as CMA and gastrointestinal (GI) symptoms [48] and inhibit permeation of allergens in Caco-2 cells and rats [50]. Other observable AR reductions by yogurt includes eliminating shrimp tropomyosin-induced intestinal mucosal disorders [51], preventing the development of infancy AD and food sensitization [52], and reducing allergic conjunctivitis [53]. As yogurt production can be readily controlled using an appropriate starter culture, this offers an advantage over the production of cheeses that sometimes adopt spontaneous fermentation. For example, yogurt can be made using a specific strain calledL. delbrueckiissp.bulgaricusOLL1073R-1, which can modulate immunity even when it is heat-killed due to their production of exopolysaccharides [36]. Additionally, in yogurt produced usingB. animalissubsp.lactisLKM512, a similar protective effect was observed [54]. The bacterial strain was shown to regulate the intestinal microflora by producing SCFAs particularly, butyrate,which can induce Th1-type cytokine in adults with intractable AD. The ability to reduce AR was also observed in yogurt using different types of culture starter, such asL. acidophilusL55 [55]andL. plantarumL67[56].
2.4 Minority dairy products
Compared to cheese and yogurt, there is limited studies that relate “minority” dairy products such as Dadih, Dahi, and Kefir.However, evidence indicates that these products offer similar benefits to yogurt, such as the ability to modulate Th1/Th2 and regulatory T cells (Tregs) immune responses, reduce serum IgE, influence the microflora components in the gut and regulate the expression of crucial pathways in AR [57-62]. Again, these studies indicate that the benefits are more prominent in products enriched with the correct type of probiotics, especially in Dahi [61,62]. Interestingly, the benefits from Kefir are not only contributed by LAB [35,63,64], which are dominant fermenting microbes in cheese and milk, but also by yeast such asKazachstania turicensisCAU Y1706 [65]. These findings demonstrate the diversity of microbial species that could be utilized in food fermentation to improve health and wellness.
3. Plant-based fermented foods
Plant-based foods constitute a significant part of “The Big 8”food group, which consists of foods (i.e. milk, eggs, tree nuts, fish,crustacean shellfish, wheat, and soy) that are most commonly linked to AR. Allergens from plant origin are usually comprised of (but are not limited to) peanuts, tree nuts, soy, wheat, rice, and fruits [18].Amongst these, tree nuts and peanuts are not typically fermented,although some variations exist e.g. fermented peanut cake (also known as Oncomin Indonesia). Fermented tree nuts and peanuts are less produced traditionally mainly because they naturally last relatively longer compared to other plant-based foods.
A large diversity of fermented foods from plants are known to cause varying degrees of AR (Table 2). Soybean is the most studied type which is likely due to its popularity in Asia. Like many other fermented food groups, reports on the effect of fermentation on the allergenicity of soybean vary. In some cases, fermentation of soybean or its derivatives with certain LAB strains (e.g.L. brevisCICC 23474,Lactobacillusspp. CICC 23470, andL. helveticus) effectively degrade allergenic proteins [66,67]. In particular,L. brevisCICC 23474 andLactobacillusspp. CICC 23470 were able to reduce immunoreactivity ofβ-conglycinin (Gly m 5) and the acidic subunit of glycinin (Gly m 6)in vitro[66]. Both glycinin andβ-conglycinin constitute a major fraction (65%-80%) in soy protein that have been strongly linked to AR induction [18]. The two LAB strains that reduced these soy protein components were also shown to ameliorate ARin vivoby reducing Th2-related inflammatory responses [66]. Several other studies also indicated the role of bacterial actions in alleviating AR in soybean by either cleaving the allergen through proteolysis (e.g. using protease or peptidase) [18,68] or directly regulating the intracellular signalling pathways, such as phosphorylation of nuclear factor kappa B and mitogen-activated protein kinase (MAPK) [69].
In addition, tempeh fermentation by fungiRhizopus oligosporusandActinomucor elegansshowed a reduction of immunoreactivity through the hydrolysis of glycinin,β-conglycinin, and several other antinutrient components [70]. However, certain fungal species (e.g.Rhizopus oryzaeandSaccharomyces cerevisae) failed to produce similar positive effects in alleviating AR from soy protein isolate.This observation was compared to that of a LAB species(L. helveticus), which could reduce the immunoreactivity of the isolate protein fractions completely [67]. These results may indicate a bigger role played by bacteria than fungi in alleviating AR through soybean fermentation. However, since positive outcomes using fungi have been reported, more studies are necessary to decipher fungi’s role and capacity in alleviating soybean-related AR.
Although fermented soybean is generally linked to favorable outcomes against AR, a Japanese delicacy, natto, exhibits less promising results. The benefits of natto intake by pregnant mothers have been reported to lower eczema incidences in their offspring [71].However, consumption of natto by hypersensitive Japanese may result in late-onset anaphylaxis and an increase in allergic markers [72-74].The formation of poly-γ-glutamic acid allergen likely causes these effects during natto fermentation [75]. Theoretically, poly-γglutamic acid can be cleaved by an enzymeγ-glutamyl hydrolase,which can be produced byBacillusspecies [7]. Thus, it may be helpful to specifically apply fermenting strains such as those fromBacillussp. that are known to metabolize foods that are likely to cause allergic reactions.
Some reports highlight the risk of consuming soy sauce [76], such as the development of lip irritation in patients of varying ages [77].The leading cause of this AR stimulation is unclear, as the subjects’histamine and serum IgE demonstrated little change before and after consumption of soy sauce. It is suspected that certain new substances derived from soy sauce fermentation might have triggered the AR. As soy sauce is typically produced from fungi such asAspergillus oryzae,the allergens in the soy sauce might not be hydrolyzed as effectively as bacterial fermentation [67,78]. Many other studies showed reduced allergenicity of soybean through soy sauce fermentation [79-82].However, the evidence are still not quite conclusive as most of the studies are quite outdated (before 2010) from the same group of researchers.
Apart from fermented soybean, another equally popular plantbased fermented foods are fermented vegetables. A typical example is kimchi, a fermented cabbage known to be part of Korean staple foods. Generally, kimchi consumption has been linked to the reduction of AR and AR-related factors. These effects are achieved by modulating immune systems and enhancing the gut and microflora functions [83-86]. More specifically, LAB isolates from kimchi such asEnterococcus faeciumFC-K andL. plantarumhave been shown to alleviate IgE production by promoting Th1 immune response and suppressing B cell activation [87]. In addition, a study demonstrated thatL. plantarumalso alleviates AR mainly by downregulating the production of cytokine that mediate Th2 immune responses,particularly cytokines that promote the activity of immune cells known to be involved in allergic diseases such as eosinophils and mast cells [88]. Sauerkraut is another cabbage-based fermented food which is fermented under different salinity and temperature. The relationship between sauerkraut and AR has not been widely studied, however, a study claimed that AR associated with sauerkraut consumption might be due to large quantities of biogenic amines, including tyrosine and histamines, generated during sauerkraut production [89]. More studies are necessary to confirm this assumption.
Most studies focusing on fermented vegetables mainly focused on the therapeutic effects of the fruit or plant extract on human rather than alter their allergenicity [90-94]. Several studies have reported positive effects of an assorted range of fermented plant-based foods against AR, mostly through LAB fermenting activities. For example,sourdough (i.e. LAB- or wild yeast-based fermented wheat) may confer a beneficial health effect towards patients with irritable bowel syndrome [95]. The study showed lower allergen markers(α-amylase/trypsin inhibitors (gluten) and FODMAPs) as the wheat fermentation progressed. Nevertheless, the study showed insignificant outcomes when compared to commercial yeast-fermented bread. In contrast, LAB-fermented rice consumed by pediatric patients resulted in significant improvements in their SCORing Atopic Dermatitis(SCORADs) results [96]. In another study, the fermentation of sesame byLentinula edodeswas demonstrated to be effective at reducing the mRNA expression of Th2-associated immune responses in a cellular model of AD [97]. Favorable immunomodulatory effectsin vitrowere also observed when this strain was used in kombucha tea, although the authors noted thatCoriolus versicolormay demonstrate better outcomes [98]. In sword beans (Canavalia gladiata) fermentation,
Kim et al. [99] found that the fermenting fungusA. oryzaecontributed to maintaining the appropriate Th1/Th2 cytokine ratio and promoting anti-inflammatory effects in an AD mouse model.Positive immunomodulation was also shown in fermented grape marc [100] and sake lees [101] in alcohol production. Consumption of LAB-fermented buckwheat sprouts was shown not to elicit AR;accompanied by the increase of nutritional and therapeutic properties during the fermentation [102].
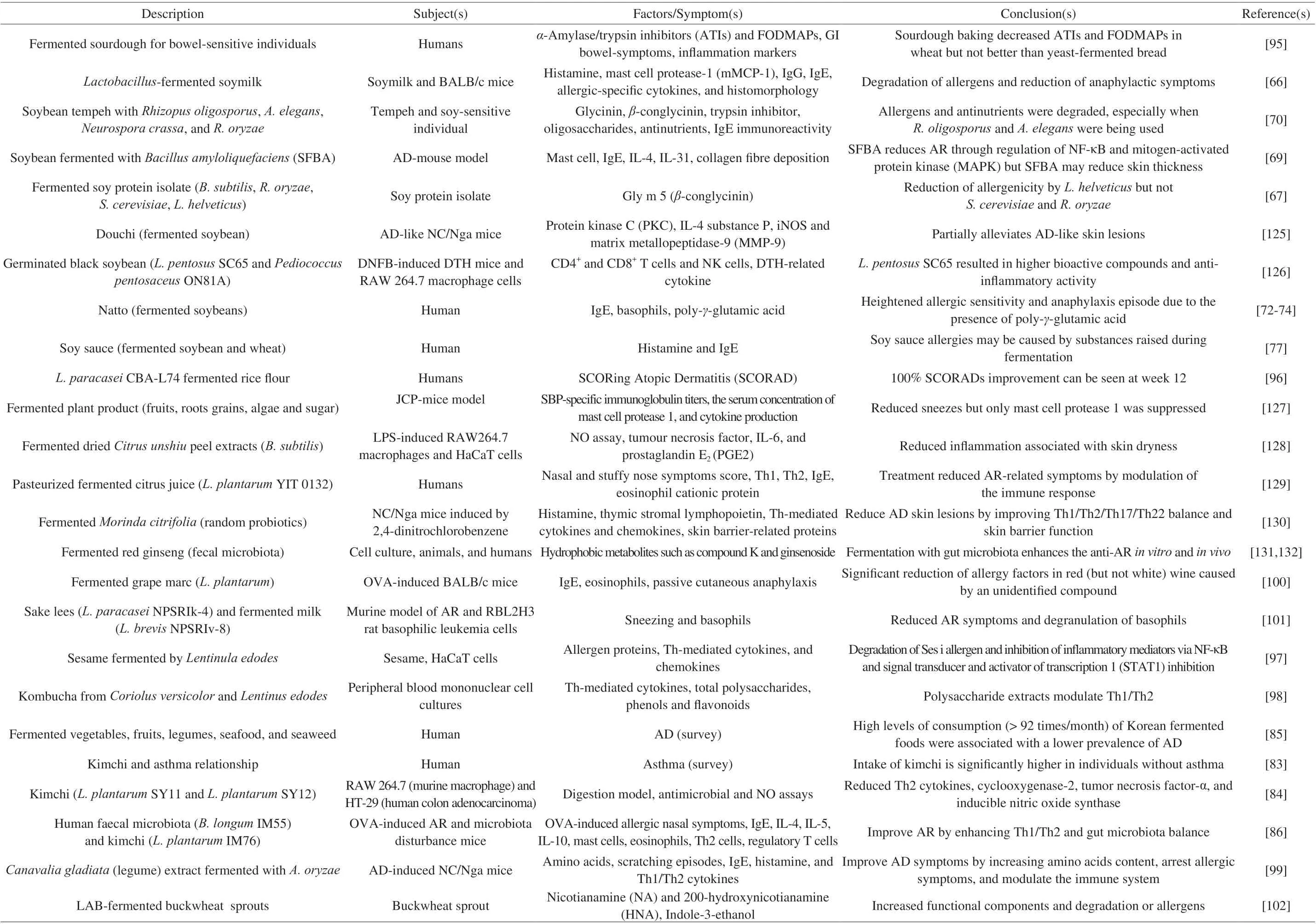
Table 2 A summary of previous literature on the AR of plant-based fermented foods.
4. Meat-based fermented foods
Seafood-based foods, including fish and shellfish are part of the significant protein sources that contribute to AR. Nonetheless, several pieces of evidence indicate the beneficial role of fermentation in reducing the allergenicity of this food group. It was found that certain microorganisms (e.g.L. plantarumandS. cerevisiae) used during fish fermentation or its products (e.g. fish oil) could significantly improve the inflammatory responses by altering the allergen structure, suppressing the activity of immune cells (e.g. helper T cells) and increasing the number of Tregs [103,104]. Further, fish allergenicity was shown to decrease by marinating (i.e. fermenting)the fish compared to direct frying, cooking, and canning [105].The latter processes shorten microbial contact time with the meat,limiting fish allergen degradation via the microbes. Additionally, the fermentation of Saeujeot, a type of Korean fermented shrimp, reduced its allergenicity by decreasing serum binding ability against shrimp tropomyosin in allergic patients [106]. Although positive results in fermented seafood were observed, there are also examples in which seafood fermentation aggravates AR. This adverse reaction was demonstrated by Moon et al. [107] who demonstrated the link between Korean fermented seafood aekjeot (fish sauce) and jeotgal (fish paste) and increased in biogenic amines (histamine and tyramine).However, this observation might be related to specific fermenting communities since fish fermentation by other species, includingTetragenococcus halophilus[108] andBacillus polymyxa[109],could reduce the histamine content instead of elevating it.
Compared to seafood, red meats (i.e. from cows, sheep, lamb etc.)showed a higher contribution to AR based on the current literature [110].There is currently little evidence on the reduction and elimination of meat allergenicity through fermentation; instead, more studies tend to report AR aggravation through fermented/processed meat consumption. A study in Spain, for example, showed a small group of children (n= 3) experiencing allergies after ingesting dry sausages fermented by the fungusPenicillium chrysogenum[111]. Each child was observed to be sensitive to proteins produced by the fungus,indicating that the microorganism itself could also trigger the allergy,apart from several meat constituents like biogenic amines and serum albumin [111,112]. Production of new allergens resulting from meat fermentation is also possible, thus further exacerbating AR. Some fermented and processed meats could also contain plant products (e.g.wheat protein) that may partly contribute to AR [113]. Nevertheless,some fermented meat production would utilize LAB as a starter culture, which has been shown to alleviate AR. One such example is from a study that demonstrated a reduction of biogenic amines in sausages fermented by LAB [114]. Fermentation was indicated to be important in meat protein degradation, although its effects on meat protein allergens was not demonstrated [115-117]. It is possible that,by carefully choosing a suitable starter culture, the allergenicity of animal-based products could be reduced through food fermentation.More investigation is necessary to deduce this hypothesis-currently,the number and scope of research on meat-based fermented food are still relatively scarce.
5. Gaps and concluding remarks
Based on this review, several conclusions and recommendations could be made, as follows:
1. A relatively large proportion of studies demonstrated that consuming carbohydrate-rich plant-based fermented foods often leads to a favorable reduction of AR. In contrast, the consumption of fermented protein-rich (including plant-based) foods such as milk,soybean, and animal products and their effects on AR highly depends on the food type and fermenting microorganisms. The discrepancies of fermented foods on AR could be attributed to several factors including the number and type of potential allergens initially found in the food, the capability of fermenting microbes in hydrolyzing or altering the structure of allergenic proteins, and the possibility of new allergens being formed from the fermenting actions by the microbes.
2. While literature on milk-based fermented foods (e.g. cheese,yogurt) production has been relatively extensive, most studies did not identify the specific microorganisms responsible for the fermentation.Thus, comparison between different studies is often limited to the effects of consuming such foods and not expanded to discussing the microbial communities that play a major role in driving these effects.Knowing the identity, abundance and related function of the starter culture microorganisms is useful for reproducibility in future studies,which is key to developing effective starter cultures and probiotics for AR reduction.
3. Many fermented food-based studies have primarily focused on utilizing LAB as the major fermenting microorganisms. Although using this bacterial group has been effective, exploration of the fermenting action of yeast and fungus and their resulting capability in alleviating AR should also be considered. Fungi serve as a vital starter culture in much legume-based and beverage fermentation,and are known to produce beneficial substances, proteases, and immunomodulating properties that remain as important themes in AR studies.
4. More studies are needed to ascertain the effects of fermented foods from lesser-known regions, such as Africa, Southeast Asia, and the Middle East. The variety of fermented food in these regions may contribute to new findings and further insights into the identity and function of the fermenting microbes, and ways the fermented foods could curtail AR in the human population.
Declaration of interest statement
The authors declare no competing interests.
- 食品科学与人类健康(英文)的其它文章
- The role of probiotics in prevention and treatment of food allergy
- The role of gut microbiota and its metabolites short-chain fatty acids in food allergy
- Association of nutrients intake during pregnancy with the risk of allergic disease in offspring: a meta-analysis of prospective cohort studies
- Purif ication and immunoglobulin E epitopes identif ication of low molecular weight glutenin: an allergen in Chinese wheat
- Determination of egg and milk allergen in food products by liquid chromatography-tandem mass spectrometry based on signature peptides and isotope-labeled internal standard
- An antifouling polydopamine-based f luorescent aptasensor for determination of arginine kinase

