孕期血脂指标与妊娠期糖尿病及新生儿脐血C肽的相关性研究
吴佳丽?甘文佳?冯品宁
【摘要】目的 分析妊娠期糖尿病(GDM)孕婦孕期血脂水平的变化情况,探讨孕期血脂水平与GDM及新生儿体重及脐血C肽之间的关系。方法 采用病例对照研究,收集673例孕妇的临床资料,根据其孕中期75 g口服葡萄糖耐量试验(OGTT)结果分为GDM组(150例)、糖耐量正常(NGT)组(523例)。采用Logistic回归分析GDM发生的风险因素。采用Spearman相关性分析GDM孕妇血脂水平与新生儿体重和新生儿脐血C肽之间的相关性。结果 在孕早期阶段,与NGT组相比,GDM组甘油三酯水平更高、脂蛋白a[Lp (a)]水平更低;在孕中期阶段,与NGT组相比,GDM组总胆固醇及HDL-C水平更低;在孕晚期阶段,与NGT组相比,GDM组甘油三酯及载脂蛋白A1/载脂蛋白B
(ApoA1/B)水平更高、ApoB水平更低(P均 < 0.05)。年龄(OR = 1.111,95% CI = 1.065~1.158,P < 0.001)和孕早期Lp(a)(OR = 0.660,95% CI = 0.454~0.960,P =0.030)是GDM发生的独立因素。新生儿出生体重与孕妇年龄呈负相关(rs =?0.253,P=0.013),与产后BMI(rs = 0.241,P = 0.017)、孕期增重(rs = 0.270, P = 0.017)、分娩时胎龄(rs = 0.34,P = 0.001)呈正相关。在孕早期和孕晚期,新生儿出生体重与甘油三酯、ApoB呈正相关,与ApoA1/B呈负相关。新生儿出生体重与孕晚期ApoE呈正相关(rs = 0.227, P = 0.025)。新生儿脐血 C 肽水平与孕中期(rs = ?0.218,P = 0.038)和孕晚期(rs = ?0.227, P = 0.031)的ApoE水平呈负相关。结论 GDM孕妇在妊娠早期就发生脂代谢紊乱。在妊娠期间,监测血脂的变化,维持正常的血脂水平能有效控制妊娠期并发症,减轻不良妊娠结局对母儿的影响。
【关键词】妊娠期糖尿病;孕妇;血糖;血脂;新生儿
Study of the correlation between serum lipid parameters during pregnancy and gestational diabetes mellitus and neonatal cord-blood C-peptide Wu Jiali, Gan Wenjia, Feng Pinning. Medical Laboratory Department, the First Affiliated Hospital of Sun Yat-sen University, Guangzhou 510080, China
【Abstract】Objective To analyze the changes of serum lipid levels in pregnant women with gestational diabetes mellitus (GDM) and the relationship between serum lipid levels during pregnancy and GDM, neonatal birth weight and cord-blood C-peptide. Methods In this case-control study, clinical data of 673 pregnant women were collected. According to the results of 75-g oral glucose tolerance test (OGTT) in the second trimester (Tr2), 673 pregnant women were divided into the GDM group (n = 150) and normal glucose tolerance (NGT) group (n = 523). The risk factors of GDM were identified by Logistic regression analysis. The correlation between serum lipid level, neonatal weight and cord-blood C-peptide in GDM pregnant women was analyzed by Spearman correlation. Results During the first trimester (Tr1), triglyceride (TG) level was higher and lipoprotein(a) [Lp(a)] level was lower in the GDM group than those in the NGT group. During Tr2, TC and high-density lipoprotein cholesterol (HDL-C) levels in the GDM group were lower compared with those in the NGT group. In the third trimester (Tr3), TG level and apolipoprotein A1/B (ApoA1/B) ratio were higher and ApoB level was lower in the GDM group than those in the NGT group, with statistical significance (all P < 0.05). Age (OR = 1.111, 95%CI = 1.065-1.158, P < 0.001) and Lp(a) in Tr1 (OR = 0.660, 95%CI = 0.454-0.960, P = 0.030) were the independent factors of the incidence of GDM. Neonatal birth weight was negatively correlated with age (rs = -0.253, P = 0.013), whereas positively correlated with postpartal body mass index (BMI) (rs = 0.241, P = 0.017), gestational weight gain (GWG) (rs =
0.270, P = 0.017) and gestational age at delivery (rs = 0.34, P = 0.001). In Tr1 and Tr3, neonatal birth weight was positively correlated with TG and ApoB levels, whereas negatively correlated with ApoA1/B ratio. Neonatal birth weight was positively correlated with ApoE level in Tr3 (rs = 0.227, P = 0.025). Neonatal cord-blood C-peptide level was negatively correlated with ApoE levels in Tr2 (rs = -0.218, P = 0.038) and Tr3 (rs = -0.227, P = 0.031). Conclusions Pregnant women with GDM develop lipid metabolism disorder in Tr1. During pregnancy, monitoring the changes in blood lipids and maintaining normal blood lipid levels can effectively control the complications during pregnancy and mitigate the effect of adverse pregnancy outcomes on mother and neonate.
【Key words】Gestational diabetes mellitus; Pregnant woman; Glucose; Lipid; Neonate
妊娠期糖尿病(GDM)是指妊娠期間发生的糖代谢异常,是常见的妊娠并发症之一[1]。目前我国GDM的发病率为12.8%~16.7%,呈逐年上升趋势[2]。研究表明GDM是孕妇产后不良妊娠结局的危险因素,同时与胎儿的健康密切相关[3-5]。妊娠期间为满足母体能量储备的需求以及胎儿生长发育的需要,母体脂质代谢会发生复杂变化。妊娠期的高脂血症会导致胰岛素抵抗和GDM的发生与发展。GDM也可诱导与胰岛素抵抗一致的血脂异常状态[6]。本研究通过分析GDM孕妇孕期血脂水平的变化情况,探讨孕期血脂水平与GDM 及新生儿体重及脐血C肽之间的关系。
对象与方法
一、研究对象
选取2018年5月至2019年11月在中山大学附属第一医院进行常规孕检的673例孕妇,根据孕中期75 g 口服葡萄糖耐量试验(OGTT)结果,将研究对象分为GDM组(150例)、糖耐量正常(NGT)组(523例),进行病例对照研究。所有研究对象排除糖尿病合并妊娠、妊娠期高血压疾病、感染性炎症以及肿瘤等疾病。本研究经中山大学附属第一医院伦理委员会批准(批件号:[2022]043),所有研究对象均知情同意。
二、方 法
1. 资料收集
通过查阅病例系统收集研究对象孕前及孕期临床资料和实验室检查结果,包括以下资料:①基线资料,如妊娠年龄、产后体重、孕期增重以及胎龄;②实验室检查结果,包括孕1~13周(孕早期)、孕14~27周(孕中期)及孕≥28周(孕晚期)的血脂指标如甘油三酯、总胆固醇、HDL-C、LDL-C、载脂蛋白 A1(ApoA1)、载脂蛋白 B(ApoB)、载脂蛋白 E(ApoE)、脂蛋白 a[Lp(a)],产后 OGTT 结果如空腹血糖、餐后1 h 血糖和餐后2 h 血糖。
2. 孕期 GDM 诊断标准
以 2022 年美国糖尿病协会(ADA)标准作为 GDM诊断标准,75 g OGTT结果符合空腹血糖≥
5.1 mmol/L,餐后1 h 血糖≥10.0 mmol/L,餐后 2 h
血糖≥8.5 mmol/L这三项中的任意一项,诊断为 GDM。
三、统计学处理
采用 SPSS 26.0 软件进行统计学分析。非正态分布计量资料采用M(P25,P75)表示。非正态分布计量资料两组间比较采用Wilcoxon秩和检验,组内比较采用重复测量设计的方差分析对孕早期、孕中期以及孕晚期的血脂水平进行比较。采用Logistic回归分析确定GDM的相关因素,纳入的变量为孕早期血脂相关指标,根据中位数将自变量分为2组,以变量<中位数组为参照组,将单因素回归有意义(P < 0.01)的变量纳入多因素Logistic回归,采用向前逐步回归法(LR 法)筛选自变量。使用Spearman秩相关分析新生儿出生体重及新生儿脐血C肽水平与孕期糖脂水平的相关性。P < 0.05为差异有统计学意义。
结果
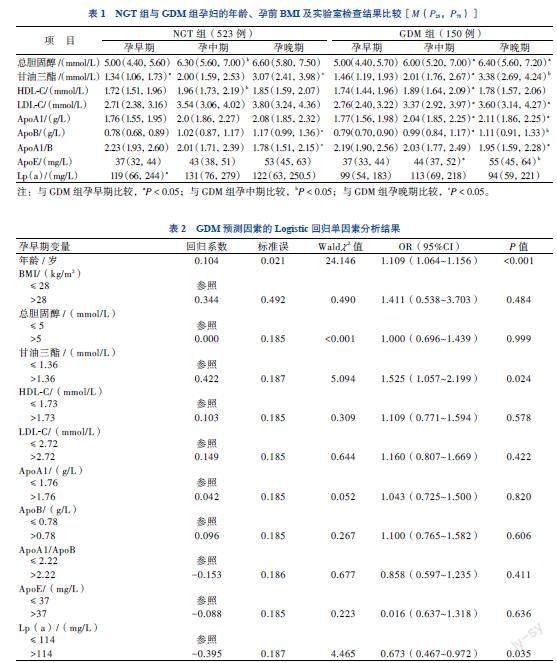
一、NGT组与GDM组孕妇的年龄、孕前BMI及实验室检查结果比较
NGT组孕妇的年龄为32(29,35)岁,孕前BMI为19.86(21.23,23.05)kg/m2;GDM组孕妇的年龄为31(34,37)岁,孕前BMI为20.03(21.62,23.66)kg/m2。2组孕妇的年龄、孕前BMI比较差异均无统计学意义(P均> 0.05)。
在孕早期阶段,与NGT组相比,GDM组甘油三酯水平更高、Lp(a)水平更低;在孕中期阶段,与NGT组相比,GDM组总胆固醇及HDL-C水平更低;在孕晚期阶段,与NGT组相比,GDM组甘油三酯水平更高、ApoB水平更低(P均< 0.05)。在GDM组中,孕中期及孕晚期总胆固醇、LDL-C 及ApoA1水平高于孕早期。甘油三酯、ApoB及ApoE水平在妊娠期间逐步升高。孕晚期ApoA1/B 水平低于孕早期及孕中期(P均< 0.05)。见表1。
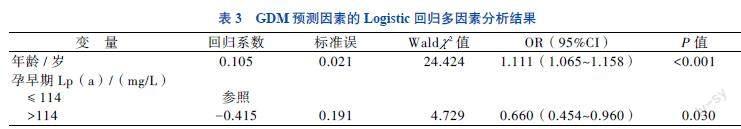
二、GDM 相關因素的Logistic回归分析
单因素分析显示,孕妇年龄、孕早期甘油三酯和Lp(a)水平与GDM相关(P均 < 0.05),见表2。多因素分析显示,孕妇年龄(OR = 1.111,95% CI = 1.065~1.158,P < 0.001)和孕早期Lp(a)(OR = 0.660,95% CI = 0.454~0.960,P = 0.030)均为GDM的独立危险因素。见表3。
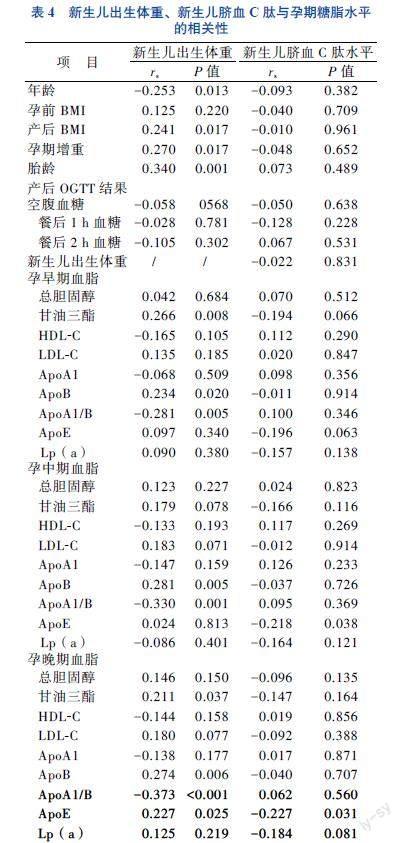
三、GDM 患者血脂水平与新生儿体重和新生儿脐血C肽的相关性分析
在150例GDM孕妇所产的新生儿中,共收集 91例新生儿脐血C肽水平和98例新生儿出生体重。新生儿出生体重与孕妇年龄呈负相关(rs = -0.253,P = 0.013),与产后BMI(rs = 0.241,P = 0.017)、孕期增重(rs = 0.270,P = 0.017)、分娩时胎龄(rs =
0.340,P = 0.001)呈正相关。在孕早期和孕晚期,新生儿出生体重与甘油三酯、ApoB呈正相关,与ApoA1/B呈负相关。新生儿出生体重与孕晚期 ApoE呈正相关 (rs = 0.227,P = 0.025)。新生儿脐血C肽水平与孕中期(rs = -0.218,P = 0.038)和孕晚期(rs = -0.227,P = 0.031)ApoE水平呈负相关。见表 4。
讨论
我国GDM发病率逐年升高,早期诊断可减轻疾病负担。GDM的最佳筛查方案仍然存在争议,美国糖尿病协会建议孕妇在孕24~28周通过OGTT 进行GDM筛查[7-8]。然而,在孕24~28周进行筛查可能太晚,很难预防与GDM相关的一些并发症。对GDM进行更早的筛查可更早地高危人群进行干预,从而降低不良妊娠结局的发生率。
有研究显示。在妊娠15周前进行有效的生活方式干预可降低GDM的发生[9]。胰岛素联合饮食干预后GDM孕妇能更好地控制血糖水平,从而改善妊娠结局[10]。虽然GDM的病因尚不明确,但肥胖及高龄的孕妇已经被认定为高危人群[11]。Todoric 等[12]研究认为,妊娠期Lp(a)水平与GDM无关。本研究显示,年龄和孕早期Lp(a)与GDM的发生相关,且孕早期Lp(a)水平与GDM的发生呈负相关。研究结果的不同可能是由于Lp(a)水平与饮食、活动、基因遗传等因素有关,研究结果还需要更大样本量的多中心研究来验证。GDM 患者发生胰岛素抵抗与胎盘分泌的激素有关,除糖代谢紊乱外,孕妇也会出现血脂异常[13]。母体糖脂代谢异常对胎儿的心血管功能有着不良的影响,导致 GDM 的母亲所生的孩子在成年后更易罹患心血管疾病[6]。本研究显示,与NGT 组相比,在孕早期及孕晚期,GDM组甘油三酯水平更高;而在孕中期,GDM组总胆固醇及 HDL-C 水平更低。结果提示,GDM孕妇在孕早期就已经出现血脂异常,孕中期孕晚期血脂代谢仍然异常,提示监测整个孕期血脂变化是非常必要的。
一项包含565例GDM患者的研究表明,母亲 ApoB 水平和甘油三酯/HDL-C比值可以预测妊娠期间巨大儿的发生[14]。另有研究表明,新生儿随着出生体重的不断增加,母亲受伤、残疾和死亡的风险逐渐增加[15]。母体代谢环境与新生儿生长发育密切相关。研究表明,母体高血糖会影响胎儿胰岛素水平,从而影响胎儿脂肪合成[16]。上述研究提示,孕妇胰岛β细胞功能障碍可能与新生儿肥胖有关。孕妇肥胖与新生儿肥胖密切相关,孕期体重增加影响出生体重和新生儿脂肪量[17-18]。新生儿出生体重肥胖与儿童期BMI相关。Josefson等[16]研究表明,新生儿肥胖和脐血C肽可介导母体葡萄糖和BMI与儿童肥胖的关系。母体环境可影响新生儿发育。本研究观察了妊娠期糖脂代谢与新生儿体重及脐血C肽的关系,结果显示新生儿出生体重与年龄呈负相关,与产后BMI、孕期增重、分娩时胎龄呈正相关。在妊娠早期和晚期,新生儿出生体重与甘油三酯、ApoB呈正相关,与ApoA1/B呈负相关。新生儿脐血C肽水平与ApoE 在孕中期和孕晚期呈负相关。
综上所述,GDM孕妇在整个妊娠期间均存在脂代谢紊乱。在妊娠期间,严密监测血脂的变化,维持正常的血脂水平可能有助控制妊娠期并发症、减轻不良妊娠结局对母儿的影响。
参 考 文 献
[1] Chiefari E, Arcidiacono B, Foti D, et al. Gestational diabetes mellitus: an updated overview. J Endocrinol Invest, 2017, 40(9): 899-909.
[2] Gao C, Sun X, Lu L, et al. Prevalence of gestational diabetes mellitus in mainland China: a systematic review and meta-analysis. J Diabetes Investig, 2019, 10(1): 154-162.
[3] Arafa A, Dong J Y. Gestational diabetes and risk of postpartum depressive symptoms: A meta-analysis of cohort studies. J Affect Disord, 2019, 253:312-316.
[4] Simeonova-Krstevska S, Bogoev M, Bogoeva K, et al. Maternal and neonatal outcomes in pregnant women with gestational diabetes mellitus treated with diet, metformin or insulin. Open Access Maced J Med Sci, 2018, 6(5): 803-807.
[5] Ceasrine A, Devlin B, Bolton J, et al. Maternal diet disrupts the placenta-brain axis in a sex-specific manner. Brain Behav Immun, 2022, 106: 35.
[6] Contreras-Duarte S, Carvajal L, Fuenzalida B, et al. Maternal dyslipidaemia in pregnancy with gestational diabetes mellitus: possible impact on foetoplacental vascular function and lipoproteins in the neonatal circulation. Curr Vasc Pharmacol, 2018, 17(1): 52-71.
[7] Adam S, David McIntyre H, Tsoi K Y, et al. Pregnancy as an opportunity to prevent type 2 diabetes mellitus: FIGO Best Practice Advice. Int J Gynecol Obstet, 2023, 160: 56-67.
[8] Diabetes Association A. 2. classification and diagnosis of diabetes: Standards of medical care in diabetes-2019. Diabetes Care, 2019, 42(Suppl 1): S13-S28.
[9] Song C, Li J, Leng J, et al. Lifestyle intervention can reduce the risk of gestational diabetes: a meta-analysis of randomized controlled trials. Obes Rev, 2016, 17(10): 960-969.
[10] 冯燕红, 谢冰秀, 张康婧. 胰岛素联合饮食干预在GDM患者中的疗效及对血糖、炎症因子及应激反应的影响. 新医学, 2020, 51(10): 796-800.
[11] Zhang C, Rawal S, Chong Y S. Risk factors for gestational diabetes: is prevention possible? Diabetologia, 2016, 59(7): 1385-1390.
[12] Todoric J, Handisurya A, Leitner K, et al. Lipoprotein(a) is not related to markers of insulin resistance in pregnancy. Cardiovasc Diabetol, 2013, 12: 138.
[13] Zhao H, Li H, Chung A C K, et al. Large-scale longitudinal metabolomics study reveals different trimester-specific alterations of metabolites in relation to gestational diabetes mellitus. J Proteome Res, 2019, 18(1): 292-300.
[14] Rao C, Ping F. Second-trimester maternal lipid profiles rather than glucose levels predict the occurrence of neonatal macrosomia regardless of glucose tolerance status: a matched cohort study in Beijing. J Diabetes Complicat, 2021, 35(8): 107948.
[15] Doty M S, Chen H Y, Sibai B M, et al. Maternal and neonatal morbidity associated with early term delivery of large-for-gestational-age but nonmacrosomic neonates. Obstet Gynecol, 2019, 133(6): 1160-1166.
[16] Josefson J L, Scholtens D M, Kuang A, et al. Newborn adiposity and cord blood C-peptide as mediators of the maternal metabolic environment and childhood adiposity. Diabetes Care, 2021, 44(5): 1194-1202.
[17] Mitanchez D, Chavatte-Palmer P. Review shows that maternal obesity induces serious adverse neonatal effects and is associated with childhood obesity in their offspring. Acta Paediatr, 2018, 107(7): 1156-1165.
[18] Mitanchez D, Jacqueminet S, Lebbah S, et al. Relative contribution of gestational weight gain, gestational diabetes, and maternal obesity to neonatal fat mass. Nutrients, 2020, 12 (11): 3434.
(收稿日期:2023-03-03)
(本文編辑:林燕薇)

