Development and validation of a machine learning-based early prediction model for massive intraoperative bleeding in patients with primary hepatic malignancies
Jin Li,Yu-Ming Jia,Zhi-Lei Zhang,Cheng-Yu Liu,Zhan-Wu Jiang,Zhi-Wei Hao,Li Peng
Abstract BACKGROUND Surgical resection remains the primary treatment for hepatic malignancies,and intraoperative bleeding is associated with a significantly increased risk of death.Therefore,accurate prediction of intraoperative bleeding risk in patients with hepatic malignancies is essential to preventing bleeding in advance and providing safer and more effective treatment.AIM To develop a predictive model for intraoperative bleeding in primary hepatic malignancy patients for improving surgical planning and outcomes.METHODS The retrospective analysis enrolled patients diagnosed with primary hepatic malignancies who underwent surgery at the Hepatobiliary Surgery Department of the Fourth Hospital of Hebei Medical University between 2010 and 2020.Logistic regression analysis was performed to identify potential risk factors for intraoperative bleeding.A prediction model was developed using Python programming language,and its accuracy was evaluated using receiver operating characteristic (ROC) curve analysis.RESULTS Among 406 primary liver cancer patients,16.0% (65/406) suffered massive intraoperative bleeding.Logistic regression analysis identified four variables as associated with intraoperative bleeding in these patients: ascites [odds ratio (OR): 22.839;P <0.05],history of alcohol consumption (OR: 2.950;P <0.015),TNM staging (OR: 2.441;P <0.001),and albumin-bilirubin score (OR: 2.361;P <0.001).These variables were used to construct the prediction model.The 406 patients were randomly assigned to a training set (70%) and a prediction set (30%).The area under the ROC curve values for the model’s ability to predict intraoperative bleeding were 0.844 in the training set and 0.80 in the prediction set.CONCLUSION The developed and validated model predicts significant intraoperative blood loss in primary hepatic malignancies using four preoperative clinical factors by considering four preoperative clinical factors: ascites,history of alcohol consumption,TNM staging,and albumin-bilirubin score.Consequently,this model holds promise for enhancing individualised surgical planning.
Key Words: Primary liver cancer;Intraoperative bleeding;Machine learning;Model
INTRODUCTION
Primary liver cancer is a common cancer type worldwide,but especially in developing countries[1].Hepatocellular carcinoma (HCC) and intrahepatic cholangiocarcinoma (ICC) are the two most prevalent primary hepatic malignancies,followed by combined HCC and cholangiocarcinoma[2].HCC accounts for the vast majority of primary hepatic malignancies and is the third leading cause of cancer-related fatalities worldwide and the second leading cause of cancerrelated death in China[3,4],whereas ICC accounts for an estimated 5%-10% of all liver malignancies[5].Hepatitis B virus infection is responsible for up to 80% of liver cancer cases in China[6,7].Previously published studies demonstrated that infectious liver disease and intraoperative bleeding >1000 mL were independent factors that increased the odds of major complications.Age over 70 years,metastatic liver tumor,difficult liver resection,liver cirrhosis,and right hepatectomy were also factors that independently influenced prolonged postoperative length of stay after laparoscopic liver resection on multivariate analysis.In general,the prognosis for primary liver cancer is dismal,and especially so for cases with vascular metastases.Patients with early-stage HCC have a median life expectancy of 6-20 mo following diagnosis,with 3-and 5-year postoperative survival rates of 72% and 50%,respectively,and 5-year post-liver transplantation survival rates ranging from 48% to 61%[8-10].
Surgical resection is the primary treatment for hepatic malignancies[11-13],and intraoperative blood loss and transfusion requirements are closely related to perioperative morbidity and mortality in patients undergoing liver cancer surgery[14].Hepatic portal blocking is usually necessary to control intraoperative bleeding[15].In 1977,Foster and Berman published the results of a multicenter analysis of 621 patients who underwent hepatectomy for various indications,which showed that operative mortality rates exceeding 13% and 20% for hepatectomy and extended hepatic resection,respectively,with 20% of deaths resulting from bleeding[14,16].Leiet al[15] conducted a retrospective study involving 643 consecutive patients who underwent hepatic resection for HCC.The study identified several risk factors associated with major intraoperative blood loss in these patients.These risk factors included male gender,elevated alanine aminotransferase levels (>55 U/dL),decreased prothrombin time (<95%),resection of more than 3 Couinaud segments,en blocresection,low case volume of the surgeon (<65 cases),and central location of the tumor.
Therefore,it is imperative to develop a precise methodology for the anticipation of intraoperative hemorrhaging in individuals afflicted with hepatic malignancies,in order to facilitate the implementation of tailored therapeutic interventions for these patients.Developing a scientifically rigorous methodology to predict the probability of intraoperative hemorrhage in individuals with hepatic malignancies would not only optimize the selection of appropriate surgical interventions but also improve the allocation of limited resources.In the present study,through retrospective analysis of the clinical and preoperative data of patients with primary hepatic malignancies,factors associated with intraoperative bleeding were identified.The identified factors were then incorporated into the development of a prognostic model designed to predict cases of significant intraoperative hemorrhage.Validation of this model was conducted using various statistical methods,confirming its effectiveness.The utilization of this model has the potential to improve personalized surgical planning.
MATERIALS AND METHODS
Study population
Patient data for individuals with primary hepatic malignancies who underwent radical resection in the Department of Hepatobiliary Surgery of the Fourth Hospital of Hebei Medical University from 2010-2020 were analyzed retrospectively.Patients were included in this study according to the following criteria: (1) Both male and female participants between the ages of 18 and 75 years;(2) Good overall health condition and ability to tolerate anesthesia,pneumoperitoneum,and laparoscopic liver resection;(3) Liver function classification according to Child-Pugh score A or B,with a residual liver volume to standard liver volume ratio greater than 40%;(4) Presence of a single HCC with a tumor size not exceeding 10 cm;and (5) No evidence of tumor invasion or thrombosis in major hepatic vessels,and no intrahepatic or extrahepatic metastasis.Patients were excluded if they met any of the following exclusion criteria: (1) A history of esophageal variceal hemorrhage,severe hypersplenism syndrome,or refractory ascites;(2) Any preoperative anticancer treatments including transcatheter arterial chemoembolization,radiofrequency ablation,radiotherapy;(3) Postoperative pathology suggested metastatic liver cancer or primary liver cancer of another tissue type;(4) Previous or concomitant malignancies;(5) In patients who have a prior history of increased bleeding risk or are known to have tumor-related coagulopathy;and (6) Presence of preoperative tumor ruptured.This study was approved by the Ethics Committee of the Fourth Hospital of Hebei Medical University.Rigorous adherence to a confidentiality policy was observed in all data manipulations,and the present investigation adhered to the principles outlined in the Declaration of Helsinki.The hospital ethics committee waived the requirement for written,informed patient consent due to the retrospective study design.
Data extraction
For all included patients,baseline characteristics,laboratory parameters,and pathological tumor features were collected.Demographic variables included gender,age,height,weight,and history of alcohol consumption.Laboratory parameters included platelet count,hemoglobin level,alanine aminotransferase level,prothrombin time,aspartate aminotransferase level,albumin level,direct bilirubin level,total bilirubin level,methemoglobin level,unconjugated bilirubin level,and carcinoembryonic antigen level.Tumor characteristics included pathologic staging,number of lesions,maximum lesion diameter,and cancer emboli.Similarly,coexisting infections such as hepatitis B virus infection,cirrhosis,and ascites were also considered.The TNM stage was used for the cancer stage,and the patient's general health was represented by the Eastern Cooperative Oncology Group score.Liver function was assessed using Child-Pugh grade,albumin bilirubin score (ALBI),and ALBI grade.The rate of massive intraoperative bleeding was calculated based on 28 indicators,as published previously,and our clinical experience.According to the available data,the etiology of primary liver cancer in each patient was evaluated and classified.
Statistical analysis
Python software (version 3.7.1) and R language software (version 3.6.3) were used for calculations and analyses.Continuous variables are expressed as mean ± SD or median and interquartile range.Categorical variables are expressed as total and percentage.The Kruskal-Wallis test was applied to compare continuous variables between two groups,and the Chi-square test for variance was used to compare categorical variables between two groups.Two-tailedPvalues <0.05 were assumed to indicate a statistically significant difference.
Logistic regression analysis was performed to screen variables associated with intraoperative massive bleeding and transfusion requirements.Based on the scikit-learn algorithm of the machine learning (ML) library,a prediction model based on the identified variables was constructed using Python[17].We conducted an evaluation of the area under the curve (AUC) values for five distinct ML models in order to ascertain the most appropriate model for our study,as depicted in Supplementary Figure 1.According to the findings,logistic regression exhibited superior AUC compared to the other four models within the medical domain.R software was used to develop the nomogram,perform logistic regression analysis,and generate decision-making,calibration,and clinical impact curves.

Figure 1 Flow chart of patient inclusion.
RESULTS
Baseline characteristics of the included liver cancer patients
A retrospective screening was conducted on data for a cohort of 445 patients diagnosed with primary hepatic malignancies.Through the screening process,a total of 406 patients were identified as meeting the predetermined inclusion criteria for the study (Figure 1).The clinical data for all 406 patients are presented in Supplementary Table 1.Blood loss exceeding 1000 mL was defined as massive bleeding.Among the 406 patients,65 (16.0%) suffered massive intraoperative bleeding (>1000 mL),while the median bleeding volume among patients was measured at 1267.4 mL,291 (71.7%) had a history of hepatitis B,and 290 (71.4%) had cirrhosis.
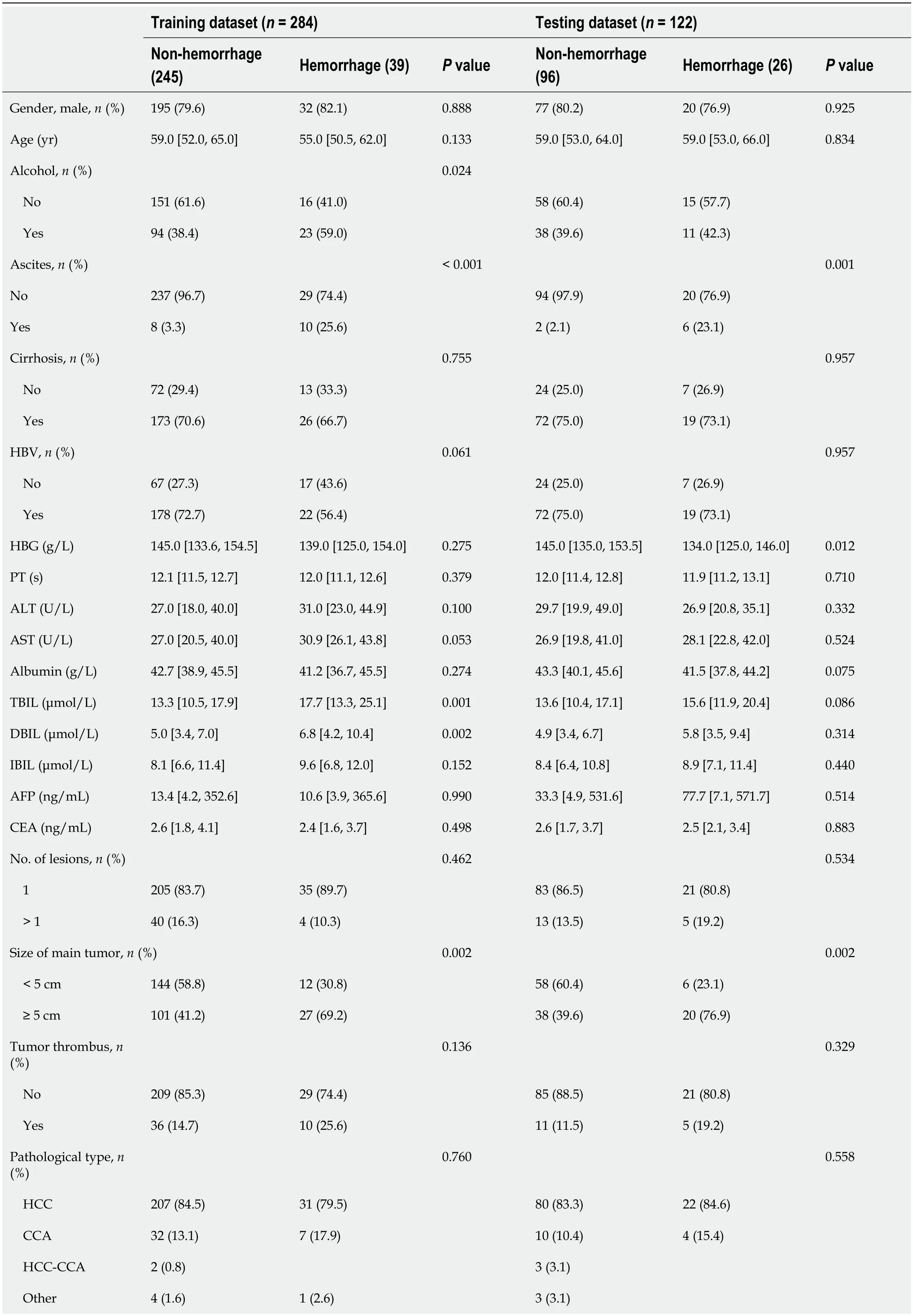
Table 1 Baseline characteristics of primary liver cancer patients in the training and prediction sets
The study cohort was divided randomly into two sets: 70% of cases to the training set,which was utilized for model training,and the remaining 30% of cases to the prediction set,which was used for model testing.Comparison of the basic and clinical characteristics of patients in the training and prediction sets showed no statistically significant differences (Table 1).Notably,14% of the training set (39/284) and 21% of the prediction set (26/122) exhibited indications of substantial intraoperative hemorrhage.
Development and evaluation of prediction model
Among the 28 variables described in the Methods section,21 associated with massive intraoperative bleeding based on clinical experience were included in the univariate analysis (Table 1).Variables for whichP<0.2 on univariate analysis were included in the subsequent multivariate analysis (Table 2).Then the ML model was constructed using the variables for whichP<0.05 on multivariate analysis.Four variables were identified as predictors of massive intraoperative bleeding and transfusion requirements: ascites [odds ratio (OR): 22.839;P<0.05],history of alcohol consumption (OR: 2.950;P<0.015),TNM staging (OR: 2.441;P<0.001),and ALBI score (OR: 2.361;P<0.001).From receiver operating characteristic curve analysis,the AUC values for the ability of the developed model to predict massive intraoperative bleeding were 0.844 in the training set and 0.803 in the test set (Figure 2).The predictive performance of the model (AUC=0.844) was found to be significantly higher compared to the individual factors of history of alcohol consumption (AUC=0.603),ascites (AUC=0.612),and ALBI score (AUC=0.580;Figure 3).The analysis also encompassed the examination of correlations among the variables incorporated in the study,as depicted in Figure 4.
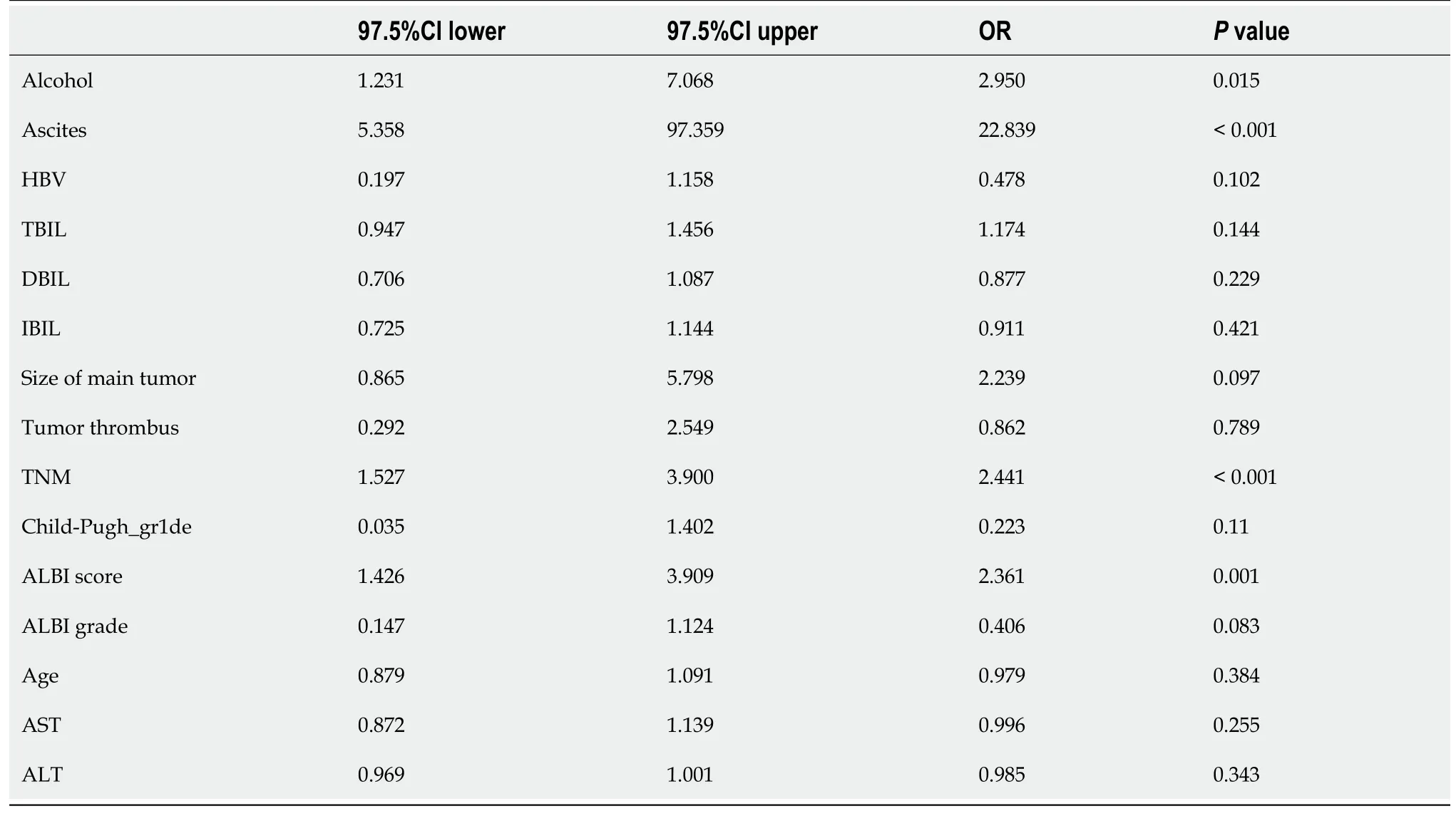
Table 2 Results of multifactor analysis of variables associated with intraoperative bleeding in primary liver cancer patients
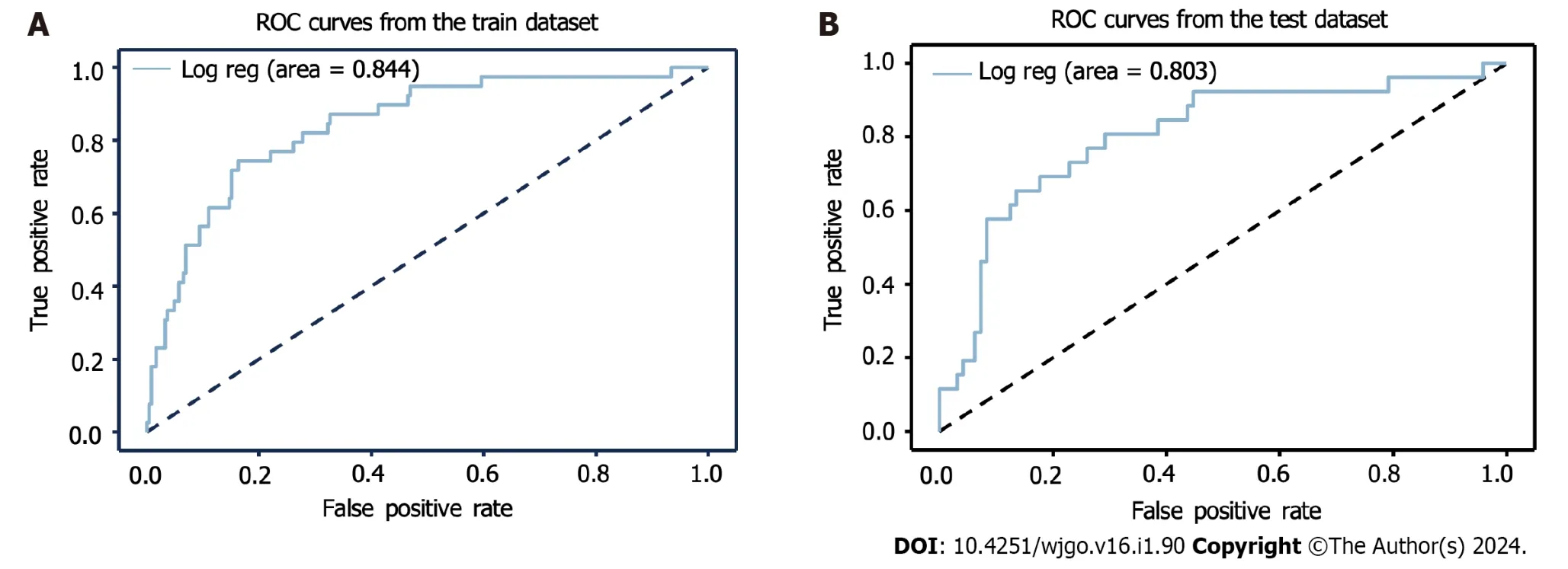
Figure 2 Predictive performance of the developed model. Model discrimination was evaluated based on area under the curve values,which were (A)0.844 in the training set and (B) 0.803 in the prediction set.ROC: Receiver operating characteristics.
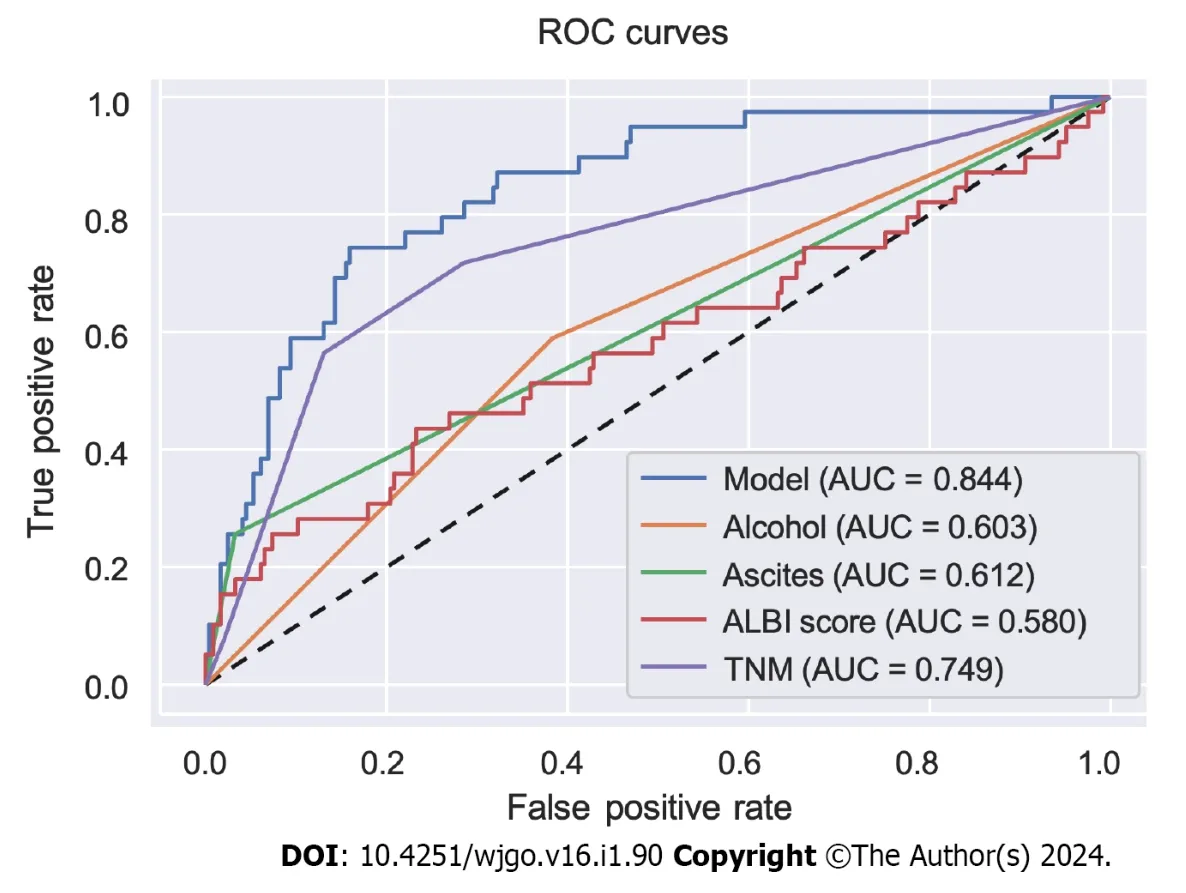
Figure 3 Receiver operating characteristics curves for the prediction model compared with the individual variables included in the model. ROC: Receiver operating characteristics;AUC: Area under the curve;ALBI: Albumin bilirubin.

Figure 4 Correlogram demonstrating the correlation between variables in the prediction model. ALBI: Albumin bilirubin.
Prediction nomogram construction
Based on the four variables identified by the logistic regression analysis,a nomogram was developed to predict the massive intraoperative bleeding among patients with hepatic malignancy (Figure 5).The calibration curve demonstrated a high level of concordance between the projected incidence derived from the logistic regression model and the observed outcomes within the cohort (Figure 6).The nomogram demonstrates reliable predictive ability for estimating thelikelihood of significant intraoperative bleeding in patients with hepatic malignancies.According to the clinical impact curves,the model demonstrated superior standardized net benefits for predicting patient outcomes compared to the individual factors of ascites,alcohol consumption history,TNM stage,and ALBI score (Figure 7).malignancies.The model showed superior standardized net benefit over the individual factors included (ascites,alcohol consumption,TNM staging,and albumin bilirubin score).ALBI: Albumin bilirubin.
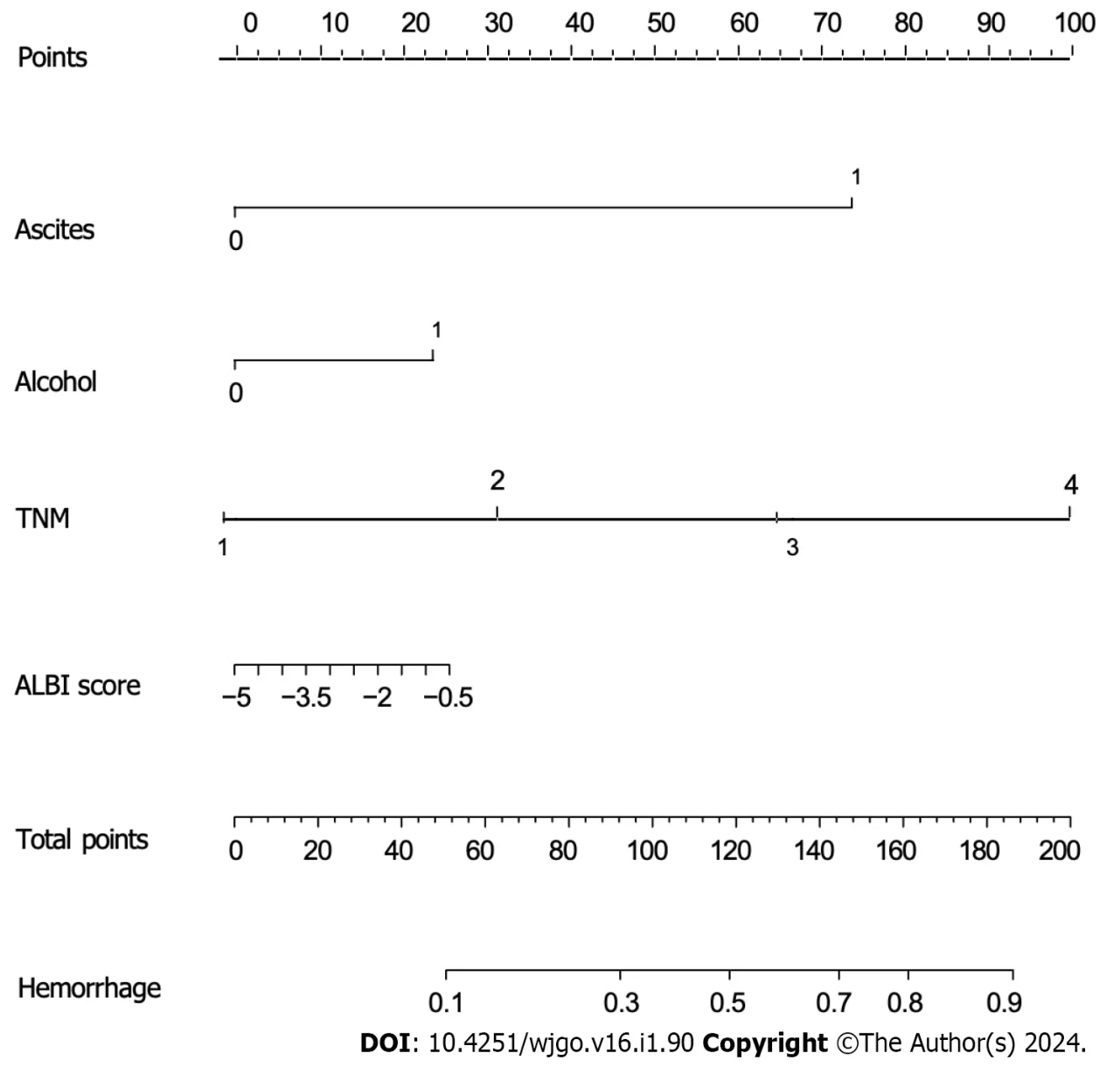
Figure 5 Nomogram for the prediction of intraoperative bleeding in patients with primary hepatic malignancies based on significant variable identified by the logistic regression model. ALBI: Albumin bilirubin.

Figure 6 Calibration curves for the prediction of intraoperative bleeding in patients with primary hepatic malignancies. Nomogram-predicted intraoperative bleeding in patients with primary hepatic malignancies is plotted on the X-axis,and actual intraoperative bleeding in patients with primary hepatic malignancies is plotted on the Y-axis.

Figure 7 Decision and clinical impact curves for use of the nomogram to predict intraoperative bleeding in patients with primary hepatic
DISCUSSION
As of present,efficacious treatment modalities for primary hepatic malignancies remain limited to hepatectomy[18].Although advancements in perioperative management as well as hepatectomy techniques have led to better outcomes for patients[19,20],massive intraoperative blood loss remains a common complication with these procedures that can adversely affect postoperative outcomes[14,21].In a comprehensive investigation conducted by Melendezet al[22],including a cohort of 496 individuals who underwent hepatectomy,it was observed that the median blood loss was 645 mL.However,the mean blood loss was higher at 848 mL,with a considerable degree of variability observed among patients,ranging from 40 to 9000 mL.Thus,given the considerable variability in blood loss,it is necessary to develop a predictive model to estimate the probability of massive intraoperative bleeding in patients diagnosed with primary hepatic malignancies.Despite previous studies investigating variables associated with severe intraoperative bleeding after hepatectomy,there has been a scarcity of research focusing on prediction models specifically for major intraoperative bleeding in patients with primary hepatic malignancies.In a study of 438 patients by Kawaguchiet al[23],hypertensive disease,preoperative chemotherapy,posterior superior resection,and partial hepatectomy were independent risk factors for increased bleeding during hepatectomy[23].A distinct study revealed that male gender and decreased prothrombin activity were correlated with an increased risk of experiencing higher blood loss during hepatectomy[24].Katzet al[25] applied multivariate analysis to identify factors that contribute significantly to blood loss during hepatectomy in patients diagnosed with hepatocellular malignancy.The variables identified as significant predictors include male sex,major hepatectomy,operating time,and vascular invasion,and they also reported that significantly increased bleeding during hepatectomy for hepatocellular malignancy was an independent prognostic factor for tumor recurrence and death[25].The present research differs significantly from prior studies in that patients in the previous studies had partial hepatectomy for a variety of reasons,while all patients in the current study had primary hepatic malignancies.In contrast to previous studies that considered both preoperative and intraoperative factors,the current study specifically aimed to identify preoperative variables associated with intraoperative bleeding in patients with primary hepatic malignancies.This approach was adopted to develop a prediction model applicable before surgical intervention for these patients.In our investigation,a prognostic model was formulated utilising four clinical variables (ascites,history of alcohol consumption,TNM staging,and ALBI score),its efficacy for predicting substantial intraoperative haemorrhaging in individuals diagnosed with primary hepatic malignancies was evaluated.The model was subsequently validated to ensure its reliability and accuracy.Multiple statistical methodologies were employed to verify the satisfactory performance of the model.Using the predicted risk of significant intraoperative hemorrhage determined by the patient's nomogram score,this model has the potential to notify and alert the attending physician and surgeon.Consequently,they can implement proactive and effective treatment interventions before and during the surgical procedure for patients who show a heightened vulnerability to substantial intraoperative bleeding.
Limitations
This study has several limitations that need to be acknowledged.Firstly,it was a single-center study with internal validation only,lacking external validation,which restricts the generalizability of the model.Therefore,larger multicenter studies are required to validate these findings.The impact of tumor location within the liver on intraoperative bleeding was not considered in the study design.Furthermore,while the study focused on preoperative factors,the inclusion of intraoperative factors could provide valuable insights for guiding intraoperative decision-making regarding bleeding control methods.Hence,further analyses incorporating intraoperative factors are warranted.Lastly,prospective studies with longer follow-up periods are crucial to confirm and enhance the performance of the developed prediction model.
CONCLUSION
In summary,screening of preoperative clinical factors in patients with primary hepatic malignancies identified four variables associated with massive intraoperative bleeding,which were then used to construct a model and corresponding nomogram for the preoperative prediction of such bleeding in these patients.The developed model has the potential to improve individualized surgical planning for patients with primary hepatic malignancies,leading to enhanced outcomes and optimal utilization of limited medical resources.
ARTICLE HIGHLIGHTS
Research background
Surgical removal is the primary treatment for hepatic malignancies,but intraoperative bleeding poses a significant risk to patients with hepatic malignancies.Accurate prediction of intraoperative bleeding is crucial for preventing complications and improving treatment outcomes.
Research motivation
This study aimed to develop a predictive model for significant intraoperative blood loss in patients with primary liver malignancies.By identifying preoperative factors associated with intraoperative bleeding,we can improve surgical planning and provide safer and more effective treatment for these patients.
Research objectives
This study aimed to identify risk factors for intraoperative bleeding in primary liver malignancies and develop a predictive model to estimate significant intraoperative blood loss.
Research methods
A retrospective analysis was conducted on primary liver malignancy patients who underwent surgery at the Hepatobiliary Surgery Department of the Fourth Hospital of Hebei Medical University between 2010 and 2020.Logistic regression analysis was used to identify risk factors for intraoperative bleeding.A predictive model was developed using Python programming.The model’s accuracy was evaluated using receiver operating characteristic (ROC) curve analysis.
Research results
Among 406 patients with primary liver cancer,16.0% (65/406) experienced significant intraoperative bleeding.Logistic regression analysis revealed four variables that were significantly associated with intraoperative bleeding: Ascites,alcohol consumption history,TNM staging,and albumin-bilirubin score.These variables were utilized to construct a predictive model.The model demonstrated good predictive accuracy,as evidenced by area under the ROC curve values of 0.844 in the training set and 0.80 in the prediction set.
Research conclusions
This study successfully developed and validated a predictive model for significant intraoperative blood loss in patients with primary liver malignancies,using preoperative clinical factors.Implementation of this model has the potential to enhance personalized surgical planning and improve patient outcomes.
Research perspectives
Further research is needed to assess the impact of implementing the predictive model on surgical decision-making,patient safety,and overall clinical outcomes to determine its real-world effectiveness and benefits.
FOOTNOTES
Author contributions:Li J,Peng L and Jia YM conceived and designed research;Zhang ZL,Liu CY and Jiang ZW collected data and conducted research;Li J,Peng L and Hao ZW analyzed and interpreted data;Li J,Jia YM and Peng L wrote the initial draft;Li J and Peng L revised the manuscript;Li J had primary responsibility for final content;all authors read and approved the final version of the manuscript.
Institutional review board statement:This study was approved by the Ethics Committee of the Fourth Hospital of Hebei Medical University.All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and national research committee and with the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards.
Informed consent statement:Due to the retrospective study design,the need for written,informed patient consent was waived by the hospital ethics committee.
Conflict-of-interest statement:The authors declare that they have no conflict of interest.
Data sharing statement:The datasets generated and analyzed during the current study are not publicly available due to limitations of ethical approval involving the patient data and anonymity but are available from the corresponding author on reasonable request.
Open-Access:This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers.It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license,which permits others to distribute,remix,adapt,build upon this work non-commercially,and license their derivative works on different terms,provided the original work is properly cited and the use is non-commercial.See: https://creativecommons.org/Licenses/by-nc/4.0/
Country/Territory of origin:China
ORCID number:Jin Li 0009-0004-1989-2309;Yu-Ming Jia 0000-0001-8796-2605;Zhi-Lei Zhang 0009-0004-0591-9056;Cheng-Yu Liu 0000-0003-2140-2706;Zhan-Wu Jiang 0000-0001-8690-2635;Zhi-Wei Hao 0009-0008-2550-0438;Li Peng 0009-0003-1568-9760.
S-Editor:Yan JP
L-Editor:A
P-Editor:Zhang XD
 World Journal of Gastrointestinal Oncology2024年1期
World Journal of Gastrointestinal Oncology2024年1期
- World Journal of Gastrointestinal Oncology的其它文章
- Comprehensive analysis of the role of ubiquitin-specific peptidases in colorectal cancer: A systematic review
- Colonoscopy plays an important role in detecting colorectal neoplasms in patients with gastric neoplasms
- Analysis of the potential biological value of pyruvate dehydrogenase E1 subunit β in human cancer
- Colorectal cancer’s burden attributable to a diet high in processed meat in the Belt and Road Initiative countries
- Emerging role of liquid biopsy in rat sarcoma virus mutated metastatic colorectal cancer: A case report
- Comprehensive evaluation of rare case: From diagnosis to treatment of a sigmoid Schwannoma: A case report
