Efficacy observation of acupuncture for dry eye syndrome of lung-yin deficiency pattern
Liu Jing-wen (刘璟文), Zhao Yao-dong (赵耀东), Zhu Ling (朱玲), Han Cong (韩聪)
Gansu University of Chinese Medicine, Lanzhou 730000, China
Abstract
Keywords: Acupuncture Therapy; Acupuncture Reinforcing Method; Tear Break-up Time; Tear Secretion; Lung-yin Deficiency; Dry Eye Syndrome
Dry eye syndrome (DES) is a type of ocular surface disease that can be triggered by multiple factors, such as tear hyperosmolarity, ocular surface inflammation and injury, tear film instability and neural paresthesia, usually manifesting as loss of tear film stability and ocular surface symptoms[1]. The incidence of DES was estimated as high as 21%-30% in China[2]. In treatment of DES, acupuncture can notably improve ocular blood circulation, adjust meridian qi and balance yin-yang, so as to nourish the eyes[3]. To enhance the clinical efficacy in acupuncture treatment of DES, we applied Zheng’s distinctive needling manipulations, Er Long Xi Zhu (two dragons playing with a pearl) and Guo Yan Re (heat produced to reach the eyes), during clinical practice. The report is given as follows.
1 Clinical Materials
1.1 Diagnostic criteria
1.1.1 Diagnostic criteria in Western medicine
Based on the diagnostic criteria for DES in the Expert Consensus on Clinical Diagnosis and Treatment of Dry Eye (2013)[2]: the diagnosis can be made given one of the subjective symptoms including dryness, foreign body sensation, burning sensation, fatigue, or discomfort in the eyes, change in visual acuity (VA) and photophobia plus tear break-up time (BUT) ≤5 s or Schirmer tear test-1 (STT-1, without topical anesthesia, 5 min) ≤5 mm; or with one of the subjective symptoms including eye dryness, foreign body sensation, burning sensation, visual fatigue, discomfort and change in VA plus BUT >5 s but ≤10 s or STT-1 (5 min) >5 mm but ≤10 mm, together with positive corneal and conjunctival fluorescein staining.
1.1.2 Pattern differentiation criteria in traditional Chinese medicine (TCM)
The TCM pattern differentiation referred the pattern of lung-yin deficiency due to ‘impending desiccation of holy water’[4]. Primary symptoms: lack of moisture, eye dryness and ache; secondary symptoms: dryness in the mouth and nose, and dry stool; tongue and pulse: red tongue body covered by thin white coating without sufficient moisture, and thin and rapid pulse.
1.2 Inclusion criteria
Conformed to the above diagnostic criteria in Western medicine and the differentiation criteria for lung-yin deficiency in TCM; aged 18 to 70 years old; not on other medications or had suspended the medication for at least 2 weeks; willing to participate in the trial and signed the informed consent form.
1.3 Exclusion criteria
Coupled with other diseases which required special intervention that may influence the current trial; had a history of immune disease; tests for anti-Smith surface antigen (SSA) and anti-SjÖgren’s syndrome B antibody (SSB) showed positive, suggesting that the dryness or discomfort in the eyes may be caused by SjÖgren’s syndrome; unable to receive treatment as required or feared of needles; pregnant or breast-feeding women; patients with severe cardiovascular diseases or other internal conditions, or immune diseases.
1.4 Elimination criteria
Failed to receive treatment as required; with incomplete medical data so that the efficacy or safety evaluation may be affected.
1.5 Statistical methods
SPSS version 20.0 software was adopted for data processing in this study. The distribution was tested in measurement data first. Those consistent with normal distribution were expressed as mean ± standard deviation (±s), with paired-samplest-test used for intra-group comparisons and independent-samplet-test for between-group comparisons when variance satisfied homogeneity andt’-test if not. Measurement data not in line with normal distribution were expressed as median (interquartile range, IQR) and analyzed using non-parametric test. Ordinal data were analyzed by rank-sum test. Enumeration data were processed using Chi-square test. Statistical significance was accepted whenP<0.05.
1.6 General data
Fifty-six eligible DES patients were enrolled from the Ophthalmology and Acupuncture-moxibustion Departments of the Affiliated Hospital of Gansu University of Chinese Medicine between October 2018 and August 2019. They were coded 1-56 according to their visiting sequence. Fifty-six numbers were successively selected on the random number table from the right side of the sixth line and sixth rank, with 1-28 allocated to the observation group and 29-56 to the control group. The general data were statistically equal between the two groups before treatment, suggesting the comparability (Table 1).
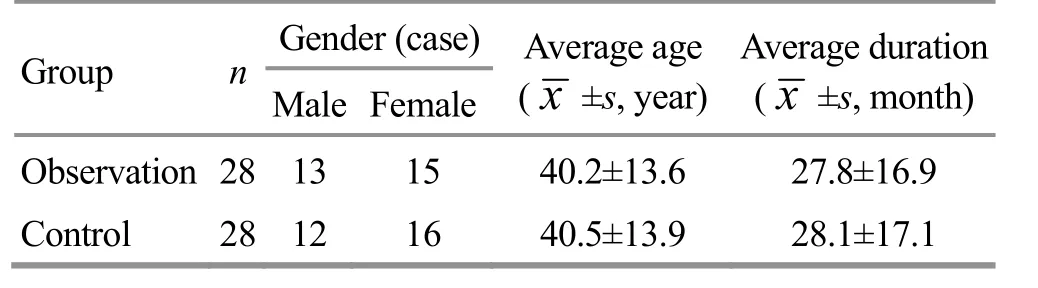
Table 1. Comparison of the general data between the two groups
2 Treatment Methods
The two groups were treated with different needling manipulations but the same group of acupoints.
Major acupoints: Cuanzhu (BL 2), Sizhukong (TE 23), Taiyang (EX-HN 5) and Fengchi (GB 20).
Adjunct acupoints: Feishu (BL 13) and Chize (LU 5).
The acupoints were selected from both sides and treated once a day, for two sets of 15 consecutive days at a 2-day interval. The therapeutic efficacy was estimated afterwards.
2.1 Observation group
The patient took a sitting position. The acupoints were sterilized using iodophor. Disposable sterile filiform needles of 0.30 mm in diameter and 40 mm in length were perpendicularly punctured into Fengchi (GB 20) till 30-35 mm with the tip towards the contralateral eye. Guo Yan Re needling manipulation[5]was applied when needling qi was obtained. The physician heavily pressed the acupoint with the left thumb and slowly inserted the needle with the right hand. When needling qi was achieved, the left thumb pressed down more heavily and the right thumb pushed forward to twirl the needle handle for 9 times. The patient should have a tender and comfortable feeling while the physician should feel tense and sunken with the needling. Then, heavily thrust and gently lifted the needle for 9 times and twirled the needle handle for another 9 times in the same direction. The needle tip should be fixed at where the needling qi was obtained. Meanwhile, the left thumb pressed upward. The whole process needed performing again if there was no hot or distending feeling. The physician needed to repeat the manipulation for another 1 min since the patient felt a hot and distending sensation generating from Fengchi (GB 20) and traveling till the eye. Removed the needle immediately and the needled area should be pressed at the removal with the left thumb. Afterwards, the patient lied down on his front and the physician used disposable filiform needles of 0.30 mm in diameter and 40 mm in length to obliquely insert Feishu (BL 13), with twirling reinforcing manipulation applied after needling qi was obtained, and the needle was also removed immediately. Then the patient took a supine position to receive acupuncture at Cuanzhu (BL 2), Sizhukong (TE 23) and Taiyang (EX-HN 5) by filiform needles of 0.30 mm in diameter and 25 mm in length to obliquely downward insert to 10-20 mm deep. Er Long Xi Zhu manipulation[6]was performed when needling qi arrived. The physician pressed heavily at the acupoint with the left index finger and swiftly inserted needle with the right hand. When needling qi was got, pushed the left index finger and twirled the needle tip simultaneously towards the upper eyelid 3-5 times to make the needling sensation transmit to the upper eyelid and eyeball. Then lifted the needle till subcutaneous layer and twirled the needle tip and pushed the left index finger for another 3-5 times to make the needling sensation transmit to the lower eyelid and eyeball. The ocular region should be brimming with needling sensation. Chize (LU 5) was perpendicularly punctured by disposable filiform needles of 0.30 mm in diameter and 40 mm in length, with twirling reinforcing manipulation performed after needling qi was obtained. The needles were removed slowly 30 min later and the points were pressed immediately at the removal.
2.2 Control group
The patient took a prone position first. After routine sterilization of the acupoints, Feishu (BL 13) was inserted by disposable filiform needles of 0.30 mm in diameter and 40 mm in length with the needle tip towards the spine, obliquely by a depth of 25 mm. Twirling reinforcing manipulation was performed for 1 min and the needles were removed immediately afterwards. Then, the patient turned to a supine position. Disposable needles of 0.30 mm in diameter and 40 mm in length were chosen to treat Fengchi (GB 20) and Chize (LU 5). The needle was obliquely punctured into Fengchi (GB 20) with the needle tip towards the contralateral eye for a depth of 30 mm, while Chize (LU 5) was perpendicularly punctured 30 mm deep. Twirling reinforcing manipulation was performed upon the arrival of needling qi. Cuanzhu (BL 2), Sizhukong (TE 23) and Taiyang (EX-HN 5) were treated with filiform needles of 0.30 mm in diameter and 25 mm in length by oblique insertion for a depth of 10-20 mm. Twirling reinforcing manipulation[7]was conducted when needling qi was obtained, i.e. pressed the acupoint with the left thumb and inserted the needle with the right hand, pushed the right thumb forward while pulling the index finger backward to twirl the needle handle upon the arrival of needling qi by 180-360° at 90 times/min, continuously and repeatedly for 1 min. The needles were gently and slowly removed 30 min later and the acupoints should be pressed at the removal.
3 Observation of Therapeutic Efficacy
3.1 Observation items
3.1.1 STT-1
Took a piece of tear detection strip (Tianjin Jingming New Technological Development Co., Ltd., China) and folded it at 5 mm using a pair of sterile tweezers, and then placed it in the conjunctival sac at the outer 1/3 of the lower eyelid. The patient then closed his eyes for 5 min and the strip was collected afterwards. The length of the moisturized part of the strip from the fold was measured. A length of 10-15 mm was taken as the normal range, while a length <5 mm would be recognized as dry eye.
3.1.2 BUT
Fluorescein sodium solution was dropped at the fornix. Asked the patient to blink several times to let the solution evenly stain the cornea. Then the patient stare straight forward without blink to allow the doctor to count the time till the tear film collapsed. The measurement was done three times to obtain the mean value. BUT <5 s was considered as dry eye.
3.1.3 Ocular surface symptom score
The common clinical symptoms in DES were scored based on theGuiding Principles for Clinical Study of New Chinese Medicines[8]and the sum of each symptom score was taken as the general score of ocular surface symptoms. The two eyes were scored separately.
Dryness in the eyes was taken as the primary symptom: no symptom, scored 0 point; accidentally, 2 points; often, 4 points; unbearable dryness, 6 points.
Secondary symptoms included visual fatigue, foreign body sensation, red eye, photophobia and distending pain. Foreign body sensation: no symptom, 0 point; mild, 1 point; obvious, 2 points; unbearable, 3 points. Visual fatigue: no symptom, 0 point; easy to feel fatigue, 1 point; notably shortened use of eyes, 2 points; unable to look at things due to involuntary close of eyes,3 points. Photophobia, red eye and distending painful eyes were categorized into 4 levels, i.e. 0, 1, 2 and 3 points.
The full score of ocular surface symptoms was 21 points, the higher the score, the more severe the symptoms.
3.2 Criteria for therapeutic efficacy
The efficacy was estimated by referring theCriteria of Diagnosis and Therapeutic Effects of Diseases and Syndromes in Traditional Chinese Medicine[4]in combination with the therapeutic efficacy index.
Therapeutic efficacy index = (Pre-treatment ocular surface symptom score - Post-treatment ocular symptom score) ÷ Pre-treatment ocular surface symptom score × 100%.
Cured: The dry eye symptoms were gone and the therapeutic efficacy index ≥95%; STT-1 (5 min) ≥10 mm; BUT ≥10 s.
Markedly effective: Therapeutic efficacy index 70%-95%; STT-1 (5 min) >5 mm, <10 mm; BUT >5 s, <10 s.
Effective: Therapeutic efficacy index ≥30%, <70%.
Invalid: Therapeutic efficacy index <30%, and the other outcome measures were not improved.
3.3 Results
3.3.1 Comparison of the clinical efficacy
The total effective rate was 92.8% in the observation group, higher than 71.4% in the control group, and the between-group difference was statistically significant (P<0.05), (Table 2).
3.3.2 Comparison of the ocular symptom score, BUT and STT-1
The ocular symptom score, BUT and STT-1 were statistically equal between the two groups before treatment (allP>0.05). After treatment, the ocular symptom score declined significantly in both groups (bothP<0.01); the BUT and STT-1 increased after treatment in both groups (allP<0.05). After treatment, the observation group showed significant advantages comparing the ocular symptom score, BUT and STT-1 compared with the control group (allP<0.05). The details are displayed in Table 3.
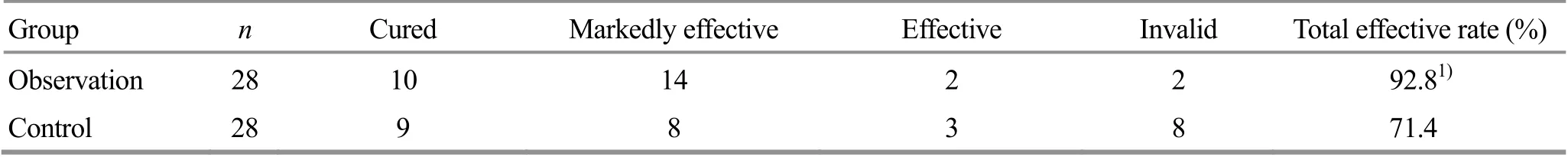
Table 2. Comparison of the clinical efficacy (case)
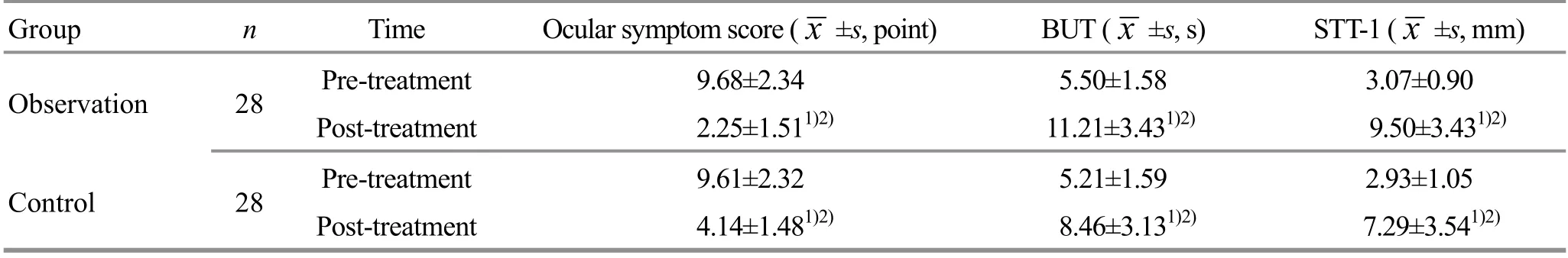
Table 3. Comparison of the ocular symptom score, BUT and STT-1
4 Discussion
DES belongs to Bai Se Bing (cloudy and dry eye) or Gan Se Hun Hua Zheng (dry eye with blurred vision) in traditional Chinese medicine (TCM). DES of lung-yin deficiency affects the eyes but its pathogenesis is insufficient yin fluid in the lung and poor qi activity for transportation and distribution[9]. Lung is in charge of qi and lung qi goes up to gather at the whites of the eyes[10]. When there is no enough yin fluid in the lung, lung qi will fail to diffuse and yin fluid cannot be transported to the eyes, resulting in dryness in the eyes. The Foot Taiyang, Hand and Foot Shaoyang, as well as Hand Taiyin Meridians are all associated with the eyes. If these meridians are blocked and meridian qi cannot travel through, the eyes won’t get sufficient nutrition[11]. We combined Guo Yan Re and Er Long Xi Zhu, two types of Zheng’s acupuncture manipulation, to treat DES and we believe its mechanism mainly contains 4 aspects.
First, it is the acupoint selection. Cuanzhu (BL 2), Sizhukong (TE 23) and Taiyang (EX-HN 5) selected in this study are located around the eyes, thus belonging to topical acupoint selection. These points are all frequently selected in treatment of ocular diseases in clinic[12]. The three points used together can regulate the meridian qi around the eyes, elevate the level of qi and blood in the topical area and improve eye dryness, which is to treat the superficial manifestations. Fengchi (GB 20) is considered as proximal acupoint selection while Feishu (BL 13) and Chize (LU 5) are distal acupoint selection. Selection of these three acupoints reflects the indication characteristic that an acupoint can treat diseases that affect where its meridian passes. Besides, they act to dispel wind and unblock collaterals, regulate qi and promote the diffusion function of the lung, supplement yin for moisturizing the dryness, which is to treat the root cause. The combination of topical, proximal and distal acupoint selections is the reflection of three power (heaven, human, earth) point selection[13], which can nourish and moisturize the eyes in an all-round way, promote lung qi diffusion, supplement yin to moisturize the dryness, targeting both the manifestations and the root cause.
The second factor is the meridians. Cuanzhu (BL 2) and Feishu (BL 13) are from Bladder Meridian of Foot Taiyang, which originates from the inner canthus of the eyes[14]. It’s reported that Bladder Meridian was the most frequently selected meridian in treatment of DES[15]. Triple Energizer Meridian of Hand Shaoyang, where Sizhukong (TE 23) belongs, and Gallbladder Meridian of Foot Shaoyang meridian, where Fengchi (GB 20) belongs, are two meridians connected with the eyes. Gallbladder Meridian and Liver Meridian are interiorly-exteriorly related. Chize (LU 5) comes from Lung Meridian of Hand Taiyin, which belongs to the lung organ. The yin fluid can travel up though Liver Meridian from the lung to the eyes. Therefore, the above acupoints were used together to unblock and regulate meridians and collaterals, reinforce lung yin, and moisturize dryness.
The third factor is the relationship between manipulation and dose-effectiveness. Er Long Xi Zhu and Guo Yan Re are two unique manipulations inherited down in Zheng’s family, which have been proved effective in treating ophthalmological diseases[16]. Performing Guo Yan Re manipulation at Fengchi (GB 20), i.e. applying warming-unblocking manipulation consisting of reinforcing twirling manipulation twice and reinforcing thrusting-lifting manipulation once, can send the needling sensation directly to the affected body region, the eyes, which should be the premise of achieving therapeutic efficacy. Conducted after Guo Yan Re, which already sent the needling qi to the affected region, Er Long Xi Zhu mixed lifting-thrusting, twirling, and against-along meridian manipulations together to make eyes encircled by the needling qi, so as to further strengthen the effect of needling qi in the ocular region, harmonizing qi and blood and moisturizing the eyes, which should be the basis of achieving therapeutic efficacy. The two progressive manipulations not only targeted the affected eyes but also regulated the internal pathogenic factor, lung-yin deficiency, treating both the superficial manifestations and root cause and regulating yin-yang and qi-blood in an overall manner. Meanwhile, acupuncture at Fengchi (GB 20) is also beneficial to the circulation around the ciliary muscle[17]. The ordinary reinforcing twirling manipulation only applies small-amplitude twirling manipulation given the arrival of needling qi at the needled spot. It cannot send the needling qi to the affected region like the two special needling manipulations. Therefore, Guo Yan Re and Er Long Xi Zhu together won out the ordinary reinforcing manipulation comparing the dose- effectiveness and produced more notable effect on the pathogenesis and qi-blood in the ocular region[18]. This clinical study confirmed that combining Guo Yan Re and Er Long Xi Zhu in the observation group produced more significant efficacy than ordinary reinforcing twirling manipulation in the control group, as well as more notable improvements in the ocular surface symptom score, BUT and STT-1.
The fourth aspect is that modern research has discovered the effect of acupuncture at periocular points in boosting tear secretion, increasing tear film stability and improving the ocular symptoms[19]. There distributes the branches of supraorbital artery and vein at Cuanzhu (BL 2). Study showed that acupuncture at Cuanzhu (BL 2) could help with the ocular arterial blood flow and bring it back to the normal level. It is the infraorbital nerve located at Sizhukong (TE 23) and the zygomatic and temporal branches of facial nerve at Taiyang (EX-HN 5). Acupuncture at the above acupoints to treat DES can elevate tear production, slow down the apoptosis of lacrimal gland epithelial cells, and improve the state of cornea and nerve conduction through regulating autonomic nervous system and immune system[20].
To sum up, in acupuncture treatment of DES, using Guo Yan Re and Er Long Xi Zhu together can promote tear production and improve the symptoms via modulating blood vessels, nerves and immune system, producing significant clinical efficacy, and thus it is worthy of application and promotion in clinic.
Conflict of Interest
The authors declare that there is no potential conflict of interest in this article.
Acknowledgments
This work was supported by Project of Zheng’s Acupuncture Manipulation Academic School Heritage Studio, Gansu Province (甘肃郑氏针法学术流派传承工作室建设项目, No. 9983999957).
Statement of Informed Consent
Informed consent was obtained from all individual participants.
Received: 11 January 2020/Accepted: 9 March 2020
 Journal of Acupuncture and Tuina Science2021年1期
Journal of Acupuncture and Tuina Science2021年1期
- Journal of Acupuncture and Tuina Science的其它文章
- Effect of electroacupuncture on calcium-activated chloride channel currents in interstitial cells of Cajal in rats with diabetic gastroparesis
- Effect of electroacupuncture pretreatment on the protein expression of c-fos in fastigial nucleus and lateral hypothalamus area in rats with acute myocardial ischemia-reperfusion injury
- Effect of herb-partitioned moxibustion in improving tight junctions of intestinal epithelium in Crohn disease mediated by TNF-α-NF-κB-MLCK pathway
- Ginger-partitioned moxibustion plus pediatric massage for treating infantile diarrhea due to spleen deficiency: a randomized controlled clinical trial
- Efficacy observation of long-retaining scalp acupuncture plus interactive training for upper-extremity dysfunction after cerebral stroke
- Observation on therapeutic efficacy of thunder-fire moxibustion for hypomenorrhea after induced abortion
