Successful treatment of lower urinary tract obstruction with peritonealamniotic and vesicoamniotic shunting
Ümit Korucuoğlu, Anıl Içel Saygi, Yaşam Kemal Akpak, Özkan Özdamar, Aydan Biri
1Koru Hospital, Department of Obstetrics and Gynecology, Ankara, Turkey
2Ankara Military Hospital, Department of Obstetrics and Gynecology, Ankara, Turkey
3Gölcük Military Hospital, Department of Obstetrics and Gynecology, Ankara, Turkey
Successful treatment of lower urinary tract obstruction with peritonealamniotic and vesicoamniotic shunting
Ümit Korucuoğlu1, Anıl Içel Saygi2*, Yaşam Kemal Akpak2, Özkan Özdamar3, Aydan Biri1
1Koru Hospital, Department of Obstetrics and Gynecology, Ankara, Turkey
2Ankara Military Hospital, Department of Obstetrics and Gynecology, Ankara, Turkey
3Gölcük Military Hospital, Department of Obstetrics and Gynecology, Ankara, Turkey
Lower urinary tract obstruction (LUTO) which is most commonly caused by posterior urethral valves or urethral atresia, is often associated with high perinatal mortality and morbidity and long-term childhood renal dysfunction or even renal failure. LUTO is an uncommon clinical entity that can be diagnosed by ultrasonographic examination and is particularly presented by enlarged bladder, hydronephrosis, hydroureter and oligohydramnios. Despite being a rare pathology of the genitourinary tract, detection rates of it is higher than other congenital abnormalities with ultrasonography. Moreover, ultrasonography has become the most widely used diagnostic tool in the diagnosis of LUTO. Pulmonary hypoplasia resulting from severe oligohydramnios is the most common cause of death. Bladder drainage has a critical role on perinatal survival in fetuses with LUTO especially in those predicted to have a poor prognosis. Further interventions and observations of renal therapies may be required in childhood.
ARTICLE INFO
Article history:
Received 9 January 2015
Received in revised form 13 January 2015
Accepted 15 January 2015
Available online 20 January 2015
LUTO
PUV
Vesicoamniotic shunt
Bladder outlet obstruction
Pigtail catheter
1. Introduction
Genitourinary tract abnormalities are one of most detectable anomalies by sonography[1]. Lower urinary tract obstruction (LUTO) comprises a heterogeneous group of pathologies including posterior urethral valves (PUV) and urethral atresia[2]. Most causes of LUTO are PUV and urethral atresia[2]. Long-term obstructive effect of LUTO extensively induces renal parenchymal damage which, in turn, engenders to renal dysfunction and renal failure and bladder dysfunction in childhood. Oligohydramnios and pulmonary hypoplasia are two parameters of poor prognosis associated with high fetal mortality and morbidity[3].In uteroshunting is a significant antenatal intervention which has been applied for obstructive uropathy up to now[4]. Indications, ideal method of treatment and appropriate time forin uteroshunting are critical points for both perinatal survival and renal and bladder development, however postnatal long-term poor renal function may render a higher risk[5]. We report two cases performedin uteroshunting for LUTO.
2. Case report
2.1. Case 1
A 28-year-old woman G2P1 at 25 weeks of gestation admitted to outpatient clinic with abnormal ultrasound screening findings concerning gross fetal ascites and megacystis without oligohydramnios. Fetal termination had been offered due to perceived poor prognosis by the perinatologists in another healthcare facility. Megacystis without oligohydramnios, gross urinary ascites due to fetal bladder rupture, bilateral diaphragm elevation which caused fetal thoracic and cardiac compression and bilateral fetal pyelectasis were identified in our ultrasound screening (Figure 1). We performed amniocentesis for fetal karyotyping. After excluding major chromosomal anomalies we performed peritonealamniotic shunting by ultrasound-guided placement of double-ended pigtail catheter (Figure 2). Location ofcatheter and fetal viability were confirmed after procedure through subsequent serial ultrasound scans. Fetal ascites, megacystis and bilateral pyelectasis resolved during the following weeks. A healthy newborn was delivered vaginally at the 38 weeks gestation. Additionally abdominal ultrasound scan of the newborn was normal.
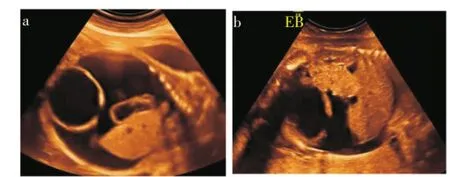
Figure 1. Ultrasound image of fetal bladder rupture.a: Fetal ascites without oligohydramnios; b: Fetal ascites.

Figure 2. A transaxial scan of the fetus after peritoneal-amniotic shunting in the following weeks.

Figure 3. Ultrasound image of enlarged bladder with oligohydramnios.

Figure 4. A transaxial scan of the fetus after vesicoamniotic shunting.
2.2. Case 2
A 24-year-old woman G1P0 at 19 weeks of gestation was referred from another obstetrics clinic to our outpatient clinic with abnormal ultrasound screening findings concerning fetal ascites and megacystis accompanying to oligohydramnios. Megacystis with oligohydramnios, gross fetal ascites, bilateral fetal pyelectasis were identified in our ultrasound screening (Figure 3). We performed amniocentesis for fetal karyotyping which revealed a normal chromosomal structure. Subsequently, vesicoamniotic shunting by ultrasound-guided placement of double-ended pigtail catheter (Figure 4). Fetal viability and catheter localization were ensured after the procedure, also with subsequent ultrasound scans. Fetal ascites, megacystis and bilateral pyelectasis were not identifiable during the following weeks. Healthy full-term newborn was delivered vaginally at another obstetrics clinic.
3. Discussion
LUTO is associated with high perinatal and childhood mortality and morbidity including bladder dysfunction or renal damage[5]. Excessive accumulation of urine and high pressure arising from bladder outlet obstruction causes to deterioration of the development of bladder and renal structure, bladder dysfunction, bilateral hydronephrosis with bilateral hydroureter and subsequent renal dysfunction and renal failure[5,6]. Development of urinary organs have associations with time period and degree of obstruction[7]. In our first case, bladder rupture, gross ascites, fetal thoracic and cardiac compression due to elevation of diaphragm were identified because of long-term obstruction. The two most common causes of LUTO are PUV and urethral atresia, other less common ones are prune belly syndrome and prostatic atresia[3,8]. The PUV is more common among male than female fetuses. Our both cases were male fetuses. Prenatal ultrasound plays impotant role on diagnosis and fetalin uterointervention for LUTO. Diagnosis time of LUTO ranges from 13 to 38 weeks, but most diagnoses are established at20-22 weeks gestation because of being time interval for routine detailed fetal anomaly scan[2,9]. Our cases admitted to outpatient clinic at 19 and 25 weeks gastation. Diagnosis should be evaluated by karyotype analysis and aspirated urine together[10]. For both cases we performed fetal karyotyping after amniocentesis. To evaulate renal function, serial fetal urine analysis of fetal urine is recommended inasmuch as LUTO has a progressive character[11]. In prognosis two most substantial causes related with higher mortality rate were oligohydramnios and pulmonary hypoplasia[3]. Oligohydramnios was identified in our second case. Morriset al.in their study demonstrated that all neonatal deaths were caused by pulmonary hypoplasia[2]. Because of mortality and morbidity due to pulmonary hypoplasia and renal dysplasia by obstruction-induced pressure, the appropriate timing forin uterointervention is critical. The main choices ofin uterotherapies include vesicocentesis, vesicoamniotic shunt, open foetal bladder surgery and fetal cystoscopy[5,8,9]. Double-ended pig tailed catheter is the most commonly used catheter to achieve bladder drainage. Sometimes double-basket catheter can be used for long-term shunting. Wonet al. demonstrated in their cases that double-basket catheter was effective for vesicoamniotic shunting for long-term decompression[10]. In our case, we used double-ended pig tailed catheter and we did not observe and catheter complication. Vesicoamniotic shunts are most commonin uterointerventions to relieve the obstructive uropathy. Morriset al.showed perinatal survival is increased significantly by fetal bladder drainage (OR: 2.53)[2]. And bladder drainage versus non-treatment with an OR of 3.86 is demonstrated in systematic observational studies[8,9]. After shunting, symptoms caused by obstruction disappeared in both cases. LUTO sometimes may be associated with certain congenital syndromes, such as prune belly syndrome, which is characterized with bladder outlet obstruction and abdominal muscle defiency[12]. Like our peritonel-amniotic shunt case, Livingstonet al.demonstrated bladder rupture and massive urinary ascites which caused thoracic and cardiac compression and subsequent potential hydrops fetalis after bladder outlet obstruction associated with mirror syndrome[13] . Obstructive uropathy was relieved after peritoneal-amniotic shunt[13]. Despite increasing perinatal survival, vesicoamniotic shunt might not have a long-term benefit[2]. Renal dysfunction and renal failure and bladder dysfunction can develop during postnatal follow-up years[14].
As a conclusion, the prenatal bladder drainage may improve perinatal survival in fetuses with LUTO. An appropriate timing of shunting is critical to preserve normalin uterorenal development. Improving perinatal survival via shunting is clear but long-term renal functional outcomes are sceptical and poor towards increasing rates of childhood morbidity based on observational studies.
Conflict of interest statement
The authors declare that they have no conflict of interest.
Consent
Written informed consent was obtained from the patient for publication of this case report and any accompanying images.
[1] Morris RK, Kilby MD. Long-term renal and neurodevelopmental outcome in infants with LUTO, with and without fetal intervention. Early Hum Dev 2011; 87: 607-610.
[2] Morris RK, Malin GL, Quinlan-Jones E, Middleton LJ, Hemming K, Burke D, et al. Percutaneous vesicoamniotic shunting versus conservative management for fetal lower urinary tract obstruction (PLUTO): a randomised trial. Lancet 2013; 382: 1496-1506.
[3] Lee J , Kimber C, Shekleton P, Cheng W. Prognostic factors of severe foetal megacystis. ANZ J Surg 2011; 81: 552-555.
[4] Pringle KC, Kitagawa H, Seki Y, Koike J, Zuccollo J. Development of an animal model to study congenital urinary obstruction. Pediatr Surg Int 2013; 29: 1083-1089.
[5] Kitagawa H, Seki Y, Nagae H, Aoba T, Manabe S, Ooyama K, et al. Valved shunt as a treatment for obstructive uropathy: does pressure make a difference? Pediatr Surg Int 2013; 29: 381-386.
[6] Jung E, Won HS, Shim JY, Lee PR, Kim A, Kim KS. Successful outcome following prenatal intervention in a female fetus with bladder outlet obstruction. Prenat Diagn 2005; 25: 1107-1110. [7] Confer SD, Galati V, Frimberger D, Kropp BP. Megacystis with an anterior urethral valve: case report and review of literature. J Pediatr Urol 2010; 6: 459-462.
[8] Clark TJ, Martin WL, Divakaran TG, Whittle MJ, Kilby MD, Khan KS. Prenatal bladder drainage in the management of fetal lower urinary tract obstruction: a systematic review and metaanalysis. Obstet Gynecol 2003; 102: 367-382.
[9] Morris RK, Malin GL, Khan KS, Kilby MD. Systematic review of the effectiveness of antenatal intervention for the treatment of congenital lower urinary tract obstruction. BJOG 2010; 117: 382-390.
[10] Won HS, Kim SK, Shim JY, Lee PR, Kim A. Vesicoamniotic shunting using a double-basket catheter appears effective in treating fetal bladder outlet obstruction. Acta Obstet Gynecol Scand 2006; 85: 879-884.
[11] Nicolini U, Spelzini F. Invasive assessment of fetal renal abnormalities: urinalysis, fetal blood sampling and biopsy. Prenat Diagn 2001; 21: 964-969.
[12] Tonni G, Ida V, Alessandro V, Bonasoni MP. Prune-belly syndrome: case series and review of the literature regarding early prenatal diagnosis, epidemiology, genetic factors, treatment, and prognosis. Fetal Pediatr Pathol 2013; 31: 13-24.
[13] Livingston JC, Malik KM, Crombleholme TM, Lim FY, Sibai BM. Mirror syndrome: a novel approach to therapy with fetal peritoneal-amniotic shunt. Obstet Gynecol 2007; 110: 540-543.
[14] Farrugia MK, Godley ML, Woolf AS, Peebles DM, Cuckow PM, Fry CH. Experimental short-term partial fetal bladder outflow obstruction: II. Compliance and contractility associated with urinary flow impairment. J Pediatr Urol 2006; 2: 254-260.
ment heading
10.1016/S2221-6189(14)60071-8
*Corresponding author: Dr. Anıl Içel Saygı, M.D., Ankara Millitary Hospital, Department of Obstetrics and Gynecology, Ankara 06100, Turkey.
Tel: +90 506 357 47 96
Fax: +90 312 464 32 32
E-mail: dr_icelanil@hotmail.com
 Journal of Acute Disease2014年4期
Journal of Acute Disease2014年4期
- Journal of Acute Disease的其它文章
- The acute effect of the antioxidant drug “U-74389G” on red blood cells levels during hypoxia reoxygenation injury in rats
- Different profiles of mental and physical health and stress hormone response in women victims of intimate partner violence
- Time-critical AMI Detection: A novel and fast technique using the 12-lead ECG
- Epidemiological survey on scorpionism in Gotvand County, Southwestern Iran: an analysis of 1 067 patients
- Treating and management in acute Laugier's fracture: a case report
- Simvastatin-induced Toxic Epidermal Necrolysis
