Virtual reality interface devices in the reorganization of neural networks in the brain of patients with neurological diseases
Valeska Gatica-Rojas, Guillermo Méndez-Rebolledo
1 Laboratory of Human Motor Control, Faculty of Health Sciences, University of Talca, Talca, Chile
2 Laboratory of Human Motor Control, School of Kinesiology, Faculty of Health Sciences, University of Talca, Talca, Chile
Virtual reality interface devices in the reorganization of neural networks in the brain of patients with neurological diseases
Valeska Gatica-Rojas1, Guillermo Méndez-Rebolledo2
1 Laboratory of Human Motor Control, Faculty of Health Sciences, University of Talca, Talca, Chile
2 Laboratory of Human Motor Control, School of Kinesiology, Faculty of Health Sciences, University of Talca, Talca, Chile
Two key characteristics of all virtual reality applications are interaction and immersion. Systemic interaction is achieved through a variety of multisensory channels (hearing, sight, touch, and smell), permitting the user to interact with the virtual world in real time. Immersion is the degree to which a person can feel wrapped in the virtual world through a de fi ned interface. Virtual reality interface devices such as the Nintendo® Wii and its peripheral nunchuks-balance board, head mounted displays and joystick allow interaction and immersion in unreal environments created from computer software. Virtual environments are highly interactive, generating great activation of visual, vestibular and proprioceptive systems during the execution of a video game. In addition, they are entertaining and safe for the user. Recently, incorporating therapeutic purposes in virtual reality interface devices has allowed them to be used for the rehabilitation of neurological patients, e.g., balance training in older adults and dynamic stability in healthy participants. The improvements observed in neurological diseases (chronic stroke and cerebral palsy) have been shown by changes in the reorganization of neural networks in patients’ brain, along with better hand function and other skills, contributing to their quality of life. The data generated by such studies could substantially contribute to physical rehabilitation strategies.
nerve regeneration; virtual reality; virtual environment; virtual reality exposure therapy; rehabilitation; stroke; postural balance; cerebral palsy; aged; review; nintendo wii balance board; neural regeneration
Funding: This study was financially supported by the National Fund for Health Research and Development (FONIS) of the National Commission for Scientific and Technological Research (CONICYT), No. Sa11i2018, and a grant from Research Department of the University of Talca.
Gatica-Rojas V, Méndez-Rebolledo G. Virtual reality interface devices in the reorganization of neural networks in the brain of patients with neurological diseases. Neural Regen Res. 2014;9(8):888-896.
Introduction
The recent successful integration of virtual reality into the fi eld of medicine and rehabilitation shows the technological potential to permit patients to face a challenging environment, is safe and ecologically accepted, and allows the maintainance of experimental control over the integrated stimuli. Virtual reality interface devices have expanded to the areas of entertainment, military defense (Armstrong et al., 2013), fi tness (Lotan et al., 2009), medicine and rehabilitation, using virtual reality equipment according to the needs of the target group (Isaacson et al., 2013; Nica et al., 2013; Tatla et al., 2013; Tunik et al., 2013; Vermetten et al., 2013). Physical therapies using virtual environments in patients post-stroke (August et al., 2006; Cameirão et al., 2010, 2012; Prochnow et al., 2013) and in patients with cerebral palsy (Li et al., 2009; Golomb et al., 2010) have improved functional and physical abilities; these changes are consistent with observed neuronal reorganization in the brains of these patients.
Nonetheless, there remain problems linked to the usage of this technology exist, speci fi cally with video gaming consoles such as the Nintendo® Wii, Sony PlayStation 2, and EyeToy, because these applications were initially designed for entertainment purposes and have been subsequently adapted for rehabilitation use (Flynn et al., 2007; Lange et al., 2010). Because they were designed for entertainment or amusement purposes, interfaces and software that require high performance on cognitive and motor tests and high levels of dif fi culty can present an obstacle to the patient or hinder the patient’s rehabilitation by erroneously maximizing sensory output and generating abnormal mobility patterns, amongst other consequences. Because of these problems, researchers are developing games designed speci fi cally for rehabilitation systems.
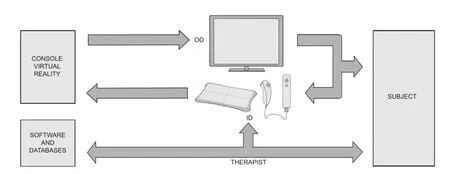
Figure 1 Structure of a virtual reality device.
Moreover, it would be helpful to know the therapeutic applicability of different virtual reality interface devices to common motion characteristics, such as postural balance. Balance can be affected by pathological and nonpathological causes. Pathological causes include the aftermath of a stroke, traumatic brain injury, vestibular disease (unilateral labyrinthine syndrome), and orthopedics (ankle instability), while non-pathological causes include the result of the normal physiological aging process (Lafond et al., 2004; Ioffe et al., 2006; Rocchi et al., 2002, 2006; Lin et al., 2008; Arnold et al., 2009). Current treatment alternatives for balance training are conservative, such as the wobble board (Ogaya et al., 2011; Cloak et al., 2013). These methods can be unsafe for the elderly population and unattractive to the patient’s adherence to treatment.
The objective of this paper is to investigate different virtual reality interface devices and how applicable they are to rehabilitation, e.g., in post-stroke patients and in patients with cerebral palsy. The effects of the virtual reality interface devices used in balance training in musculoskeletal injuries, neurological pathologies and the care of elderly people should be further investigated.
Virtual reality in the rehabilitation: interfaces and design
Several researchers have pointed out three key factors about virtual reality and its application during rehabilitation: (1) Repetition: plasticity is dependent on practice, and causes changes in neural organization in the brain. Repetition improves the learning of motor and functional skills. (2) Sensory feedback: it is widely known that the importance of multisensory stimulation in the rehabilitation of children with cerebral palsy is a global alteration. Maximum development of neural networks can be obtained by working through different channels. Virtual environments provide children with massive and intensive motor-sensory stimulation, which is needed to induce brain restructuring. (3) Individual motivation: this is reached on having focused the different activities that shape the therapy of the subject in a pleasant and appealing way (Holden, 2005; Adamovich et al., 2009; Monge Pereira et al., 2012).
Some authors have de fi ned virtual reality as computerized technology that provides artificial sensory feedback, in the sense that the user obtains experiences that are similar to activities and events that take place in real life (Snider et al., 2010; Monge Pereira et al., 2012). That is, users experience motor learning in three dimensions, which corresponds to a movement performed in the real world (Cano de la Cuerda et al., 2010; Snider et al., 2010). Within the scope of this de finition, highly technological interfaces have the power to generate virtual environments and mediate interaction with the user (Laver et al., 2011). The hardware, such as the central processing unit, monitor, keyboards, mouse, and joystick, allows the construction of a virtual environment. However, for the environment’s generation and implementation, the presence of one or several pieces of software is required. These software products can be defined as the logical media that enable the creation of speci fi c tasks, allowing an interface or connection with the user.
In a virtual reality interface, the user is connected to the system as a part of an input/output loop, allowing individuals to provide inputs to the virtual environment and experiment as a result of that input (Lange et al., 2010). Virtual reality systems offer a simulated environment that allows the user to have a real-time interaction through a computer. To locate the user inside a real-time loop simulation, virtual reality systems require an output or visual interface (Head Mounted Display or flat screen), input interfaces for interaction (mouse, joystick or wired gloves) and tracking devices. The software or virtual environment can be seen through the output interface, and this can be manipulated through input interfaces. Figure 1 shows the components of a virtual reality system.
Fitzgerald et al. (2008) used a conventional computer and Nintendo® Wii Fit Balance Board to carry out exercises that could reduce postural instability, improve balance, and facilitate better weight distribution. These games were developed using a process called User-Centered design, incorporating feedback from those who are most concerned (therapists,patient and caregivers) into the development process, as well as in the re fi nement of the product. The Rehabilitation Gaming System has been designed as a fl exible, virtual reality-based device for rehabilitation, especially for neurological patients (Prochnow et al., 2013; Orihuela-Espina et al., 2013). The Rehabilitation Gaming System is used frequently in the rehabilitation of motor deficits after damage to the brain such as stroke. Moreover, the virtual reality-based device is a novel neurorehabilitation approach since it is associated with the mirror neuron system (Prochnow et al., 2013; August et al., 2006) and motor intention that can be used for visuomotor training (Prochnow et al., 2013). The model of visuomotor training was demonstrated in eighteen healthy right-handed volunteers from the analysis of functional magnetic resonance imaging that showed extensive activity in frontal, parietal, temporal, cingulate and cerebellar areas (Prochnow et al., 2013).
Lange et al. (2010) have pointed out that there are different stages in user-centered game design. The process commences with interviews with those concerned, and observational studies about the game’s activities. The interviews consist of collecting information (experience, details and qualitative data) through user-friendly qualitative questionnaires. The observational studies are a kind of game testing, used to identify processes involved in the game’s activity. The following phases include brainstorming and the suggestion of game ideas. Brainstorming ideas for the development of the game use all of the information collected in previous stages and define the main problem of the game. Once the most appropriate idea is selected, a game prototype is built and the game testing cycle begins. After this cycle has reached an end, the game can be developed in a planned format and can be trial-tested on a larger scale to determine if (1) the game is fun, (2) the graphics are appropriate and entertaining, (3) the game is appealing, and, maybe more importantly, (4) the game carries out the goals of the required therapy.
Classi fi cation of virtual reality interfaces
There are several ways to classify virtual reality. One of them is related to the speci fi c patient population. Thus, numerous types of rehabilitation can be distinguished, like musculoskeletal virtual rehabilitation (orthopedic), post-stroke virtual rehabilitation, and virtual cognitive rehabilitation (Burdea, 2003). Another way to label virtual rehabilitation is linked to the rehabilitation protocol. Here we can distinguish virtual reality-augmented rehabilitation from virtual reality-based therapy. With regard to the fi rst, the patient undergoes treatment consisting of conventional exercises executed on equipment available in the clinic or at home, as well as a regime of simulated virtual rehabilitation exercises. In the second case, the conventional exercises are completely eliminated and a new approach is adopted where virtual rehabilitation is the means by which the patient achieves recovery. However, we do believe that the classi fi cation suggested by Wang and Reid (2011) is the most appropriate. They indicate three types of screen interfaces that can be classi fi ed according the type of interaction between an individual and a computer: (1) feedback-centered interaction, (2) gesture-based interaction, and (3) haptic stimuli-based interaction.
Feedback-centered interaction
This virtual reality modality is based on the delivery of reinforcement or feedback to the base or conventional therapy of the patient. This type of human-computer interaction is typically one-dimensional and it only varies quantitatively. An example of this is electroencephalography used as feedback. This process uses electrical signals produced by the active brain, which can be tracked, monitored, and measured through the external positioning of electrodes on the scalp of the individual. The patterns of the electroencephalographic signals indicate the excitation levels of the brain as well as the diverse areas of activation. For example, for children who suffer from Attention Deficit Hyperactivity Disorder, electroencephalographic patterns are used to control or level cerebral excitement, given that they compare normal and abnormal patterns through monitors, producing feedback that is used to regulate cerebral activity and neural reorganization (Gorrindo and Groves, 2009; Bioulac et al., 2012). The use of virtual reality integrated into the rehabilitation of lower limbs on children with cerebral palsy has also been examined. A screen with a two-dimensional fantasy world in front of a treadmill was used with the purpose of promoting treadmill training (Kott et al., 2009). In a similar fashion, post-stroke patients were trained in front of a screen that represents a virtual environment. These patients improved their weight distribution from one hemibody to another during treadmill training with a partial body weight-supported interface (Walker et al., 2010).
Gesture-based interaction
This system includes specialized cameras to capture points of reference of a target (for example, the human body) during several motions. Then, in real time, the captured image is projected to facilitate the interaction between the target and the virtual environment. According to Wang and Reid (2011), there are two available basic systems with these capacities: those designed specifically for rehabilitation purposes and those designed primarily to entertain. All of these motion capture systems allow users to look at themselves in the virtual environment while they perform activities. These types of virtual reality systems have been used in patients with spinal cord injury (Kizony et al., 2005) and cerebral palsy (Li et al., 2009), and in post-stroke patients (Flynn et al., 2007). The evidence indicates that virtual reality-based gesture therapy in stroke survivors promotes neural reorganization in the motor cortex, prefrontal cortex and cerebellum, especially in patients with greater impairment (Orihuela-Espina et al., 2013). However, a key challenge in neurorehabilitation is to establish optimal training protocols for the given patient.
One clear example of gesture-based interaction is the use of the Nintendo® Wii and its Peripheral Nunchuks-Balance Board, which allows the user to participate in baseball, tennis, and football matches, just to name a few. Nevertheless, as stated before, these interfaces and their software products have been designed for entertainment functions, so their use in rehabilitation must be exhaustively investigated and subsequent-ly validated with regard to people with diverse dysfunctions.
Haptic stimuli-based interaction
This type of virtual reality system is characterized by using haptic stimuli as well as a virtual environment. In other words, haptic interfaces enable the user to perceive mechanic stimuli inside a virtual environment. In this way, besides visual (pictures of items, places, people), vestibular (environments that change their position or orientation from the user’s perspective) or olfactory feedback, these interfaces include somatosensory (mechanical) feedback, granting a larger amount of input interrelated to the user’s central nervous system. Traditional haptic interfaces comprise different types of devices, from a classic computer mouse to a touchscreen. Over the last few years, complex haptic systems including sensory gloves and haptic roboticic systems for the lower and upper limbs have been developed. The Center for Advanced Information Processing, Rutgers, along with staff from the State University of New Jersey, designed the Rutgers Master II-ND glove, which is a haptic interface allowing the interaction of the hand of the user inside a virtual environment (Bouzit et al., 2002). This interface allows the user to move all their fi ngers independently and provides force feedback of up to 16 N. In this way, the user experiences typical virtual reality feedback combined with somatosensory stimuli in real time.
Virtual reality interface devices used in balance training
Balance training has been prescribed by therapists for a series of medical conditions, such as musculoskeletal injuries (Howells et al., 2013), neurological pathologies (Hill et al., 2009; Kim and Park, 2013), and the care of elderly people (Flynn et al., 2007; Seco et al., 2013). Rehabilitation programs include activities and/or the use of interfaces that challenge patients’ balance, by incorporating sensory information (visual, vestibular, and somatosensory) and integrating it into the central nervous system in relation to the generation of coordinated movement patterns. When there is a deterioration of this motor skill, a balance de fi cit is presented; in other words, the loss of the participant’s ability to maintain the center of mass relative to the base of support.
Many virtual reality devices have been used in rehabilitation, e.g., in patients with attention de fi cit hyperactivity disorder and improving the function of the hand or upper limb in hemiplegic patients (Figure 2A, C) and balance training in subjects with neurological disorders (Parkinson’s disease, post- stroke, cerebral palsy) or older adults with loss of balance and normal individuals (Figure 2B, D).
Balance near automatic virtual environment
This is an immersive system with stereoscopic images in which the virtual environment is projected all over the patient’s visual field, placed on a dynamometric platform in the center of the “virtual room”. Patients were put into groups according to the presence or absence of vestibular malfunction, and watched scenes in motion. Motion in the patients’ head, pressure center and electromyographic register is recorded. Both groups responded to visual stimuli with substantial increases in their head motion and body balance in synchrony with these stimuli (Whitney et al., 2002), confi rming the effect of visual stimuli provided by virtual reality systems. However, the use of these interfaces may allow a graduated immersion of the patient into visual stimuli, hence making balance training easier.
Cave automatic virtual environment
This is regarded as an immersive virtual reality environment that is known for its high resolution with three-dimensional video and audio features, fi tted to a fl oored space with three walls (one frontal wall and two lateral ones). It is used in the study of the organization of dynamic postural responses in normal individuals, establishing that the controllers of posture in the nervous system can establish motion boundaries in each segment of the body instead of being guided solely by visual vertical perception (Keshner and Kenyon, 2000; Holden, 2005) (Figure 2C).
Head mounted displays
These offer images in the highest possible resolution because of their proximity to the eye. They consist of one monocular or binocular device, and since they are placed on the head of the user, they can follow the user’s movements, making them feel integrated into the environment created by the computer (Monge Pereira et al., 2012). However, they have drawn much criticism because they generally restrict movement, are heavy, provoke nausea, give a limited visual fi eld, and are uncomfortable. Nonetheless, Milhalik et al. (2008) carried out a study where they tested whether the weight of a head mounted display (HMD) interface influences performance on balance tests. They observed that the balance of the individuals using HMD was not affected by this interface. However, the researchers indicated that patients perceived some degree of apprehension towards the HMD interface, as they could not visualize parts of their body (e.g., feet) when looking down at the fl oor.
Computer assisted rehabilitation environment
This is virtual reality software that has been used in treadmill training with post-stroke patients. It is known for being a mixed system because it incorporates virtual reality, detects disturbances on the walking surface through a modified treadmill, and has a bar used as a haptic interface for the fi ngers of the patient (Fung and Perez, 2011). This haptic interface has become an ef fi cient and innovative way to enhance postural control and dynamic stability. It combines a display screen with the manipulation of physical environment along with haptic feedback to improve equilibrium and mobility after a stroke.
Nintendo® Wii and peripheral nunchuks-balance board
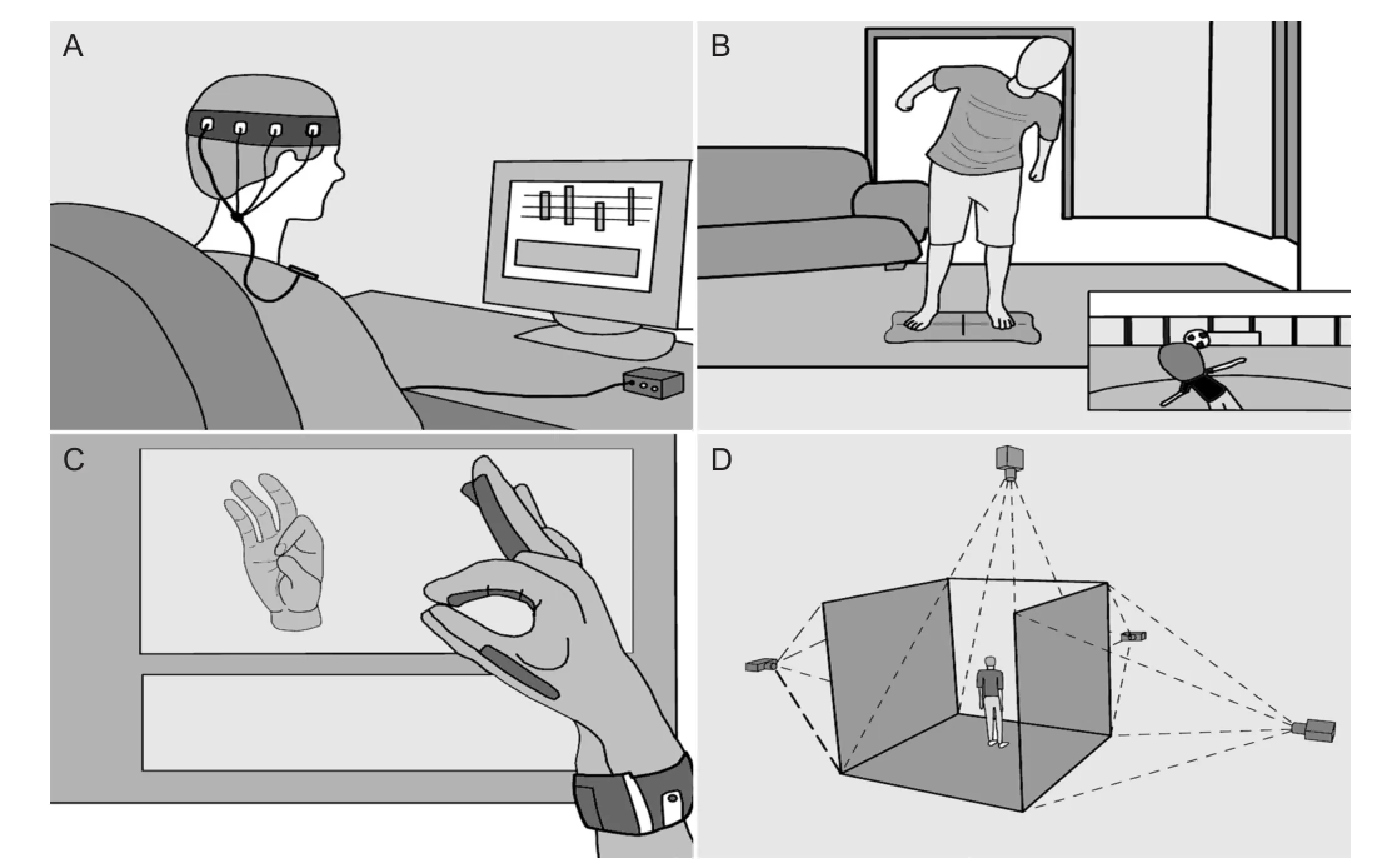
Figure 2 Virtual reality devices used in rehabilitation and training.
This video game console, originally designed for entertainment purposes, has been used in much therapy-driven research. The player is represented by an avatar in the virtual environment, which is controlled by a peripheral interface (Nunchuk) that the user has to hold in their hand. The software measures the movements of the player and these are transferred to the screen; this remote control detects changes in acceleration and orientation, and the system adjusts feedback according to these parameters. The peripheral device provides haptic feedback; games offer not only plentiful visual and auditory feedback, but also the opportunity to include more players with different dif fi culty levels. Nevertheless, the Wii Balance Board is the most used peripheral interface when it comes to therapeutic purposes related to balance. Along with the Nintendo® Wii Fit game, it allows the user to train the displacement of the pressure center in the support base (Lange et al., 2010). The Balance Board consists of four load cells distributed in each of its four corners, which is similar to how force platform posturography, created to evaluate and measure balance in a quantitative form, works (Lange et al., 2010; see Figure 2B).
Sony® PlayStation 2 Eye Toy
This is based on the capture of the user’s motion that is represented in a virtual environment. In this way, the patient constantly interacts with the challenges imposed by video games. Flynn et al. (2007) carried out a case study of a poststroke patient who underwent a rehabilitation program using the PlayStation 2 Eye Toy. The requirements of the game tests included objective-based movement, balance, and motor planning.
Telerehabilitation
Recent innovation in telerehabilitation systems has allowed post-stroke patients to have access to long-distance rehabilitation services through a remote location (Holden, 2005), eliminating self-formation problems in rehabilitation. Furthermore, it increases the number of motor gestures in diverse functional situations, thus keeping patients from getting bored by a repetitive and monotonous motion. Telerehabilitation systems, in theory, could make motor learning easier thanks to the assistance of the learner’s motor planning system in a natural way; in other words, through imitation learning (Keshner and Kenyon, 2000).
Effects of virtual reality on balance
In recent years, several scienti fi c articles have been published about the effects of virtual reality on balance, measured primarily through scales or clinical trials (Csuka and McCarty, 1885; Duncan et al., 1990; Podsiadlo and Richardson, 1991; Berg et al., 1992; Corry et al., 1996; Boyd et al., 1999; Johnston et al., 2004; Kim et al., 2004; Lafond et al., 2004; Tyson and DeSouza, 2004; Kennedy et al., 2005; van Hedel et al., 2005, 2007; Whitney et al., 2005; Stratford et al., 2006; Hill etal., 2009; Kouzaki and Shinohara, 2010; Kouzaki and Masani, 2012). However, few publications have used technologically objective measurement systems, such as a force platform, to measure the effects of virtual reality. Force platforms provide several measurements that re fl ect postural balance, such as the area, velocity and sway in the anteroposterior and mediolateral directions, based on center of pressure excursion (Kouzaki and Shinohara, 2010; Kouzaki and Masani, 2012). Center of pressure is de fi ned as the location of the vertical ground reaction force vector (Onambele and Narici, 2006). Studies show that loss of balance may occur in healthy people (Podsiadlo and Richardson, 1991; Johnston et al., 2004) as well as patients suffering from neurological disorders, when the displacement of the center of pressure is outside the boundaries of stability.
For non-pathological causes such as the effects of age, the loss of balance in seniors is well known (Kouzaki and Masani, 2012). In fact, postural instability has been identified as the greatest intrinsic factor in falls, which can potentially be in fl uenced by some means of intervention (Tinetti et al., 1988, 1994; Horak et al., 1989; Shumway-Cook et al., 1997; Aruin et al, 1998; Duarte and Zatsiorsky, 2002; Moghadam et al., 2011). In this vein, Bisson et al. (2007) based a study on a quasi-experimental design by forming two study groups consisting of healthy older adults who were not prone to accidental falls. Participants of the virtual reality group used a“juggler” application from a computerized exercise program called IREX. They underwent standing training in front of a monochrome wall to enable a video camera to capture their image in real time, which was sent to a unit for computational processing. The virtual environment was generated using color subtraction software, which first removed the background from the video image allowing for the isolation of the participant’s image, and then incorporated virtual objects. Conversely, the biofeedback group carried out this task in conjunction with a force platform, where a red cursor represented the center of pressure position in real time, providing visual feedback on a monitor in front of the participant. Senior adults in each group attended two 30-minute sessions per week, for a total of 10 consecutive weeks. The results of their study showed that both training groups significantly improved on the Community balance and Mobility Scale, as well showing a decline in reaction times. However, the postural sway in the mediolateral and antero-posterior directions during quiet standing posture with the participants’feet apart, feet together, and a dual task showed no signi fi cant difference between the groups, and training rates did not differ signi fi cantly in terms of center of pressure displacement.
Gatica et al. (2010) improved the measured balance based on area and velocity of the center of pressure in a sample of 20 older adult participants who were not at risk for falls. During quiet stance, these variables dropped significantly, and in tandem the center of pressure decreased greatly. Both changes were observed in the phase when patients were looking straight ahead with their head erect. This quasi-experimental research design (a convenience sample) employed a protocol of 20-minute training sessions, 3 times per week, for a total of 8 consecutive weeks. Evaluations were carried out from the start and at weeks 3, 6 and 8 of training. The virtual reality training protocol employed the use of the Nintendo® Wii and its peripheral Balance Board. The biggest advances with regard to balance were obtained 6 weeks after training.
Balance can also be evaluated using clinical measurements. Clinical scales are meant to measure the functional balance of patients suffering from a clinical condition, like poststroke (or Acquired Brain Injury). These clinical evaluations are classified along scales of functional balance for both static and dynamic conditions. Some easily identi fi able static evaluations are the Berg Balance Scale, the Brunel Balance Assessment and the Anterior Reach Test while some examples of dynamic scales include the Timed Stair Test, the Stepping Test, the 10-Meter Walk Test, the 1-Minute Walking Test, the Time “Up and Go” Test, and the Sit-to Stand Test amongst others (Csuka and McCarty, 1885; Duncan et al., 1990; Podsiadlo and Richardson, 1991; Berg et al., 1992; Corry et al., 1996; Boyd et al., 1999; Johnston et al., 2004; Kim et al., 2004; Tyson and DeSouza, 2004; Kennedy et al., 2005; van Hedel et al., 2005, 2007; Whitney et al., 2005; Stratford et al., 2006; Hill et al., 2009).
Gil-Gómez et al. (2011) recruited 17 hemiparetic patients with acquired brain damage for a single-blinded randomized controlled trial. For balance training, this research team designed the “easy Balance Virtual Rehabilitation” system, which is used to improve balance by providing motivational tasks and orientation exercises designed by physical therapists. The hardware components of the “easy Balance Virtual Rehabilitation” system are based on a conventional computer, a 42-inch LCD screen and a Nintendo® Wii console in addition to its peripheral Balance Board. In this way, the exercises are operated on the computer, and the system uses the Wii Balance Board/easy Balance Virtual Rehabilitation as an interface. The trial group received a total of 20 training sessions (1 hour each session) with a minimum of 3 and a maximum of 5 sessions per week. The control group received the same amount and frequency of treatment, but with conventional exercises aimed at improving balance. The trial group that used the “easy Balance Virtual Rehabilitation” system showed a signi fi cant improvement on static balance tests, such as the Berg Scale and the Functional Reach Test, in contrast to the control group that received traditional treatment. However, no signi fi cant differences between the trial and control groups were found for the measurement of dynamic balance, using the Timed Stair Test, Stepping Test, 10-Meter Walk Test, 1-Minute Walking Test, Time “Up and Go” Test, or Sit-to-Stand Test. However, each study group improved in a similar fashion over time in all measures for dynamic balance, which could mean that each training session independently contributed to dynamic functional balance (Gil-Gómez et al., 2011).
Research on virtual environments has not only been shown to improve balance in pathological conditions, but it has also contributed positively to the functional abilities of patients. For example, Golomb et al. (2010) used telerehabilitation to train three patients with severe hemiplegic cerebral palsy for 3 months. Virtual rehabilitation systems were installed in the homes of patients by means of a video game console connected to a remote monitoring system. Feedback and monitoring were established through a DSL connection with the hospital as well as with the Tele-Rehabilitation Institute, Rutgers University. The patients exercised the affected hand 30 minutes a day, fi ve days a week with a sensor glove placed over the hand and connected to the video gameconsole. The results of this pilot study showed an improvement in hand functional skills (lifting objects and improving range of motion). The functional skills of the affected hand improved and were re fl ected in the changes of neural reorganization in the brain that were observed through functional magnetic resonance imaging (Golomb et al., 2010).
Probable mechanisms of action of virtualreality on balance
Three sensory systems are involved in balance and human posture: vision, vestibular, and somatosensory (mechanoreceptors and proprioceptors). These systems deliver feedback mechanisms that generate an appropriate corrective torque based on how (1) the vestibular sensory cues detect deviations of head orientation from the vertical (gravity), (2) the proprioceptors detect orientation relative to the support surface, and (3) the visual sensors detect head orientation relative to the visual fi eld. In this way, visual receptors, proprioceptors, and mechanoreceptors are the direct route of input entry provided by virtual environments (Peterka, 2002).
Virtual reality interfaces (see previous section) with the objective of training balance provide enriched feedback with visual, vestibular, and somatosensory input. This approach allows the central nervous system to experience plastic phenomena that elicit efficient motor responses to keep the center of body mass inside the support base, thus avoiding falls in elderly people (Schellenbach et al., 2010), improving treadmill patterns (Duque et al., 2013) and maintaining adequate balance (Keshner and Kenyon, 2004; Rendon et al., 2012). Virtual reality can be used in several ways to train postural control and, therefore, the balance of a patient. Adamovich et al. (2009) state that visual feedback is one of the most used sensory inputs in a virtual reality setting, presenting two methods of intervention. First, virtual reality can be used to manipulate visual feedback with the aim of producing con fl icts between somatosensory, vestibular, and visual information, while also permitting the training of different sensory systems (Keshner and Kenyon, 2004). Second, virtual reality feedback can be systematically regulated (in terms of speed and complexity), with the aim of challenging the static and dynamic postural control of an individual in the course of their sensorimotor training.
Moreover, the training of balance is habitually based on the repetition of speci fi ed movements in the sagittal, frontal, and transverse planes, in addition to the integration of force, flexibility, and resistance. Older adults have a significant reduction in the number of falls and in the percentage of these types of events when they commit systematically to this mode of training (Gillespie et al., 2003; Sherrington et al., 2008; Sakurai et al., 2011). In young patients with knee instability, a balance training on a Wobble board significantly improves knee function and reduces the number of recurring incidents (Cloak et al., 2013). In this sense, it is dif fi cult to train signi fi cantly aged populations or those with motor de fi ciency due to acquired cerebral damage on unstable surfaces, which could result in an insecure environment for these people. In addition, many of these therapeutic tasks are based on the repetition of exercises that may affect motivation or patient adherence to treatment. Therefore, virtual reality is an innovative method that manages to attractively incorporate technology, security and therapeutic training objectives proposed by professionals (e.g., physical therapists) to their patients. In contrast to other therapeutic methods that can be tedious, costly, and dull with regard to their repetition in each treatment session, virtual reality can not only improve the balance of patients (Gil-Gómez et al., 2011) (e.g., post stroke) but can also contribute to improving functional tasks because virtual environments allow interactions related to activities of daily living (repetition improves the learning of motor and functional skills, indicated in the previous sections). Sveistrup (2004) notes that motor impairments are improved when using virtual reality technology in the treatment of patients with acquired brain damage.
Conclusion
Virtual reality interface devices represent a good tool for developing therapies that contribute to postural balance and patient motor function. The diversity of virtual reality interface devices initially developed to entertain can be adapted for therapeutic purposes in patients. These adaptations often reduce the economic cost that involves the acquisition of speci fi c software for rehabilitation. Both interaction and immersion in virtual environments constitute the input mechanism of sensory systems (visual, vestibular and kinesthetic) and the central nervous system, adjusting postural control and balance. Future research should incorporate methods of balance measurement that are more accurate and objective (i.e., force platforms). The background information provided in this research could substantially contribute to physical rehabilitation strategies.
Author contributions:Gatica-Rojas V obtained the funding, wrote, and designed the manuscript. Méndez-Rebolledo G wrote the manuscript and developed all figures. Both participated in the critical revision of the manuscript and approved the final version of this paper.
Con fl icts of interest:None declared.
Adamovich SV, Fluet GG, Tunik E, Merians AS (2009) Sensorimotor training in virtual reality: a review. NeuroRehabilitation 25:29-44.
Armstrong CM, Reger GM, Edwards J, Rizzo AA, Courtney CG, Parsons TD (2013) Validity of the Virtual Reality Stroop Task (VRST) in active duty military. J Clin Exp Neuropsychol 35:113-123.
Arnold BL, De La Motte S, Linens S, Ross SE (2009) Ankle instability is associated with balance impairments: a meta-analysis. Med Sci Sports Exerc 41:1048-1062.
Aruin AS, Forrest WR, Latash ML (1998) Anticipatory postural adjustments in conditions of postural instability. Electroencephalogr Clin Neurophysiol 109:350-359.
August K, Lewis JA, Chandar G, Merians A, Biswal B, Adamovich S (2006) FMRI analysis of neural mechanisms underlying rehabilitation in virtual reality: activating secondary motor areas. Conf Proc IEEE Eng Med Biol Soc 1:3692-3695.
Berg KO, Wood-Dauphinee SL, Williams JI, Maki B (1992) Measuring balance in the elderly: validation of an instrument. Can J Public Health 83 Suppl 2:S7-11.
Bioulac S, Lallemand S, Rizzo A, Philip P, Fabrigoule C, Bouvard MP (2012) Impact of time on task on ADHD patient’s performances in a virtual classroom. Eur J Paediatr Neurol 16:514-521.
Bisson E, Contant B, Sveistrup H, Lajoie Y (2007) Functional balance and dual-task reaction times in older adults are improved by virtual reality and biofeedback training. Cyberpsychol Behav 10:16-23.
Bouzit M, Burdea G, Popescu G, Boian R (2002) The rutgers master II-new design force-feedback glove. IEEE/ASME Transactions on Mechatronics 7:256-263.
Boyd R, Fatone S, Rodda J, Olesch C, Starr R, Cullis E, Gallagher D, Carlin JB, Nattrass GR, Graham K (1999) High- or low- technology measurements of energy expenditure in clinical gait analysis? Dev Med Child Neurol 41:676-682.
Burdea GC (2003) Virtual rehabilitation--benefits and challenges. Methods Inf Med 42:519-523.
Cameirão MS, Badia SB, Oller ED, Verschure PF (2010) Neurorehabilitation using the virtual reality based Rehabilitation Gaming System: methodology, design, psychometrics, usability and validation. J Neuroeng Rehabil 7:48.
Cameirão MS, Badia SB, Duarte E, Frisoli A, Verschure PF (2012) The combined impact of virtual reality neurorehabilitation and its interfaces on upper extremity functional recovery in patients with chronic stroke. Stroke 43:2720-2728.
Cano de la Cuerda R, Muñoz-Hellín E, Alguacil-Diego IM, Molina-Rueda F (2010) Telerehabilitation and neurology. Rev Neurol 51:49-56.
Cloak R, Nevill A, Day S, Wyon M (2013) Six-week combined vibration and wobble board training on balance and stability in footballers with functional ankle instability. Clin J Sport Med 23:384-391.
Corry IS, Duffy CM, Cosgrave AP, Graham HK (1996) Measurement of oxygen consumption in disabled children by the Cosmed K2 portable telemetry system. Dev Med Child Neurol 38:585-593.
Csuka M, McCarty DJ (1885) Simple method for measurement of lower extremity muscle strength. Am J Med 78:77-81.
Duarte M, Zatsiorsky VM (2002) Effects of body lean and visual information on the equilibrium maintenance during stance. Exp Brain Res 146:60-69.
Duncan PW, Weiner DK, Chandler J, Studenski S (1990) Functional reach: a new clinical measure of balance. J Gerontol 45:M192-197.
Duque G, Boersma D, Loza-Diaz G, Hassan S, Suarez H, Geisinger D, Suriyaarachchi P, Sharma A, Demontiero O (2013) Effects of balance training using a virtual-reality system in older fallers. Clin Interv Aging 8:257-263.
Fitzgerald D, Trakarnratanakul N, Dunne L, Smyth B, Caulfield B (2008) Development and user evaluation of a virtual rehabilitation system for wobble board balance training. Conf Proc IEEE Eng Med Biol Soc 2008:4194-4198.
Flynn S, Palma P, Bender A (2007) Feasibility of using the Sony PlayStation 2 gaming platform for an individual poststroke: a case report. J Neurol Phys Ther 31:180-189.
Fung J, Perez CF (2011) Sensorimotor enhancement with a mixed reality system for balance and mobility rehabilitation. Conf Proc IEEE Eng Med Biol Soc 2011:6753-6757.
Gatica RV, Elgueta CE, Vidal SC, Cantin ML, Fuentealba JA (2010) Impacto del entrenamiento del balance a través de realidad virtual en una población de adultos mayores. Int J Morphol 28:303-308.
Gil-Gómez JA, Lloréns R, Alcañiz M, Colomer C (2011) Effectiveness of a Wii balance board-based system (eBaViR) for balance rehabilitation: a pilot randomized clinical trial in patients with acquired brain injury. J Neuroeng Rehabil 8:30.
Gillespie LD, Gillespie WJ, Robertson MC, Lamb SE, Cumming RG, Rowe BH (2003) Interventions for preventing falls in elderly people. Cochrane Database Syst Rev (4):CD000340.
Golomb MR, McDonald BC, Warden SJ, Yonkman J, Saykin AJ, Shirley B, Huber M, Rabin B, Abdelbaky M, Nwosu ME, Barkat-Masih M, Burdea GC (2010) In-home virtual reality videogame telerehabilitation in adolescents with hemiplegic cerebral palsy. Arch Phys Med Rehabil 91:1-8.e1.
Gorrindo T, Groves JE (2009) Computer simulation and virtual reality in the diagnosis and treatment of psychiatric disorders. Acad Psychiatry 33:413-417.
Hill KD, LoGiudice D, Lautenschlager NT, Said CM, Dodd KJ, Suttanon P (2009) Effectiveness of balance training exercise in people with mild to moderate severity Alzheimer’s disease: protocol for a randomised trial. BMC Geriatr 9:29.
Holden MK (2005) Virtual environments for motor rehabilitation: review. Cyberpsychol Behav 8:187-211.
Holden MK, Dyar TA, Dayan-Cimadoro L (2007) Telerehabilitation using a virtual environment improves upper extremity function in patients with stroke. IEEE Trans Neural Syst Rehabil Eng 15: 36-42.
Horak FB, Shupert CL, Mirka A (1989) Components of postural dyscontrol in the elderly: a review. Neurobiol Aging 10:727-738.
Howells BE, Clark RA, Ardern CL, Bryant AL, Feller JA, Whitehead TS, Webster KE (2013) The assessment of postural control and the in fl uence of a secondary task in people with anterior cruciate ligament reconstructed knees using a Nintendo Wii Balance Board. Br J Sports Med 47:914-919.
Ioffe ME, Ustinova KI, Chernikova LA, Kulikov MA (2006) Supervised learning of postural tasks in patients with poststroke hemiparesis, Parkinson’s disease or cerebellar ataxia. Exp Brain Res 168:384-394.
Isaacson BM, Swanson TM, Pasquina PF (2013) The use of a computer-assisted research environment (CAREN) for enhancing wounded warrior rehabilitation regimens. J Spinal Cord Med 36:296-299.
Johnston TE, Moore SE, Quinn LT, Smith BT (2004) Energy cost of walking in children with cerebral palsy: relation to the Gross Motor Function Classi fi cation System. Dev Med Child Neurol 46:34-38.
Kennedy DM, Stratford PW, Wessel J, Gollish JD, Penney D (2005) Assessing stability and change of four performance measures: a longitudinal study evaluating outcome following total hip and knee arthroplasty. BMC Musculoskelet Disord 6:3.
Keshner EA, Kenyon RV (2000) The in fl uence of an immersive virtual environment on the segmental organization of postural stabilizing responses. J Vestib Res 10:207-219.
Keshner EA, Kenyon RV (2004) Using immersive technology for postural research and rehabilitation. Assist Technol 16:54-62.
Kim CM, Eng JJ, Whittaker MW (2004) Level walking and ambulatory capacity in persons with incomplete spinal cord injury: relationship with muscle strength. Spinal Cord 42:156-162.
Kim JH, Park EY (2013) Balance self-ef fi cacy in relation to balance and activities of daily living in community residents with stroke. Disabil Rehabil doi: 10.3109/09638288.2013.790488.
Kizony R, Raz L, Katz N, Weingarden H, Weiss PL (2005) Video-capture virtual reality system for patients with paraplegic spinal cord injury. J Rehabil Res Dev 42:595-608.
Kott KM, Lesher K, DeLeo G (2009) Combining a virtual reality system with treadmill training for children with cerebral palsy. J Cyber Ther Rehabil 2:35-42.
Kouzaki M, Masani K (2012) Postural sway during quiet standing is related to physiological tremor and muscle volume in young and elderly adults. Gait Posture 35:11-17.
Kouzaki M, Shinohara M (2010) Steadiness in plantar fl exor muscles and its relation to postural sway in young and elderly adults. Muscle Nerve 42:78-87.
Lafond D, Corriveau H, Hébert R, Prince F (2004) Intrasession reliability of center of pressure measures of postural steadiness in healthy elderly people. Arch Phys Med Rehabil 85:896-901.
Lange B, Flynn S, Proffitt R, Chang CY, Rizzo AS (2010) Development of an interactive game-based rehabilitation tool for dynamic balance training. Top Stroke Rehabil 17:345-352.
Lange BS, Requejo P, Flynn SM, Rizzo AA, Valero-Cuevas FJ, Baker L, Winstein C (2010) The potential of virtual reality and gaming to assist successful aging with disability. Phys Med Rehabil Clin N Am 21:339-356.
Laver KE, George S, Thomas S, Deutsch JE, Crotty M (2011) Virtual reality for stroke rehabilitation. Cochrane Database Syst Rev (9):CD008349.
Li W, Lam-Damji S, Chau T, Fehlings D (2009) The development of a home-based virtual reality therapy system to promote upper extremity movement for children with hemiplegic cerebral palsy. Technol Disabil 21:107-113.
Lin D, Seol H, Nussbaum MA, Madigan ML (2008) Reliability of COP-based postural sway measures and age-related differences. Gait Posture 28:337-342.
Lotan M, Yalon-Chamovitz S, Weiss PL (2009) Improving physical fi tness of individuals with intellectual and developmental disability through a Virtual Reality Intervention Program. Res Dev Disabil 30:229-239.
Mihalik JP, Kohli L, Whitton MC (2008) Do the physical characteristics of a virtual reality device contraindicate its use for balance assessment?. J Sport Rehabil 17:38-49.
Moghadam M, Ashayeri H, Salavati M, Sarafzadeh J, Taghipoor KD, Saeedi A, Salehi R (2011) Reliability of center of pressure measures of postural stability in healthy older adults: effects of postural task dif fi culty and cognitive load. Gait Posture 33:651-655.
Monge Pereira E, Molina Rueda F, Alguacil Diego IM, Cano De La Cuerda R, De Mauro A, Miangolarra Page JC (2012) Use of virtual reality systems as proprioception method in cerebral palsy: clinical practice guideline. Neurologia (in press)
Nica AS, Brailescu CM, Scarlet RG (2013) Virtual reality as a method for evaluation and therapy after traumatic hand surgery. Stud Health Technol Inform 191:48-52.
Ogaya S, Ikezoe T, Soda N, Ichihashi N (2011) Effects of balance training using wobble boards in the elderly. J Strength Cond Res 25:2616-2622.
Onambele GL, Narici MV, Maganaris CN (2006) Calf muscle-tendon properties and postural balance in old age. J Appl Physiol 100:2048-2056.
Orihuela-Espina F, Fernández del Castillo I, Palafox L, Pasaye E, Sánchez-Villavicencio I, Leder R, Franco JH, Sucar LE (2013) Neural reorganization accompanying upper limb motor rehabilitation from stroke with virtual reality-based gesture therapy. Top Stroke Rehabil 20:197-209.
Peterka RJ (2002) Sensorimotor integration in human postural control. J Neurophysiol 88:1097-1118.
Podsiadlo D, Richardson S (1991) The time “up & go”: a test of basic functional mobility for frail elderly persons. J Am Geriatr Soc 39:142-148.
Prochnow D, Bermúdez i Badia S, Schmidt J, Duff A, Brunheim S, Kleiser R, Seitz RJ, Verschure PF (2013) A functional magnetic resonance imaging study of visuomotor processing in a virtual reality-based paradigm: Rehabilitation Gaming System. Eur J Neurosci 37:1441-1447.
Rendon AA, Lohman EB, Thorpe D, Johnson EG, Medina E, Bradley B (2012) The effect of virtual reality gaming on dynamic balance in older adults. Age Ageing 41:549-552.
Rocchi L, Chiari L, Horak FB (2002) Effects of deep brain stimulation and levodopa on postural sway in Parkinson’s disease. J Neurol Neurosurg Psychiatry 73:267-274.
Rocchi L, Chiari L, Cappello A, Horak FB (2006) Identification of distinct characteristics of postural sway in Parkinson’s disease: a feature selection procedure based on principal component analysis. Neurosci Lett 394:140-145.
Sakurai R, Fujiwara Y, Kim H, Saito K, Yasunaga M, Nonaka K, Kobayashi K, Ogawa K, Yoshida H, Tanaka C, Uchida H, Suzuki K, Watanabe S, Shinkai S (2011) A randomized controlled trial of the effects of a comprehensive intervention program for community-dwelling older adults. Nihon Ronen Igakkai Zasshi 48:352-360.
Schellenbach M, Lövdén M, Verrel J, Krüger A, Lindenberger U (2010) Adult age differences in familiarization to treadmill walking within virtual environments. Gait Posture 31:295-299.
Seco J, Abecia LC, Echevarría E, Barbero I, Torres-Unda J, Rodriguez V, Calvo JI (2013) A long-term physical activity training program increases strength and flexibility, and improves balance in older adults. Rehabil Nurs 38:37-47.
Sherrington C, Whitney JC, Lord SR, Herbert RD, Cumming RG, Close JC (2008) Effective exercise for the prevention of falls: a systematic review and meta-analysis. J Am Geriatr Soc 56:2234-2243.
Shumway-Cook A, Baldwin M, Polissar NL, Gruber W (1997) Predicting the probability for falls in community-dwelling older adults. Phys Ther 77:812-819.
Singh DK, Rajaratnam BS, Palaniswamy V, Pearson H, Raman VP, Bong PS (2012) Participating in a virtual reality balance exercise program can reduce risk and fear of falls. Maturitas 73:239-243.
Snider L, Majnemer A, Darsaklis V (2010) Virtual reality as a therapeutic modality for children with cerebral palsy. Dev Neurorehabil 13:120-128.
Stratford PW, Kennedy DM, Woodhouse LJ (2006) Performance measures provide assessments of pain and function in people with advanced osteoarthritis of the hip or knee. Phys Ther 86:1489-1496. Sveistrup H (2004) Motor rehabilitation using virtual reality. J Neuroeng Rehabil 1:10.
Tatla SK, Sauve K, Virji-Babul N, Holsti L, Butler C, Van Der Loos HF (2013) Evidence for outcomes of motivational rehabilitation interventions for children and adolescents with cerebral palsy: an American Academy for Cerebral Palsy and Developmental Medicine systematic review. Dev Med Child Neurol 55:593-601.
Tinetti ME, Speechley M, Ginter SF (1988) Risk factors for falls among elderly persons living in the community. N Engl J Med 319:1701-1707.
Tinetti ME, Baker DI, McAvay G, Claus EB, Garrett P, Gottschalk M, Koch ML, Trainor K, Horwitz RI (1994) A multifactorial intervention to reduce the risk of falling among elderly people living in the community. N Engl J Med 331:821-827.
Tunik E, Saleh S, Adamovich SV (2012) Visuomotor discordance during visually-guided hand movement in virtual reality modulates sensorimotor cortical activity in healthy and hemiparetic subjects. IEEE Trans Neural Syst Rehabil Eng 21:198-207.
Tyson SF, DeSouza LH (2004) Development of the Brunel Balance Assessment: a new measure of balance disability post stroke. Clin Rehabil 18:801-810.
van Hedel HJ, Wirth B, Dietz V (2005) Limits of locomotor ability in subjects with a spinal cord injury. Spinal Cord 43:593-603.
van Hedel HJ, Dietz V, Curt A (2007) Assessment of walking speed and distance in subjects with an incomplete spinal cord injury. Neurorehabil Neural Repair 21:295-301.
Vermetten E, Meijer L, van der Wurff P, Mert A (2013) The effect of military motion-assisted memory desensitization and reprocessing treatment on the symptoms of combat-related post traumatic stress disorder: fi rst preliminary results. Stud Health Technol Inform 191:125-127.
Walker ML, Ringleb SI, Maihafer GC, Walker R, Crouch JR, Van Lunen B, Morrison S (2010) Virtual reality-enhanced partial body weight-supported treadmill training poststroke: feasibility and effectiveness in 6 subjects. Arch Phys Med Rehabil 91:115-122.
Wang M, Reid D (2011) Virtual reality in pediatric neurorehabilitation: attention de fi cit hyperactivity disorder, autism and cerebral palsy. Neuroepidemiology 36:2-18.
Whitney SL, Sparto PJ, Brown KE, Furman JM, Jacobson JL, Redfern MS (2002) The potential use of virtual reality in vestibular rehabilitation: preliminary fi ndings with the BNAVE. Neurol Rep 26:72-78.
Whitney SL, Wrisley DM, Marchetti GF, Gee MA, Redfern MS, Furman JM (2005) Clinical measurement of sit-to-stand performance in people with balance disorders: validity of data for the Five-Times-Sit-to-Stand Test. Phys Ther 85:1034-1045.
Copyedited by Jackson C, Robens J, Armstrong C, Li CH, Song LP, Zhao M
10.4103/1673-5374.131612 http://www.nrronline.org/
Valeska Gatica-Rojas, Ph.D., Laboratory of Human Motor Control, Faculty of Health Sciences, University of Talca, Talca, Chile, vgatica@utalca.cl.
Accepted: 2014-01-21
- 中国神经再生研究(英文版)的其它文章
- Similar effects of substance P on learning and memory function between hippocampus and striatal marginal division
- Apoptosis is an obstacle to the differentiation of adipose-derived stromal cells into astrocytes
- Citalopram increases the differentiation ef fi cacy of bone marrow mesenchymal stem cells into neuronal-like cells
- Fusion protein of single-chain variable domain fragments for treatment of myasthenia gravis
- Nasal mucosal inhalation of amyloid-beta peptide 3-10 defective adenovirus attenuates cytotoxicity induced by beta-amyloid (1-42)
- Regulatory effects of anandamide on intracellular Ca2+concentration increase in trigeminal ganglion neurons

