18F-FDG PET/CT显像偶发甲状腺癌的葡萄糖代谢与临床病理学的相关性研究
李雪娜,尹雅芙,杜补林,李亚明中国医科大学附属第一医院核医学科,辽宁 沈阳 110001
18F-FDG PET/CT显像偶发甲状腺癌的葡萄糖代谢与临床病理学的相关性研究
李雪娜,尹雅芙,杜补林,李亚明
中国医科大学附属第一医院核医学科,辽宁 沈阳 110001
[摘要]背景与目的:18F-FDG PET/CT的广泛应用导致偶发甲状腺癌的比例明显增加,偶发甲状腺癌灶的糖代谢与甲状腺癌病理学的相关性尚不清楚。研究因非甲状腺疾病行18F-FDG PET/CT显像、偶发甲状腺癌的患者,分析甲状腺癌灶的糖代谢与肿瘤的分化程度、淋巴结转移的相关性。方法:回顾性分析18F-FDG PET/ CT显像偶发甲状腺瘤患者195例,53例患者手术病理诊断为甲状腺癌。分别测量甲状腺癌灶的最大标准摄取值(SUVmax)、病变大小、病变个数,同时测量患者正常甲状腺组织的SUVmax。通过病理分析病理学分型、淋巴结转移,患者分为G1组(分化型甲状腺癌)、G2组(非分化型甲状腺癌)、G3组(甲状腺癌无淋巴结转移)和G4组(甲状腺癌有淋巴结转移)。分析G1组与G2组、G3组与G4组间甲状腺癌灶的糖代谢的差异。结果:53例患者中,PET显像发现甲状腺癌灶53个。病理学发现甲状腺癌灶62个,乳头状甲状腺癌37例,滤泡状甲状腺癌4例,髓样癌9例,低分化癌3例。正常甲状腺组织的SUVmax为1.51±0.30,G1组(41例)SUVmax为4.25±1.70,G2组(12例)SUVmax为6.34±2.45,G1组和G2组的SUVmax均显著高于正常甲状腺组织(t=11.0,t=7.10,P<0.01),但G1组与G2组的SUVmax差异无统计学意义(t=3.61,P>0.05)。G3组(29例)的SUVmax为4.77±2.15,G4组(24例)的SUVmax为4.67±2.02,差异无统计学意义(t=0.33,P=0.56)。结论:18F-FDG PET/CT显像偶发癌分化型甲状腺癌、非分化型甲状腺癌均具有高糖代谢改变;不同分化程度、淋巴结转移能力的甲状腺癌灶的糖代谢水平差异无统计学意义。
[关键词]甲状腺偶发瘤;甲状腺癌;18F-FDG;PET/CT;分化型甲状腺癌;转移
18F-FDG PET/CT是目前临床常用的显像方法,在肿瘤的诊断和分期中发挥重要的作用。18F-FDG PET/CT显像的广泛应用导致偶发甲状腺瘤的比例明显增加[1-2]。有研究报道,在18F-FDG PET/CT显像发现的甲状腺偶发瘤中,大约1/3为甲状腺恶性肿瘤[3-5]。美国甲状腺学会(America Thyroid Association,ATA)指南推荐进一步行细胞学或组织学诊断[6]。偶发甲状腺癌灶的糖代谢与甲状腺癌病理学的相关性还不清楚。本研究分析了18F-FDG PET/CT显像偶发甲状腺癌的患者,甲状腺癌灶的糖代谢与病理类型、肿瘤分期的相关性,以探讨偶发甲状腺癌糖代谢水平的临床意义。
1 资料和方法
1.1研究对象
回顾性分析中国医科大学附属第一医院2004年11月—2013年12月因非甲状腺疾病原因行18F-FDG PET/CT显像的患者14 758例,其中195例显像发现甲状腺局灶性异常代谢增高灶,经手术病理证实为甲状腺癌的患者53例。其中男性22例,女性31例,年龄(51.0±12.4)岁。53例患者中,PET/CT显像发现甲状腺癌灶53个,病理学发现甲状腺癌灶62个,淋巴结转移灶73个。乳头状甲状腺癌37例,滤泡状甲状腺癌4例,髓样癌 9例,低分化癌3例。
1.2检查方法与参数设置
PET/CT采用GE Discovery LS PET/CT仪。CT为Lightspeed 4排螺旋CT。18F-FDG由GE Minitrace回旋加速器生产,通过合成模块自动合成,放化纯>95%。患者空腹4 h以上,空腹血糖小于10 mmol/L。平静状态下按5.55 MBq/kg通过静脉三通管注射18F-FDG。在暗室平卧50~60 min后行体部PET/CT显像,每个床位采集3 min,层厚5 mm。图像重建采用有序子集最大期望值迭代法,得到三维图像及横断、冠状和矢状断层图像。
1.318F-FDG PET/CT图像处理、分析
所有患者的图像均在GE XELERIS图像处理工作站进行分析处理,经2位有PET/CT诊断经验的医师逐层阅读PET/CT影像,通过视觉分析甲状腺部位18F-FDG分布高于周围正常甲状腺组织,即为甲状腺局限性代谢增高灶。对于选择甲状腺病灶摄取最显著的层面,应用感兴趣区(region of interest,ROI,直径为1.0 cm)技术测定病灶、区域淋巴结测量病灶的最大标准摄取值(SUVmax),并同时测量正常部位甲状腺组织的SUVmax。通过CT图像测量甲状腺病灶的直径。
1.4病理学分析
手术标本和区域淋巴结标本由病理科医师作病理分析。收集甲状腺癌的个数、病理分型和淋巴结转移数据。
1.5统计学处理
2 结 果
18F-FDG PET/CT显像偶发甲状腺癌灶53个。病理学发现甲状腺癌灶62个,其中8例患者病理见多灶性微小甲状腺癌,PET/CT显像未检出。乳头状甲状腺癌37例,滤泡状甲状腺癌4例,髓样癌9例,低分化癌3例。分化型甲状腺癌组(G1组)41例,非分化型甲状腺癌组(G2组)12例。甲状腺癌无淋巴结转移组(G3组)29例,甲状腺癌有淋巴结转移组(G4组)24例(表1、2)。
正常甲状腺组织的SUVmax为1.51±0.30,G1组SUVmax为4.25±1.70(图1)。G2组SUVmax为6.34±2.45(图2),G1组和G2组的SUVmax均显著高于正常甲状腺组织(t=11.0,t=7.10,P<0.01),但G1组与G2组的SUVmax差异无统计学意义(t=3.61,P=0.06)。G1组的癌灶大小为(1.40±0.63) cm,G2组的癌灶大小为(1.74±0.41) cm,差异无统计学意义(t=0.06, P=0.80)。
G3组的SUVmax为4.77±2.15,G4组的SUVmax为4.67±2.02,差异无统计学意义(t=0.33,P=0.56)。G3组的癌灶大小为(1.41±0.50) cm,G4组的癌灶大小为(1.56±0.70) cm,差异无统计学意义(t=0.12,P=0.73)。所有甲状腺癌灶SUVmax与肿瘤大小之间呈正相关(r=0.38,P<0.01)。
17例G1组患者发生淋巴结转移,7例G2组患者发生淋巴结转移,两者发生淋巴结转移的比例差异无统计学意义(χ2=1.06,P=0.3)。
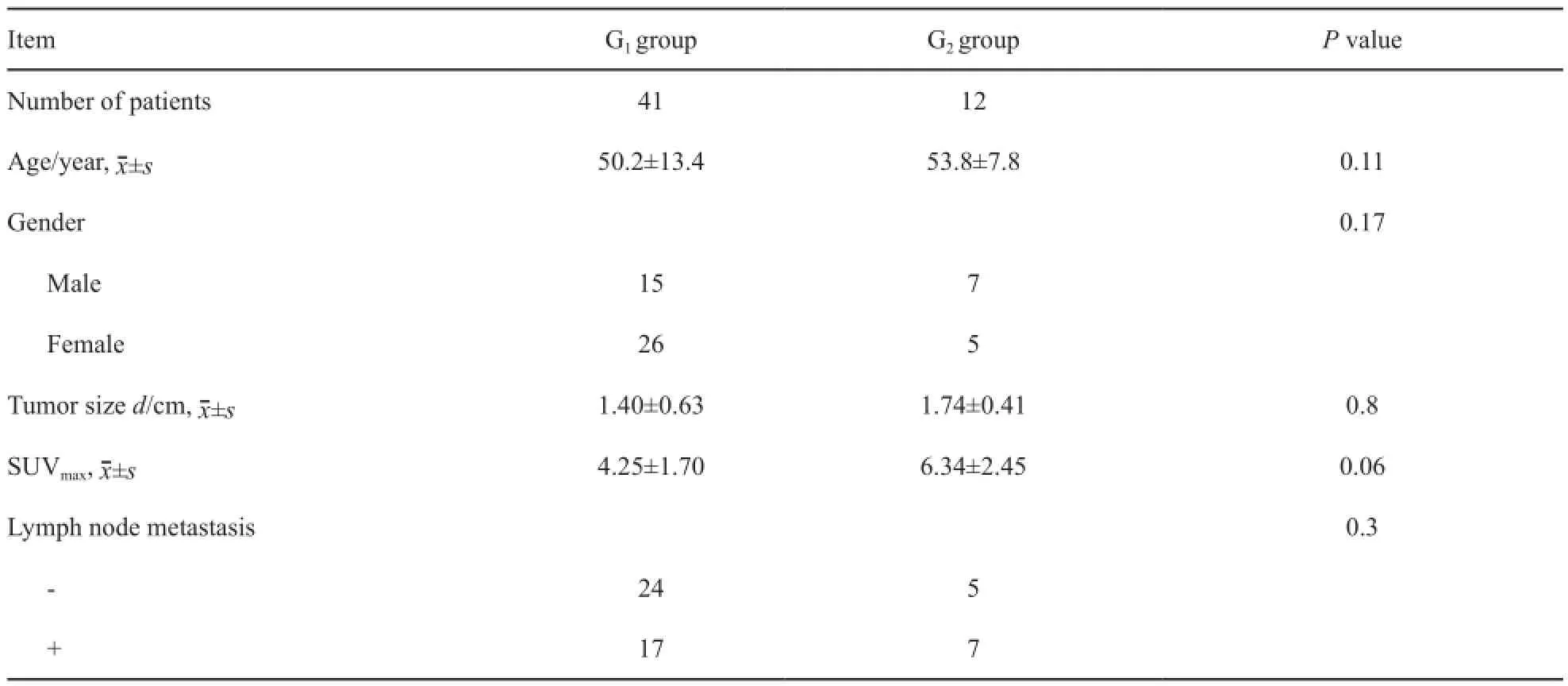
表1 G1组和G2组的临床特征Tab.1 Clinical characteristics of G1group and G2group
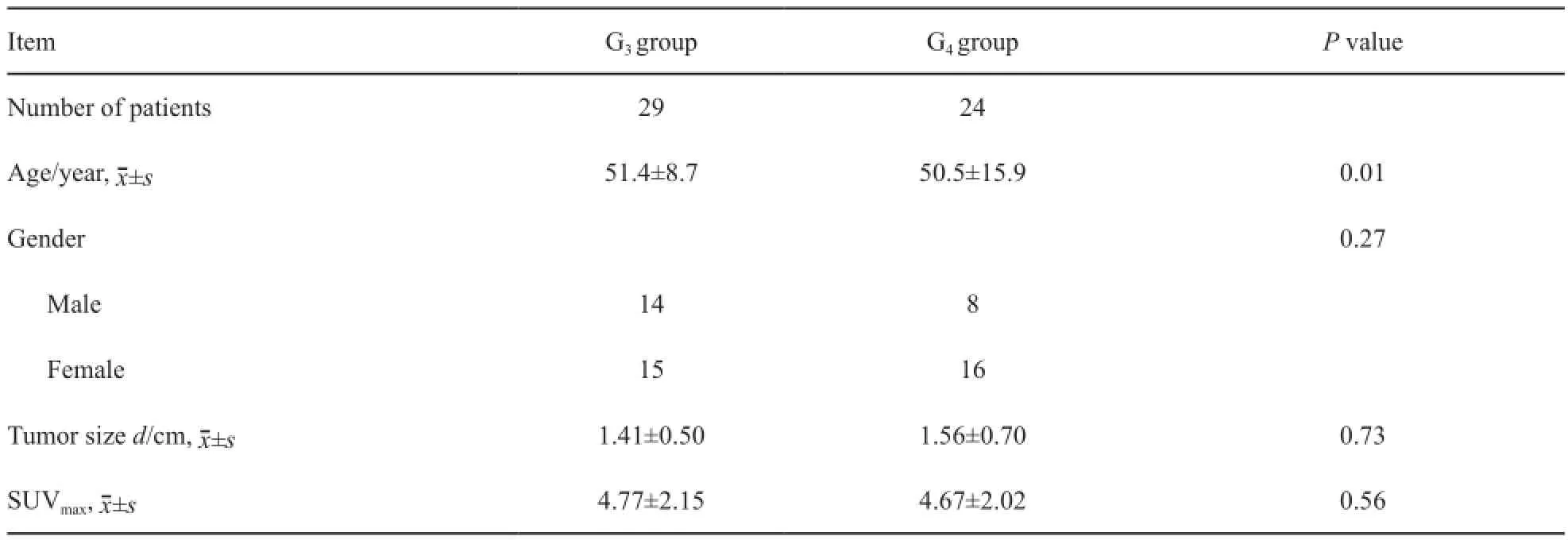
表2 G3组和G4组临床特征Tab.2 Clinical characteristics of G3group and G4group

图1 18F-FDG PET/CT显像和病理图片Fig.118F-FDG PET/CT image and pathological image
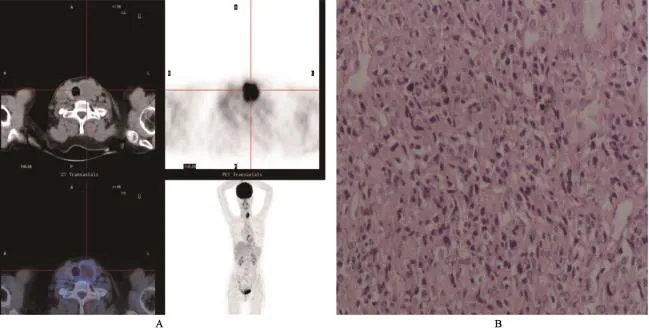
图2 18F-FDG PET/CT 显像和病理图片Fig.218F-FDG PET/CT image and pathological image
3 讨 论
一项多中心研究结果显示,PET显像发现的甲状腺偶发瘤的比例为1.6%[5]。本研究中,18F-FDG PET/CT显像发现的甲状腺偶发瘤的比例为1.3%。在多个单中心的研究中,18F-FDG PET/CT偶发甲状腺瘤的恶性率是不一致的[2,7-8]。多中心的研究结果显示,恶性率约为34%[3,5,9]。本研究中,甲状腺偶发瘤的恶性率为27.1%。因此,这样的恶性率在临床工作中不应该被忽视。
SUV值是18F-FDG PET/CT显像评价病变葡萄糖代谢的重要参数,恶性肿瘤组织的SUV值会升高[10],正常的甲状腺组织的SUV值不会升高[11]。本研究中,偶发瘤的甲状腺癌灶的SUV值明显高于正常的甲状腺组织。偶发甲状腺癌的糖代谢水平升高的临床意义还不清楚。18F-FDG PET/CT通常被应用于分化型甲状腺癌Tg升高、全身碘显像阴性怀疑甲状腺癌发生了失分化的患者中[12-13]。有研究显示,甲状腺癌失分化后,碘的摄取能力丧失,而糖代谢被激活,葡萄糖转运体1的表达增加[14]。而分化好的甲状腺癌葡萄糖转运体1表达较低[15],分化型甲状腺癌是预后相对好的肿瘤,因此分化型甲状腺癌常被认为是低糖代谢的改变[16-17]。而在本研究中,分化型甲状腺癌41例,乳头状甲状腺癌37例,滤泡状甲状腺癌4例,均具有高糖代谢的影像表现。既往的多中心的研究也显示,18F-FDG PET/CT显像偶发甲状腺癌的大部分病理分型为乳头状癌[5],与我们的研究结果一致。这一现象与我们既往对分化型甲状腺糖代谢认知不同。有研究报道,在分化型甲状腺癌中,葡萄糖转运体3高表达[18],因此,分化型甲状腺癌可能也具有摄取18F-FDG的分子基础,具体的机制还需要进一步研究。本研究中,分化型甲状腺癌与髓样癌、低分化癌的SUVmax值分别为4.25±1.70 和6.34±2.45,髓样癌、低分化癌的SUV值略高于分化型甲状腺癌,但差异无统计学意义(P=0.06)。本研究的髓样癌与低分化癌的样本量较少,因此可能会影响统计结果,有待于进一步扩大样本量,分析两者的SUV值的差别。一项对18F-FDG PET/CT偶发甲状腺癌进行了预后的随访研究显示,葡萄糖代谢增高的甲状腺癌,预后不良[19]。因此,我们推测葡萄糖代谢增高的分化型甲状腺癌有可能是一种病理亚型,可能与分化型甲状腺癌的不良预后相关。
有研究显示,偶发甲状腺癌灶的葡萄糖代谢体积和总糖酵解与肿瘤淋巴结转移密切相关,高的代谢体积和总糖酵解的分化型甲状腺癌更易发生淋巴结转移[20]。但本研究结果显示,甲状腺癌原发灶的SUVmax在转移组和非转移组中差异无统计学意义,我们应用的评价代谢参数与他们不同,可能会导致研究结果的不同。因此,还需要扩大样本量和采用多种评价糖代谢的参数进行这方面的研究。本研究显示,甲状腺癌的SUVmax与病灶大小呈正相关。有研究报道,病灶大小是影响SUV值的重要因素之一[21]。在本研究中,8例甲状腺微小癌灶在18F-FDG PET/CT显像中未显影,是因为小病灶受显像的分辨率限制或部分容积效应的影响。
本研究样本量较少,有一定局限性,且本研究是回顾性分析,显像方法中的影响图像质量的因素不是标准化的。因此,需要扩大样本量,并进行前瞻性的研究,探讨18F-FDG PET/ CT显像偶发癌的葡萄糖代谢的临床意义及与肿瘤侵袭转移的相关性。
本研究显示,偶发癌中分化型甲状腺癌和非分化型甲状腺癌均具有高糖代谢改变;不同分化程度、侵袭转移能力的甲状腺癌,癌灶糖代谢水平差异无统计学意义。
[参考文献]
[1] NISHIMORI H, TABAH R, HICKESON M, et al. Incidental thyroid “PETomas“: clinical significance and novel description of the self-resolving variant of focal FDG-PET thyroid uptake [J]. Can J Surg, 2011, 54(2): 83-88.
[2] BRINDLE R, MULLIAN D, YAP B K, et al. Thyroid incidentalomas discovered on positron emission tomography CT scanning-malignancy rate and significance of standardized uptake values [J]. Eur J Surg Oncol, 2014, 40(11): 1528-1532.
[3] SOELBERG K K, BONNEMA S J, BRIX T H, et al. Risk of malignancy in thyroid incidentalomas detected by18F-fluorodeoxyglucose positron emission tomography: a systematic review [J]. Thyroid, 2012, 22(9): 918-925.
[4] TREGLIA G, BERTAGNA F, SADEGHI R, et al. Focal thyroid incidental uptake detected by18F-fluorodeoxyglucose positron emission tomography. Meta-analysis on prevalence and malignancy risk [J]. Nuklearmedizin, 2013, 52(4):130-136.
[5] BERTAGNA F, TREGLIA G, PICCARDO A, et al. Diagnostic and clinical significance of18F-FDG-PET/CT thyroid incidentalomas [J]. J Clin Endocrinol MeTab.2012, 97(11):3866-3875.
[6] American Thyroid Association (ATA) Guidelines Taskforce on Thyroid Nodules and Differentiated Thyroid Cancer, COOPER D S, DOHERTY G M, et al. Revised American Thyroid Association management guidelines for patients with thyroid nodules and differentiated thyroid cancer [J]. Thyroid,2009, 19(11): 1167-1214.
[7] ELZEIN S, AHMED A, LORENZ E, et al. Thyroid incidentalomas on PET imaging-evaluation of management and clinical outcomes [J]. Surgeon, 2015, 13(2): 116-120. [8] BAE J S, CHAE B J, PARK W C, et al. Incidental thyroid lesions detected by FDG-PET/CT: prevalence and risk of thyroid cancer [J]. World J Surg Oncol, 2009, 10(7): 63. [9] BERTAGNA F, TREGLIA G, PICCARDO A, et al.18F-FDGPET/CT thyroid incidentalomas: a wide retrospective analysis in three Italian centers on the significance of focal uptake and SUV value [J]. Endocrine, 2013, 43(3): 678-685.
[10] KUMAR V, NATH K, BERMAN C G, et al. Variance of SUVs for FDG-PET/CT is greater in clinical practice than under ideal study settings [J]. Clin Nucl Med, 2013, 38(3): 175-182.
[11] SCHODER H, YEUNG H W. Positron emission imaging of head and neck cancer, including thyroid carcinoma [J]. Semin Nucl Med, 2004, 34(3): 180-197.
[12] DONG M J, LIU Z F, ZHAO K, et al. Value of18F-FDG-PET/ PET-CT in differentiated thyroid carcinoma with radioiodinenegative whole-body scan: a metaanalysis [J]. Nucl Med Commun, 2013, 30(8): 639-650.
[13] 林岩松,张 彬,梁智勇,等. 复发转移性分化型甲状腺癌诊治共识 [J]. 中国癌症杂志, 2015, 25(7): 481-496.
[14] FEINE U, LIETZENMAYER R, HANKE J P, et al. Fluorine-18-FDG and iodine-131-iodide uptake in thyroid cancer [J]. J Nucl Med, 1996, 37(9): 1468-1472.
[15] CHANDAN V S, FAQUIN W C, WILBUR D C, et al. The role of immunolocalization of CD57 and GLUT-1 in cell blocks in fine-needle aspiration diagnosis of papillary thyroid carcinoma [J]. Cancer, 2006, 108(5): 331-336.
[16] TREGLIA G, BERTAGNA F, PICCARDO A, et al.131I wholebody scan or18F-FDG PET/CT for patients with elevated thyroglobulin and negative ultrasound? [J]. Clin Transl Imaging, 2013, 16(9): 770-775.
[17] MAZZAFERRI E L, KLOOS R T. Current approaches to primary therapy for papillary and follicular thyroid cancer [J]. J Clin Endocrinol MeTab.2001, 86(4): 1447-1463.
[18] CIAMPI R, VIVALDI A, ROMEI C, et al. Expression analysis of facilitative glucose transporters (GLUTs) in human thyroid carcinoma cell lines and primary tumors [J]. Mol Cell Endocrinol, 2008, 291(1-2): 57-62.
[19] PICCARDO A, PUNTONI M, BERTAGNA F, et al.18F-FDG uptake as prognostic variable in primary differentiated thyroid cancer incidentally detected by PET/CT: a multicenter study [J]. Eur J Nucl Med Mol Imaging, 2014, 41(8): 1482-1491.
[20] KIM B H, KIM S J, KIM K, et al. High metabolic tumor volume and total lesion glycolysis are associated with lateral lymph node metastasis in patients with incidentally detected thyroid carcinoma [J]. Ann Nucl Med, 2015, 29(8): 721-729.
[21] STANGIERSKI A, WOLIŃSKI K, CZEPCZYŃSKI R, et al. The usefulness of standardized uptake value in differentiation between benign and malignant thyroid lesions detected incidentally in18F-FDG-PET/CT examination [J]. PLoS One, 2014, 9(10): e109612.
DOI:10.19401/j.cnki.1007-3639.2016.06.008
中图分类号:R736.1
文献标志码:A
文章编号:1007-3639(2016)06-0527-06
收稿日期:(2015-11-30 修回日期:2016-01-17)
基金项目:辽宁省科学技术计划项目(2012225013)。通信作者:李亚明 E-mail: ymli2001@163.com
The correlation study between the glucose metabolism of 18F-FDG PET/CT incidental thyroid cancer and clinicopathologic characteristics
LI Xuena, YIN Yafu, DU Bulin, LI Yaming (Department of Nuclear Medicine, the First Hospital of China Medical University, Shenyang 110001, Liaoning Province, China)Correspondence to: LI Yaming E-mail: ymli2001@163.com
[Abstract]Background and purpose: The proportion of incidental thyroid cancer in PET imaging was signifcantly increased with the wide application of18F-FDG PET/CT. The correlation between the glucose metabolism of thyroid incidental thyroid cancer and pathological changes is unclear. The objective of this study is to analyze the relationship between the glucose metabolism by18F-FDG PET/CT and tumor diferentiation or lymph node metastasis in patients with incidental thyroid cancer. Methods: A total of 195 patients with focal FDG-avid thyroid incidentaloma during cancer evaluation were enrolled. Fifty-three patients were diagnosed as having thyroid cancer by the pathology. The SUVmaxof thyroid cancer foci, lesion size, lesion number, and SUVmaxof normal thyroid tissue were quantifed. The tumor pathological grades and lymph node metastasis were analyzed by the pathology. The patients were broken down into 4 groups (G1, G2, G3and G4) according to the tumor pathological grades and lymph node metastasis (diferentiated thyroid cancer, non-diferentiated thyroid cancer, without lymph node metastasis and with lymph node metastasis). The diferences of glucose metabolism between G1and G2groups, G3and G4groups were analyzed. Results: Fifty-three foci were found by PET imaging. Sixty-two foci were found by the pathology (37 papillary thyroid carcinoma, 4 follicular thyroid carcinoma, 9 medullary thyroid carcinoma, 3 poorly diferentiated thyroid cancer). The SUVmaxin the normal thyroid tissue, G1and G2were 1.51±0.30, 4.25±1.70 and 6.34±2.45, respectively. The SUVmaxin the G1and G2weresignifcantly higher than in the normal thyroid tissue (t=11.0,t=7.10,P<0.01). The SUVmaxof G3was 4.77±2.15, and the SUVmaxof G4group was 4.67±2.02. The diferences between G1and G2groups, G3and G4groups were not statistically signifcant (t=3.61, P>0.05; t=0.33, P=0.56). Conclusion: The diferentiated incidental thyroid carcinoma and non-diferentiated incidental thyroid carcinoma had high glucose metabolism, and there was no signifcant diference in the levels of glucose metabolism in diferent diferentiation degree and metastasis ability cancer.
[Key words]Thyroid incidentalomas; Thyroid cancer;18F-FDG; PET/CT; Diferentiated thyroid cancer; Metastasis