尼可地尔联合替罗非班对急性心肌梗死患者急诊PCI术后心肌微循环和心功能短期预后的影响
王立中,董 鹏,刘 芳,姜 阳,李远征,张 斌
(航空总医院,北京 100012)
尼可地尔联合替罗非班对急性心肌梗死患者急诊PCI术后心肌微循环和心功能短期预后的影响
王立中,董鹏,刘芳,姜阳,李远征,张斌
(航空总医院,北京 100012)

目的探讨急诊PCI术中及术后冠脉及静脉内给予尼可地尔和替罗非班对急性心肌梗死患者PCI术后心肌微循环和心功能短期预后的影响。方法连续入选行急诊PCI的急性心肌梗死患者120例,随机分为联合组、替罗非班组和对照组各40例。联合组和替罗非班组均于PCI术中冠脉内给予负荷量替罗非班10 μg/kg,随后予替罗非班0.15 μg/(kg·min)持续静脉滴注至PCI术后48 h;联合组在应用替罗非班基础上PCI术中冠脉内给予尼可地尔负荷量0.06 mg/kg,随后予尼可地尔2 mg/h持续静点48 h。术后3组均予常规冠心病Ⅱ级预防药物治疗。统计3组PCI术后冠脉TIMI血流3级比率及校正的冠脉TIMI血流帧数,并在术后6,10,14,18,24和48 h测定血清肌酸激酶(CK)、肌酸激酶同工酶(CK-MB)及超氧化物歧化酶(SOD)、内皮素(ET)和高敏C反应蛋白(hs-CRP)以找出其中峰值浓度,术后24 h及4周后测定血浆N-末端脑钠肽前体(NT-proBNP)水平及行超声心动图测定左室舒张末内径(LVEDD)、左室收缩末内径(LVESD)和左室射血分数(LVEF)。结果联合组和替罗非班组术后冠脉TIMI血流3级比率均明显高于对照组(P均<0.05),PCI术后冠脉校正的TIMI血流帧数及48 h内CK、CK-MB峰值浓度均明显低于对照组(P均<0.05),但联合组和替罗非班组比较差异均无统计学意义(P均>0.05);48 h内联合组SOD峰值浓度明显高于其他2组(P均<0.05),ET和hs-CRP峰值浓度均明显低于其他2组(P均<0.05),替罗非班组和对照组比较差异均无统计学意义(P均>0.05)。术后24 h,3组血浆NT-proBNP水平和LVEDD、LVESD、LVEF比较差异均无统计学意义(P均>0.05);术后4周,联合组血浆NT-proBNP水平及LVESD、LVEDD均明显低于其他2组(P均<0.05), LVEF均明显高于其他2组(P均<0.05),而替罗非班组与对照组比较差异均无统计学意义(P均>0.05)。结论尼可地尔联合替罗非班不仅可通过抗血小板和抗血栓作用明显改善心肌微循环,而且可通过扩张冠状动脉微循环血管和抗氧化、抗炎及改善冠状动脉微循环血管内皮功能等减轻心肌再灌注损伤,两种药物联合应用可以明显减少急性心肌梗死急诊PCI术后心肌损伤和坏死,可改善心功能短期预后。
尼可地尔;替罗非班;心肌梗死;心肌微循环
急诊PCI开通罪犯血管只是心外膜血管达到了解剖上的再通,而微循环往往存在灌注不良。血小板ⅡB/ⅢA受体抑制剂(如替罗非班)可以在一定程度上改善微循环血流,因此急诊PCI术中冠脉内给予替罗非班已成为ACC/AHA指南中Ⅱa B类适应证,术后持续静脉滴注48 h也可给患者临床预后带来益处,但替罗非班主要是通过抗血小板而起抗栓作用,并不能减轻患者心肌再灌注损伤[1-3]。已有基础实验和临床研究证明尼可地尔是一种ATP敏感的钾通道开放剂,其可通过扩张冠状动脉微血管而改善心肌血供,减少心肌坏死,还可通过抗炎及抗氧化作用保护微循环血管内皮功能,减轻患者心肌再灌注损伤而改善近远期预后[4-6]。目前尼可地尔联合替罗非班用在急诊PCI患者中在国内尚少见。本研究旨在观察尼可地尔联合替罗非班对急性心肌梗死患者PCI术后心肌损伤的保护作用和对心功能短期预后的影响,现将结果报道如下。
1 临床资料
1.1一般资料选择2014年3月—2015年9月在我院心内科行急诊PCI术的急性心肌梗死患者120例,患者均符合2015年中华医学会心血管分会修订的急性ST段抬高性心肌梗死诊断标准,除外伴有严重肝肾功能不全者。其中男88例,女32例;年龄35~77岁,平均60.2岁。将患者随机分为对照组、替罗非班组和联合组各40例,3组间一般资料比较差异均无统计学意义(P均>0.05),见表1。本研究已经过我院伦理委员会通过,并告知患者家属及本人后签署治疗知情同意书。
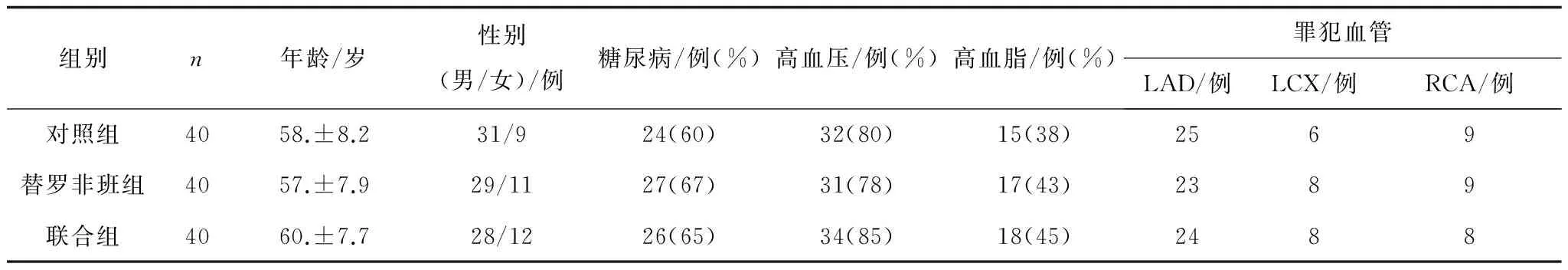
表1 3组一般资料比较
1.2治疗方法替罗非班组和联合组根据患者体质量PCI术中冠脉内给予负荷量替罗非班(远大医药中国有限公司,国药准字H20041165)10 μg/kg,术后予替罗非班0.15 μg/(kg·min)持续静点48 h;联合组在此基础上术中予冠脉内尼可地尔(北京四环科宝制药有限公司,国药准字H20120069)0.06 mg/kg,术后予尼可地尔2 mg/h静点48 h。3组均接受相同的常规冠心病Ⅱ级预防治疗。
1.3检测指标统计3组PCI术后冠脉TIMI血流3级比率及校正的冠脉TIMI血流帧数(CTFC),并在术后6,10,14,18,24和48 h测定血清肌酸激酶(CK)、肌酸激酶同工酶(CK-MB)及超氧化物歧化酶(SOD)、血清内皮素(ET)和高敏C反应蛋白(hs-CRP)以找出其中峰值浓度,术后24 h及4周后测定血浆N-末端脑钠肽前体(NT-proBNP)水平及行超声心动图测定左室舒张末内径(LVEDD)、左室收缩末内径(LVESD)和左室射血分数(LVEF)。

2 结 果
2.13组PCI术后冠脉TIMI血流3级比率和CTFC比较3组患者均完成4周治疗及随访,无再住院和死亡者。联合组和替罗非班组PCI术后冠脉TIMI血流3级比率均明显高于对照组(P均<0.05),CTFC均明显低于对照组(P均<0.05),联合治疗组和替罗非班组比较差异均无统计学意义(P均>0.05)。见表2。
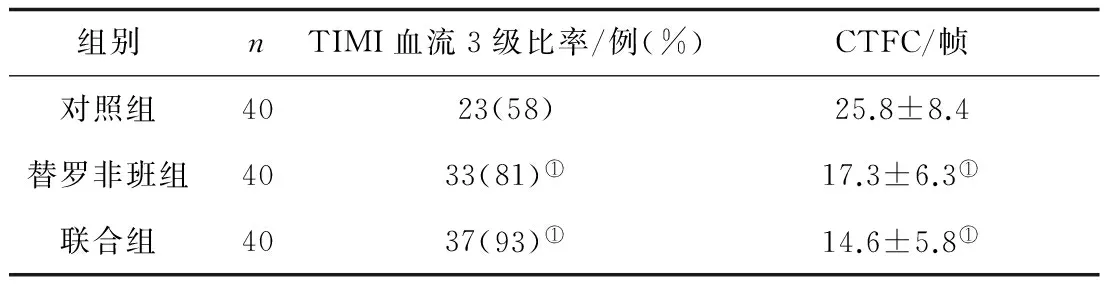
表2 3组PCI术后冠脉TIMI血流3级比率和CTFC比较
注:①与对照组比较,P<0.05。
2.23组治疗后CK、CK-MB、SOD、ET和hs-CRP峰值浓度比较术后48 h内联合组和替罗非班组CK、CK-MB峰值浓度均明显低于对照组(P均<0.05),联合组和替罗非班组比较差异均无统计学意义(P均>0.05);联合组SOD峰值浓度明显高于其他2组(P均<0.05),ET和hs-CRP峰值浓度均明显低于其他2组(P均<0.05),替罗非班组和对照组比较差异均无统计学意义(P均>0.05)。见表3。

表3 3组治疗后CK、CK-MB、SOD、ET和hs-CRP峰值浓度比较
注:①与联合组比较,P<0.05。
2.33组术后24 h及4周血浆NT-proBNP水平和LVEDD、LVESD及LVEF比较术后24 h,3组血浆NT-proBNP水平和LVEDD、LVESD、LVEF比较差异均无统计学意义(P均>0.05)。术后4周,3组血浆NT-proBNP水平均明显低于术后24 h(P均<0.05),联合组LVEF明显高于术后24 h(P<0.05);联合组血浆NT-proBNP水平及LVESD、LVEDD均明显低于其他2组(P均<0.05), LVEF均明显高于其他2组(P均<0.05),而替罗非班组与对照组比较差异均无统计学意义(P均>0.05)。见表4。

表4 3组术后24 h及4周血浆NT-proBNP水平和LVEDD、LVESD及LVEF比较
注:①与术后24 h比较,P<0.05;②与联合组比较,P<0.05。
3 讨 论
急性心肌梗死早期开通冠脉罪犯血管可恢复冠脉血流和改善心肌微循环,减少梗死范围,防止左室重构,改善患者预后。但心外膜冠脉的再通并不表示心肌微循环血管达到了完全的再灌注,仍会因为微血栓栓子和斑块碎屑的脱落造成微循环灌注不良或由于微循环血管内皮细胞水肿、心肌细胞钙超载等引起细胞坏死及微血管痉挛。急诊PCI术后应用替罗非班可以通过抑制血小板聚集改善心肌微循环,从而改善心肌血供达到减少心肌坏死的目的[1,3]。但也有部分心肌梗死患者缺乏心肌梗死前缺血预适应的过程,一旦梗死相关血管(IRA)开通就会在一定程度上出现心肌微循环障碍,从而影响心功能预后。而心肌微循环障碍是患者住院病死率增加的重要因素,CK和CK-MB是衡量微循环障碍和再灌注损伤的重要指标,和患者心功能预后明显相关[7-9]。
心肌缺血预适应和后适应所出现心肌保护作用的现象为药物或介入手段干预IRA提供了理论依据。有报道尼可地尔对防止急性心肌梗死患者的梗死面积延展、缩小梗死面积、保护缺血心肌及恢复心功能有一定作用,其可通过减轻心肌过氧化损伤及抑制交感神经兴奋性等有助于急性心肌梗死患者溶栓后ST段完全回落,降低再灌注时室早、室速的发生率,改善左室功能[10-12];另有报道尼可地尔可通过改善冠心病患者冠脉血管的内皮功能从而达到改善心功能的作用[13-14]。
本研究结果表明,联合组急诊PCI术后反映心外膜罪犯血管再通的TIMI血流3级比率明显升高,反映微循环灌注的CTFC明显降低,反映心肌坏死的 CK、CK-MB峰值浓度明显降低,反映抗氧化应激作用的SOD明显升高,反映心肌坏死和炎症反应的ET和hs-CRP峰值浓度均明显下降,提示联合治疗可改善心肌微循环,减少心肌坏死和,减轻再灌注损伤。治疗4周后联合组血浆NT-proBNP水平明显减低,反映左心室重构的LVESD、LVEDD明显改善,反映心功能的LVEF明显升高,说明患者的短期预后明显改善。尼可地尔所表现出的有益作用可能与其扩张心外膜下冠状动脉和心内膜下微循环血管、抗氧化应激和抗炎症反应以及改善冠脉血管内皮功能有关,甚或与抗血小板激活和聚集防止微循环血栓形成有关,而这些有益作用并不影响患者的血压、心率及心肌收缩力和心肌耗氧量。但急诊PCI术中至术后联合应用尼可地尔和替罗非班治疗的有效性和合理性,特别是冠脉内应用尼可地尔的安全性还需进一步观察;另外尼可地尔对心功能预后有无量效关系及对心功能远期疗效也需进一步评价。
[1]Lavi S,Gruberg L,Kapeliovich M,et al. The impact of GP IIb/IIIa inhibitors during primary percutaneous coronary intervention in acute myocardial infarction patients[J]. J Invasive Cardiol,2005,17(6):296-299
[2]KarvouniE,KatritsisDG,IoannidisJP.IntravenousglycoproteinⅡb/Ⅲareceptorantagonistsreducemortalityafterpercutaneouscoronaryinterventions[J].JAmCollCardiol,2003,41(1):26-32
[3]Liu X,Tao GZ. E ffects of tirofiban on the reperfusion-related no-reflow in rats with acute myocardial infarction[J]. J Geriatr Cardiol,2013,10(1):52-58
[4]赵京林,杨跃进,尤士杰,等. 尼可地尔对猪急性心肌梗死再灌注后无再流的影响[J]. 中国危重病急救医学,2005,17(7):421-425
[5]Iwakura K. Modulation of individual susceptibility to the no-reflow phenomenon after acute myocardial infarction[J]. Curr Pharm Des,2013,19(25):4519-4528
[6]Sakata Y,Nakatani D,Shimizu M,et al. Oral treatment with nico-randil at discharge is associated with reduced mortality after acute myocardial infarction[J]. J Cardiol,2012,59(1):14-21
[7]王立中,俞晓微,赵冬靖,等. 替罗非班联用前列地尔对急诊经皮冠脉介入治疗术后心肌梗死患者心肌再灌注和心功能短期预后的影响[J]. 中国医药导报,2013,17(10):77-82
[8]Sharma V,Bell RM,Yellon DM. Targeting reperfusion injury ina-cute myocardial infarction:a review of reperfusion injury pharmacotherapy[J]. Expert Opin Pharmacother,2012,13(8):1153-1175
[9]Luo Y,Pan YZ,Zeng C,et al. Altered serum creatine kinase level and cardiac function in ischemia-reperfusion injury during percutaneous coronary intervention[J]. Med Sci Monit,2011,17(9):CR474-479
[10] Ota S,Nishikawa H,Takeuchi M. Impact of nicorandil to prevent reperfusion injury in patients with acute myocardial infarction: Sigmart Multicenter Angioplasty Revascularization Trial (SMART) [J]. Circ J,2006,70(9):1099-1014
[11] Iwakura K,Ito H,Okamura A,et al. Nicorandil treatment in patients with acute myocardial infarction:a meta-analysis[J]. Circ J ,2009,73(5):925-931
[12] Kasama S,Toyama T,Sumino H. Long-term nicorandil therapy improves cardiac sympathetic nerve activity after reperfusion therapy in patients with first acute myocardial infarction[J]. J Nucl Med,2007,48(10):1676-1682
[13] Wu M,Huang Z,Xie H,et al. Nicorandil in patients with acute myocardial infarction undergoing primary percutaneous coronary intervention:a systematic review and meta-analysis[J]. PLoS One,2013,8(10):e78231
[14] Fujiwara T,Matsunaga T,Kameda K,et al. Nicorandil suppresses the increases in plasma level of matrix metalloproteinase activity and attenuates left ventricular remodeling in patients with acute myocardial infarction[J]. Heart Vessels,2007,22(5):303-309
Effects of combination therapy of tirofiban and nicorandil on cardiac function and myocardial microcirculation in patients with acute ST segment elevation myocardial infarction after percutaneous coronary intervention
WANG LiZhong,DONG Peng,LIU Fang,JIANG Yang,LI Yuanzheng,ZHANG Bin
(Aviation General Hospital, Beijing 100012, China)
Objective It is to evaluate the effects of combination therapy of tirofiban and nicorandil on cardiac function and myocardial microcirculation in patients with acute ST segment elevation myocardial infarction (STEMI) after percutaneous coronary intervention(PCI). Methods 40 patients with STEMI admitted to Aviation General Hospital from September 2012 to May 2015 were selected randomly into contrast group and 40 cases into tirofiban observation group and 40 cases into tirofiban and nicorandil observation group. Loading dose of tirofiban by bolus drop. Nicorandil (0.06 mg/kg) was dropped into coronary artery during PCI and (2 mg/h) used in nicorandil and tirofiban group for 48 hs after PCI. The rate of TIMI 3 grade and corrected TIMI frame count (CTFC) was counted in three groups. Tirofiban (10 μg/kg) was injected into intracoronary by bolus according to weight of patients in tirofiban and combination groups during PCI. After PCI tirofiban [0.15 μg/(kg·min)] was used for 48 hs Concentrations of serum CK, CK-MB, Endotheiin (ET), superoxide dismutase (SOD) and high sensitive C-reactive protein (hs-CRP) were tested at 6 h, 10 h, 14 h, 18 h, 24 h and 48 h after PCI for finding out the peak level. Amino terminal-pro brain natriuretic peptide (N-proBNP) was checked and Echocardiography was done at 24 h and 4 weeks. Results The rate of TIMI 3 grade was higher in two observation groups than one in contrast group (P<0.05). Serum peak levels of CK, CK-MB and CTFC were lower after therapy in two observation groups than ones in contrast group(P<0.05), no differences between two observation groups (P>0.05). Though serum peak levels of ET and hs-CRP were lower and SOD was higher in nicorandil and tirofiban group than ones in tirofiban and contrast groups (P<0.05), no differences between tirofiban and contrast groups (P>0.05). NT-proBNP and value of LVEDD, LVESD and LVEF were no different among three groups at 24 h after PCI. In nicorandil and tirofiban group N-proBNP and value of LVEDD, LVESD was lower and value of LVEF was higher than ones in contrast group 4 weeks after PCI(P<0.05). Though value of LVEF was increasing trend in tirofiban group than one in contrast group, no significant change was found in two groups (P>0.05). Conclusion Nicorandil and tirofiban treatments may improve myocardial blood supply by ablating microcirculation and anti-thrombus but also may decrease myocardial ischemia-reperfusion injury and improve endothelial function of coronary artery by anti-inflammatory and antioxidant. Combination therapy Nicorandil and tirofiban might decrease myocardium injury and enhance cardiac function.
tirofiban; nicorandil; myocardial infarction; myocardial microcirculation
王立中,男,主任医师,主要从事冠心病介入治疗。
10.3969/j.issn.1008-8849.2016.17.004
R542.22
A
1008-8849(2016)17-1834-04
2016-01-15