股神经阻滞对老年膝关节置换术后炎性反应与认知功能的影响
罗振国, 肖 莉, 吴 刚, 董补怀, 吕建瑞, 薛荣亮*
(1西安交通大学医学院附属红会医院麻醉科,西安 710054; 2西安交通大学第二附属医院麻醉科;*通讯作者,E-mail:xuerl299@163.com)
股神经阻滞对老年膝关节置换术后炎性反应与认知功能的影响
罗振国1, 肖莉1, 吴刚2, 董补怀1, 吕建瑞2, 薛荣亮2*
(1西安交通大学医学院附属红会医院麻醉科,西安710054;2西安交通大学第二附属医院麻醉科;*通讯作者,E-mail:xuerl299@163.com)
目的探讨股神经阻滞对全麻下老年膝关节置换患者术后炎性反应与认知功能的影响。方法择期全麻下行膝关节置换术老年患者80例,年龄65-78岁,ASAⅠ或Ⅱ级,随机分为两组:单纯全麻组(n=40)与股神经阻滞复合全麻组(n=40)。均行气管插管全麻,股神经阻滞复合组麻醉诱导前在神经刺激仪引导下行股神经阻滞。分别于麻醉诱导后(T1),术后1 h(T2)、24 h(T3)、72 h(T4)采集静脉血测定血清IL-6、C-反应蛋白(CRP)水平。术前1 d,术后1,7 d均采用简易智能量表(MMSE)评估患者的认知水平,记录术后认知功能障碍(POCD)的发生情况。结果与T1时比较,T3时两组患者IL-6、CRP水平均明显升高(P<0.05)。与全麻组比较,T3时股神经阻滞复合组患者IL-6、CRP水平明显降低(P<0.05)。与术前比较,术后1 d两组患者的MMSE评分均明显降低,且全麻组明显低于股神经阻滞复合组(P<0.05)。股神经阻滞复合组术后1 d发生POCD 明显少于全麻组(20.0%vs50%P<0.05)。结论股神经阻滞可降低老年膝关节置换术患者术后炎性因子水平,降低POCD的发生。
股神经阻滞;老年人;炎性反应;认知功能障碍
[12]Liu Y.FDG PET differentiation of tumor recurrence from post-stereotactic radiosurgical scar in a central neurocytoma[J].Clin Nucl Med,2013,38(6):469-470.
[13]鲍俊初,周文兰,王全师,等.18F-FDG PET/CT显像在胃癌术后复发和转移中的诊断价值[J]. 中国临床医学影像杂志, 2010, 2l(10):701-704.
[14]Votrubova J,Belohlavek O,Jaruskova M,etal.The role of FDG-PET/CT in the detection of recurrent colorectal cancer[J].Eur J Nucl Med Mol Imaging,2006,33(7):779-784.
[15]Sun L,Guan YS,Pan WM,etal.Clinical value of18F-FDG PET/CT in assessing suspicious relapse after rectal cancer resection[J].World J Gastrointest Oncol,2009,1(1):55-61.
[16]Jo HJ,Kim SJ,Lee HY,etal.Prediction of survival and cancer recurrence using metabolic volumetric parameters measured by18F-FDG PET/CT in patients with surgically resected rectal cancer[J].Clin Nucl Med,2014, 39(6):493-497.
术后认知功能障碍(postoperative cognitive dysfunction, POCD)是手术麻醉后以理解力、记忆力、注意力下降为特征的中枢神经系统并发症,老年患者更易发生。研究显示炎性反应与POCD的发生密切相关[1]。手术创伤和疼痛可激活免疫系统,产生大量促炎因子,引起机体炎症反应, 老年人中枢神经系统在应激下易发生炎性反应,继而影响认知功能[2]。外周神经阻滞可抑制手术创伤与疼痛引起的应激反应[3],股神经阻滞对术后炎性反应和POCD的影响目前尚未见报道。本研究拟观察股神经阻滞对老年膝关节置换术后认知功能及炎性反应的影响。
1 资料与方法
1.1一般资料
本研究经西安交通大学第二附属医院伦理委员会批准,并由患者或近亲属签署知情同意书。选择择期因膝关节骨性关节炎行单侧膝关节置换老年患者80例, ASAⅠ或Ⅱ级,年龄65-78岁,体重57-74 kg。排除标准:患有下肢外周神经疾病者;视、听觉障碍者;手术时间超过2 h。按照随机数字表法分为两组,单纯全麻组和股神经阻滞复合全麻组,每组各40例。
1.2麻醉方法
1.2.1麻醉实施无术前用药,所有患者均采用气管插管麻醉,监测NBP、HR、SPO2、ECG、PETCO2。N组于诱导前在神经刺激仪(宝雅,德国)定位下行股神经阻滞。患者仰卧,患肢外展在腹股沟韧带处触及股动脉搏动,股动脉搏动外侧1.0-1.5 cm作为穿刺点。穿刺点消毒连接,刺激仪初始电流1 mA,频率1 Hz,神经刺激针(宝雅,德国)向头端以45°刺入皮肤,当股四头肌出现典型收缩后,下调刺激仪电流至0.3 mA时仍见股四头肌收缩运动,注入0.4%罗哌卡因(批号:MA1796)25 ml。注药时先预注5 ml,再增大电流不见股四头肌运动,表明局麻药已在股神经周围浸润,随后继续注药。神经阻滞10 min后出现支配区域感觉与运动功能减退为阻滞有效。麻醉诱导:咪达唑仑0.05 mg/kg,舒芬太尼0.1-0.5 μg/kg,丙泊酚1.5 mg/kg,顺阿曲库铵0.2 mg/kg,气管插管后机械通气,氧流量1.5-2.0 L/min,VT 8-10 ml/kg,RR 10-12次/min, 维持PETCO235-45 mmHg。麻醉维持:吸入七氟醚1.0%,静脉输注丙泊酚2-6 mg/(kg·h)、瑞芬太尼0.1-0.5 μg/(kg·min)。维持BIS 45-55之间。
1.2.2术后管理术毕患者送麻醉恢复室(PACU)。所有患者均给予静脉自控镇痛(PCIA),配方:舒芬太尼100 μg+托烷司琼10 mg+生理盐水至100 ml,背景速度2 ml/h,自控追加量0.5 ml/次,锁定时间15 min。
1.3观察指标
①记录术前、术后1 d、术后7 d的MMSE评分,MMSE满分30分,同一患者术后MMSE评分较术前MMSE评分差值低2分以上表明发生了POCD[4];②记录术前(T1)、术后1 h(T2)、24 h(T3)、72 h(T4)外周血IL-6、CRP水平;③术后6 h、12 h、24 h进行视觉模拟疼痛(VAS)评分 。本研究由同一手术小组采用相同的手术方式完成手术。MMSE评分由经过培训的专人在评估日的8∶00-9∶00完成测试。POCD的判断参考郑羡河等[5]的研究。
1.4统计分析

2 结果
2.1一般情况
所有患者均完成研究,两组患者年龄、性别构成、体重、受教育程度比较差异无统计学意义(P>0.05)。与全麻组比较,股神经阻滞复合组丙泊酚和瑞芬太尼用量减少(P<0.05,见表1)。
表1两组患者一般情况比较及药物用量比较
Table 1Comparison of general clinical data and dosage between two groups
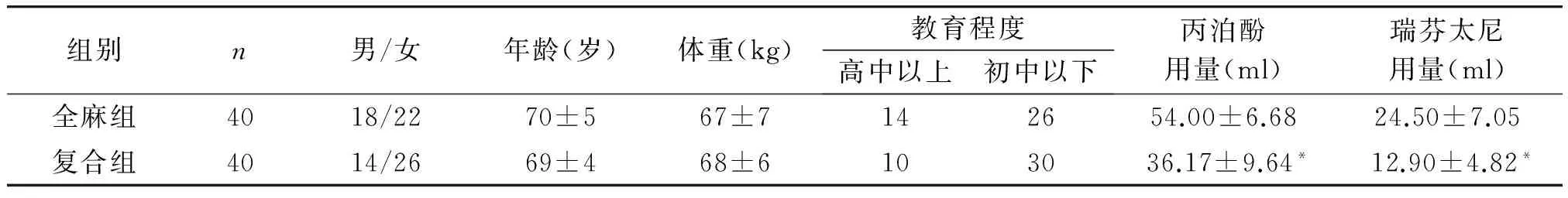
组别n男/女年龄(岁)体重(kg)教育程度高中以上初中以下丙泊酚用量(ml)瑞芬太尼用量(ml)全麻组4018/2270±567±7142654.00±6.6824.50±7.05复合组4014/2669±468±6103036.17±9.64*12.90±4.82*
与全麻组比较,*P<0.05;丙泊酚1 ml相当于10 mg,瑞芬太尼1 ml相当于50 μg
2.2两组血清IL-6和CRP比较
与T1时比较,两组患者血清CRP在T3、T4时均显著升高(P<0.05);与全麻组比较,股神经阻滞复合组CRP水平在T3、T4时显著降低(P<0.05)。与T1时比较,两组患者血清IL-6在T3时均显著升高(P<0.05),全麻组血清IL-6在T2时较T1时显著升高(P<0.05);与全麻组比较,股神经阻滞复合组IL-6水平在T2、T3时显著降低(P<0.05,见表2)。
表2两组患者不同时点血清IL-6、CRP水平比较
Table 2Comparison of IL-6 and CRP between two groups at different time points

指标组别T1T2T3T4CRP(mg/L)全麻组1.81±0.921.39±0.76171.66±71.45#162.59±48.04#*复合组1.46±0.851.69±0.89166.73±41.10#40.63±14.24#*IL-6(pg/ml)全麻组24.77±1.5933.35±8.01#42.03±5.30#26.48±2.32复合组25.02±1.8424.88±0.85*35.35±3.22#*25.24±1.29
与全麻组比较,*P<0.05;与T1时比较,#P<0.05
2.3患者MMSE评分
两组患者术后1dMMSE评分较术前1d显著降低(P<0.05),术后1 d全麻组MMSE评分明显低于股神经阻滞复合组(P<0.05)。其中,股神经阻滞复合组有8例(20.0%)发生POCD比全麻组的20例(50.0%)少(P<0.05)。术后7 d两组患者的MMSE评分与术前比差异无统计学意义,但两组分别仍有6例(15.0%)和2例(5.0%)患者发生POCD(见表3)。
2.4镇痛效果
术后6 h及12 h全麻组VAS评分高于股神经阻滞复合组(P<0.05,见表4),而术后24 h两组间差异无统计学意义。



组别术前1d术后1d术后7d全麻组26.70±2.3020.90±3.60#23.55±3.12复合组27.20±2.2123.30±2.98#*25.05±2.35
与全麻组比较,*P<0.05;与术前1天比较,#P<0.05


组别6h12h24h静息活动静息活动静息活动全麻组6.3±1.67.5±1.56.5±1.97.4±1.84.9±1.54.3±1.7复合组1.6±0.3*4.4±0.7*2.0±1.1*4.9±2.1*5.8±1.15.4±1.1
与全麻组比较,*P<0.05
3 讨论
外周炎性反应通过直接或间接途径可以引起中枢神经系统炎性反应。中枢神经系统炎性反应通过氧化与硝酸化应激损害神经元,氧化与硝酸化应激能引起细胞线粒体的损伤,而这种损伤被认为是神经元损伤的主要通路和关键环节[6,7]。与学习记忆密切相关的海马区域的过度炎性反应可引起神经元突触链接受损[8];长时程增强(LTP)是与学习记忆密切相关的生理现象,研究提示海马区高水平炎性因子伴有LTP受抑制[9]。IL-6是重要的炎性因子,IL-6可抑制LTP、改变海马神经元形态、抑制突触可塑性而致认知功能受损[10],研究提示高水平IL-6可导致认知功能短期受损[11,12]。CRP作为体内重要的急性相反应蛋白,它的水平反映了炎性反应的程度[13]。有学者[14]在研究急性肾损伤时中枢炎症因子的变化与认知功能改变关系时发现大鼠的大脑运动协调性等功能降低伴随着CRP和炎症因子的明显增加。有学者[15]研究认为CRP与老年手术患者认知功能减退有明确相关性。在老年髋部手术患者的研究中证实高CRP水平与术后早期认知功能下降有关[16]。本研究中,两组患者T3时炎性反应水平较T1时显著升高,且麻醉诱导前行股神经阻滞的复合组患者在T3时IL-6、CRP水平较全麻组显著降低,而两组患者的MMSE评分也呈现相似变化,说明不同麻醉处理因素造成的炎性反应水平和认知功能变化不同。
过度疼痛可引起机体大量炎性因子的释放,膝关节置换手术创伤应激大,术后疼痛严重,且是中至重度的疼痛[17]。手术创伤前有效的股神经阻滞可阻断手术切口处痛觉传导,降低中枢敏化,进而达到镇痛作用[18]。本研究提示:复合组患者术中麻醉药物用量明显减少,术后早期疼痛程度明显降低。股神经阻滞产生超前镇痛、术中麻醉、术后镇痛作用降低了手术创伤和疼痛刺激,从而减轻了术后炎性反应。复合组患者术后POCD发生率也明显低于全麻组,提示股神经阻滞有助于降低全麻下老年膝关节置换患者POCD的发生。
[1]Hu Z,Ou Y,Duan K,etal.Inflammation:a bridge between postoperative cognitive dysfunction and Alzheimer’s disease[J].Med Hypotheses,2010,74(4):722-724.
[2]宋杰,姜秀丽,杜伯群,等.帕瑞昔布钠对老年腹腔镜手术患者炎性因子及认知功能的影响[J].国际麻醉学与复苏杂志,2015,36(6):493-495.
[3]Demirel I,Ozer AB,Duzgol O,etal.Comparison of unilateral spinal anesthesia and L1paravertebral block combined with psoas compartment and sciatic nerve block in patients to undergo partial hip prosthesis[J].Eur Rev Med Pharmacol Sci,2014,18(7):1067-1072.
[4]姜维,胡远,孙云云,等.依达拉奉对老年患者围术期炎性反应及术后认知功能障碍的影响[J].临床麻醉学杂志,2014,30(10):961-93.
[5]郑羡河,蒋宗明,张昌锋,等.帕瑞昔布钠超前镇痛对老年病人术后认知功能的影响[J].中华麻醉学杂志,2011,31(3):310-312.
[6]Di FM,Chiasserini D,Tozzi A,etal.Mitochondria and the link between neuroinflammation and neurodegeneration[J].J Alzheimers Dis,2010,20(Suppl 2):s369-379.
[7]Gubellini P,Picconi B,Di FM,etal.Downstream mechanisms triggered by mitochondrial dysfunction in the basal ganglia:from experimental models to neurodegenerative diseases[J].Biochim Biophys Acta,2010,1802(1):151-161.
[8]Di FM,Chiasserini D,Gardoni F,etal.Effects of central and peripheral inflammation on hippocampal synaptic plasticity[J].Neurobiol Dis,2013,52:229-236.
[9]Zhu J,Jiang X,Shi E,etal.Sevoflurane preconditioning reverses impairment of hippocampal long term potentiation induced by myocardial ischaemia-reperfusion injury[J].Eur J Anaesthesiol,2009,26(11):961-968.
[10]McAfoose J,Baune BT.Evidence for a cytokine model of cognitive function[J].Neurosci Biobehavi Rev,2009,33(3):355-366
[11]Li YC,Xi CH,An YF,etal.Perioperative inflammatory response and protein S-100beta concentrations-relationship with postoperative cognitive dysfunction in elderly patients[J].Acta Anaesthesiol Scand,2012,56(5):595-601.
[12]Hudetz JA,Gandhi SD,Iqbal Z,etal.Elevated postoperative inflammatory biomarkers are associated with short-and medium-term cognitive dysfunction after coronary artery surgery[J].J Anesth,201l,25(1):1-9.
[13]Esme H,Kesli R,Apiliogullari B,etal.Effects of flurbiprofen on CRP TNF-α IL-6 and postoperative pain of thoracotomy[J].Int J Med Sci,2011,8(3):216-221.
[14]Liu M,Liang Y,Chigurupati S,etal.Acute kidney injury leads to inflammation and function changes in brain[J].J Am Soc Nephrol,2008,19(7):1360-1370.
[15]Gunstad J,Bausserman L,Paul RH,etal.C-reactive protein,but not homocysteine,is related to cognitive dysfunction in older adults with cardiovascular disease[J].J Clin Neurosci,2006,13(5):540-546.
[16]Beloosesky Y,Hendel D,Weiss A,etal.Cytokines and creactive protein production in hip-fracture-operated elderly patients[J].J Gerontol,2007,62A:420-6.
[17]Ng FY,Chiu KY,Yan CH,etal.Continuous femoral nerve block versus patient-controlled analgesia following total knee arthroplasty[J].J Orthop Surg(Hong Kong),2012 ,20(1):23-26.
[18]Frerichs J,Janis L.Preemptive analgesia in foot and ankle surgery[J].Clin Podiatr Med Surg, 2003,20(2):237-256.
Effects of femoral nerve block on postoperative inflammation response and cognitive function in elderly patients undergoing total knee arthroplasty
LUO Zhenguo1, XIAO Li1, WU Gang2, DONG Buhuai1, LÜ Jianrui2, XUE Rongliang2*
(1DepartmentofAnesthesiology,HonghuiHospitalofXi’anJiaotongUniversityMedicalCollege,Xi’an710054,China;2DepartmentofAnesthesiology,SecondAffiliatedHospitalofXi’anJiaotongUniversity;*Correspondingauthor,E-mail:xuerl299@163.com)
ObjectiveTo investigate the effects of femoral nerve block on postoperative inflammation response and cognitive function in elderly patients undergoing total knee arthroplasty under general anesthesia.MethodsEighty ASAⅠor Ⅱ patients, aged 65-78 years, scheduled for elective total knee arthroplasty under general anesthesia, were randomly divided into two groups(n=40 in each group): general anesthesia group and general anesthesia combined femoral nerve block group(combination group). Operations were performed under general anesthesia with endotracheal tube. Patients received nerve block guided by nerve stimulator before induction of anesthesia in combination group. The blood samples were collected after anesthesia induction(T1),1 h(T2),24 h(T3) and 72 h after operation(T4) to determine serum concentrations of C-reactive protein(CRP) and IL-6.Cognitive function was also evaluated at 1 d before surgery and 1 d, 7 d after surgery by mini-mental state examination(MMSE). The incidence of postoperative cognitive dysfunction(POCD) was recorded.ResultsThe levels of IL-6 and CRP in both two groups were significantly increased at 1 d after operation compared with before surgery(P<0.05).Compared with general anesthesia group, the concentrations of CRP and IL-6 were significantly reduced at 24 h after operation in combination group(P<0.05).The MMSE scores declined at 1 d after operation in both groups, and the MMSE scores were lower in general anesthesia group(P<0.05).The incidence of POCD was significantly higher in general anesthesia group than in combination group at 1 d after operation(50.0%vs20.0%,P<0.05).ConclusionFemoral nerve block can reduce the postoperative inflammation response and the incidence of POCD in elderly patients undergoing total knee arthroplasty.
femoral nerve block;aged;inflammation response;postoperative cognitive dysfunction
罗振国,男,1977-11生,硕士,副主任医师, E-mail:icewater511@sina.com
2015-12-05
R614
A
1007-6611(2016)03-0293-04
10.13753/j.issn.1007-6611.2016.03.022

