脑囊虫病手术治疗对策探讨(附6例病例)
温玉星,郑诗豪,黄绍崧,林 伟
脑囊虫病手术治疗对策探讨(附6例病例)
温玉星,郑诗豪,黄绍崧,林 伟
目的根据脑囊虫病的特征,探讨手术治疗对策。方法对神经外科收治的6例脑囊虫病患者,根据不同病情特征,应用不同手术对策治疗,观察术后疗效。结果6例患者经不同手术治疗1年后随访观察,除1例因脑积水需再次行脑室-腹腔分流术外。其余患者均获手术成功,且恢复情况良好,一直未出现新的神经损害症状。结论6例患者,根据不同病情特征,应用不同手术治疗对策,有效消除了脑囊虫病的并发症和致残,值得今后同行手术借鉴和参考。
脑囊虫病;诊断;治疗
囊虫病是由猪肉绦虫的幼虫(囊尾蚴)寄生于人体引起的疾病,它比成虫引起的猪肉绦虫病危害性更大[1]。囊尾蚴可以寄生于人体的不同组织器官,其中以脑组织最为常见。主要寄生于脑实质、脑室、蛛网膜下腔和各脑底池中,引发癫痫[2]、头痛、颅高压、精神障碍、脑膜炎、记忆力下降等症状。由于患者的临床表现复杂多样,轻者可无任何症状,重者可引起重度神经功能障碍[3-4]。过去,福建省的仙游、龙海等沿海地区囊虫病极为多见。改革开放后,随着居民个体散养猪的减少和人们卫生意识水平提高,该病发病率已在逐年下降,致使当前大多数医务人员特别是年青医务人员,缺乏对此病手术治疗的对策。为此,我们特将本院2010年至2017年收治的6例脑囊虫病进行了手术治疗对策的探讨。
1 材料与方法
1.1材料 6例囊虫病患者,均通过手术及病理确诊。其中男性4例,女性2例。年龄12~63岁。农村患者5例,城镇患者1例。均有囊虫病感染史。
1.2临床症状 有头痛、头晕、恶心、呕吐者4例,有癫痫发作病史3例,有皮下结节者2例,有肢体活动障碍、肌力下降者2例,有视物模糊者1例。详见表1。
1.3影像学诊断 6例患者术前磁共振(MRI)检查均清晰显示囊虫病灶周围,具有水肿带的典型特征,有2例在囊壁内侧可见囊虫头节。6例中病灶位于脑实质型4例,侧裂池1例,侧脑室1例。
1.4实验室检查 6例患者中,5例血清或脑脊液囊虫酶联免疫吸附试验阳性,其中血清检查4例阳性,脑脊液检查5例阳性;血常规检验,嗜酸性粒细胞增高者5例;粪便检出绦虫卵者1例。详见表2。
1.5手术治疗对策 一是脑实质囊虫摘除术,二是脑室、脑池囊虫摘除术。
表1 6例脑囊虫患者基本情况
Tab.1 The basic features of 6 patients with cerebral cysticercosis
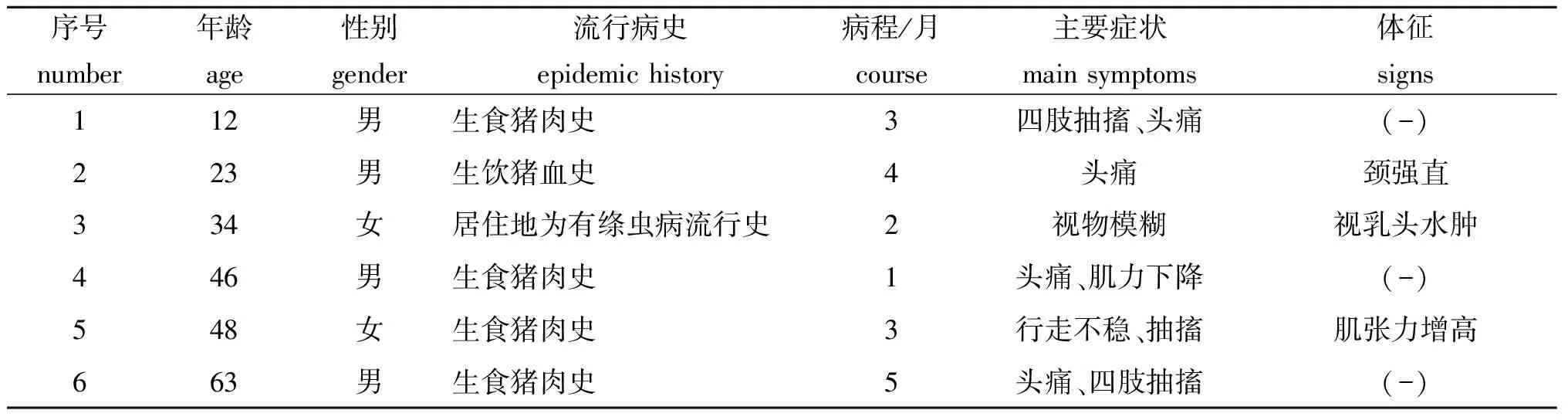
序号number年龄age性别gender流行病史epidemichistory病程/月course主要症状mainsymptoms体征signs112男生食猪肉史3四肢抽搐、头痛(-)223男生饮猪血史4头痛颈强直334女居住地为有绦虫病流行史2视物模糊视乳头水肿446男生食猪肉史1头痛、肌力下降(-)548女生食猪肉史3行走不稳、抽搐肌张力增高663男生食猪肉史5头痛、四肢抽搐(-)
表2 6例脑囊虫患者实验室检查
Tab.2 Laboratory examinations of 6 patients with cerebral cysticercosis
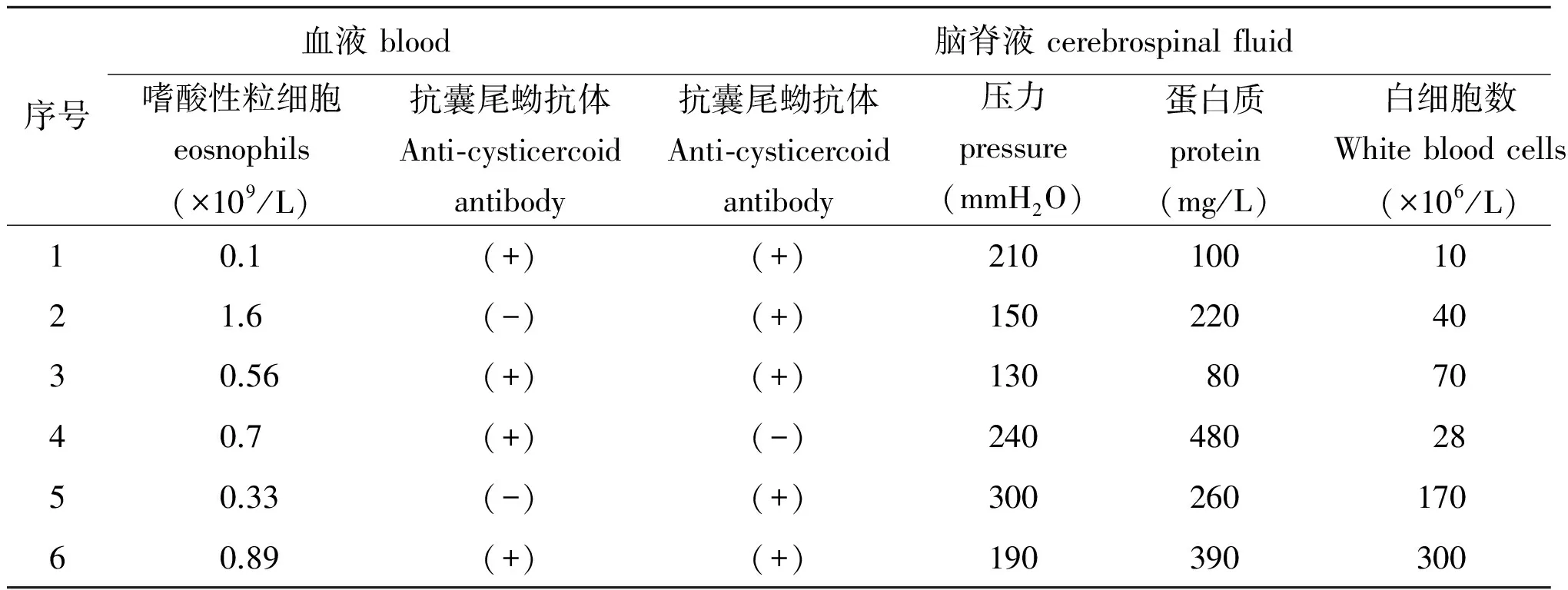
序号血液blood脑脊液cerebrospinalfluid粪便feces嗜酸性粒细胞eosnophils(×109/L)抗囊尾蚴抗体Anti⁃cysticercoidantibody抗囊尾蚴抗体Anti⁃cysticercoidantibody压力pressure(mmH2O)蛋白质protein(mg/L)白细胞数Whitebloodcells(×106/L)虫卵Ova10.1(+)(+)21010010-21.6(-)(+)15022040-30.56(+)(+)1308070-40.7(+)(-)24048028-50.33(-)(+)300260170+60.89(+)(+)190390300-
2 结 果
6例患者中4例行脑实质囊虫摘除术,2例行脑室、脑池囊虫摘除术。术后4例患者症状消失,2例患者症状改善。均无严重并发症。患者术后再经规范囊虫药物治疗6-36个月后随访结果,除1例患者偶尔出现癫痫症状,后经抗癫痫药物治疗很快得到控制,另2例出现脑积水,再行脑室腹腔分流术,脑室系统也已接近正常。
3 讨 论
猪肉绦虫成虫寄生在肠道引起的疾病,称为猪肉绦虫病,其幼虫引起的疾病为猪囊尾蚴病,主要侵犯运动较多的肌肉内,亦可侵犯脑、眼、心脏等重要器官,其中脑囊尾蚴病是最常见的一种。人体感染囊尾蚴的途径,分内源性(亦称自身感染)与外源性感染(亦称异体感染)两种。内源性感染,是因患者恶心、呕吐,引起肠道逆蠕动,致使寄生在肠道的成虫孕节,返流入胃或十二指肠,这时孕节中的大量成熟虫卵,经消化后孵出六钩蚴,侵入肠壁血管或淋巴管随血液或淋巴液而扩散,这种自身感染的囊虫病,其危害性远远大于外源性感染。外源性感染,是因食入被虫卵污染的食物所致,由于食入的虫卵有限,故引起的囊虫病灶数量不多,危害也相对较小。
侵入脑部的囊虫所引起的脑囊虫病,临床最常见的症状是癫痫,发生率约60%~80%,其发作形式、程度及频率与囊虫数目、寄生部位密切相关,少数患者可出现癫痫持续状态。尤其当囊尾蚴死亡后,分解出的异体蛋白,可加重癫痫发作;其次是头痛,但脑囊虫病引起的头痛症状缺乏特异性;再次为颅内压增高,是因脑水肿引起,它多见于侧脑室、第三或第四脑室脑囊虫患者[6]。当囊虫侵犯第四脑室时还可引起Brun综合征[7],这时患者一旦改变头位,即可引发小脑扁桃体下疝,致头晕、呕吐、神志不清甚至心跳呼吸骤停,值得高度警惕。对于言语障碍、肢体乏力等症状多与相应神经功能支配区域受累有关。
血清和脑脊液免疫学检验有助于脑囊虫病的诊断。头部CT和MRI检查对脑囊虫的诊断有重要意义,CT对于囊虫钙化病灶的诊断优于MRI,但MRI对于早期脑囊虫病的定性、定位及分布情况的诊断明显优于CT[9]。头颅MRI对软组织内的囊虫显影清晰,可根据其分布部位、大小、囊壁厚薄、头节是否存在,将其分为活虫期、退变死亡期和钙化期等[10]。
目前对于囊虫病的治疗药物是吡喹酮和阿苯哒唑。其中吡喹酮杀虫效果明显,能使囊虫在短时间内大量死亡,但缺点是其分解产物给患者带来严重副反应,引起癫痫持续发作、颅内压增高、甚至脑疝危及生命,因此,对于囊虫病灶多者必须与激素联用。阿苯达唑药物作用温和,在脑脊液中渗透性好,且不与其他药物相互作用[11]。总之,在使用抗虫药物杀虫时,除应严格把控适应症外,还要积极应用皮质激素、脱水药物、抗癫痫药物等,以减轻不良副反应。
脑囊虫的手术治疗,主要用于药物治疗无效、有严重神经症状的脑实质囊虫病和脑室系统内囊虫病,其目的是为了摘除囊虫,解除脑积水、缓解颅高压危象[12]。手术治疗对策包括双侧颞肌减压术、脑脊液分流术及脑室内囊虫摘除术[15]。
[1] Jacome SE, Correa DE, Martinez BB, et al. Neurocysticercosis a public health problem[J]. Clin Case Rep, 2017, 5(4): 543-544.
[2] Gripper LB, Welburn SC. The causal relationship between neurocysticercosis infection and the development of epilepsy - a systematic review[J]. Infect Dis Poverty, 2017, 6(1): 31.
[3] Cheng JH, Man EM, Luk SY, et al. Neurocysticercosis: diagnostic dilemma[J]. Hong Kong Med J, 2016, 22(6): 616-618.
[4] Gripper LB, Welburn SC. Neurocysticercosis infection and disease-A review[J]. Acta Trop, 2017, 166: 218-224.
[5] Burneo JG, Cavazos JE. Neurocysticercosis and epilepsy[J]. Epilepsy Curr, 2014, 14(1 Suppl): 23-28.
[6] Leon A, Saito EK, Mehta B, et al. Calcified parenchymal central nervous system cysticercosis and clinical outcomes in epilepsy[J]. Epilepsy Behav, 2015, 43: 77-80.
[7] Del BO. Clinical management of neurocysticercosis[J]. Expert Rev Neurother, 2014, 14(4): 389-396.
[8] Sciutto E, Cardenas G, Adalid-Peralta L, et al. Human neurocysticercosis: immunological features involved in the host’s susceptibility to become infected and to develop disease[J]. Microbes Infect, 2013, 15(6/7): 524-530.
[9] Zammarchi L, Bonati M, Strohmeyer M, et al. Screening, diagnosis and management of human cysticercosis and T. solium taeniasis: Technical recommendations by the COHEMI project study group[J]. Trop Med Int Health, 2017,22(7):881-894.
[10] Song Z, Chen X, Tang Y, et al. Magnetic resonance three dimensional sampling perfection with application optimized contrasts using different flip angle evolution sequence for obstructive hydrocephalus: impact on diagnosis and surgical strategy modification[J]. Chin J Surg, 2015, 53(11): 860-864.
[11] Ruiz-Olmedo MI, Gonzalez-Hernandez I, Palomares-Alonso F, et al. Effect of nitazoxanide on albendazole pharmacokinetics in cerebrospinal fluid and plasma in rats[J]. Saudi Pharm J, 2017, 25(3): 413-418.
[12] Dhamne M, Hui AC, Kurukularatne C. The role of surgery in the management of neurocysticercosis[J]. Hong Kong Med J, 2016, 22(6): 624.
[13] Bu XY,Liu M,Zhang JG,et al. Surgical treatment of brain cysticercosis patients with hydrocephalus[J].Henan Med Res,2009(03):193-195. (in Chinese)
步星耀,刘猛,张建国,等.脑积水型脑囊虫病的外科手术治疗研究[J].河南医学研究,2009(03):193-195.
[14] An CX,Li Q,Liang WT,et al. Clinical analysis of neuroendoscopy treatment of the third ventricle cysticercosis[J].Chin J Endosc,2016(07):94-97. (in Chinese)
安彩霞,李强,粱文涛,等.神经内镜治疗第三脑室囊虫病的临床分析[J].中国内镜杂志,2016(07):94-97.
[15] Carpio A, Romo ML. Should calcified neurocysticercosis lesions be surgically removed?[J]. Epilepsia, 2014, 55(2): 379.
Diagnosisandtherapyofcerebralcysticercosiswith6casereportsattached
WEN Yu-xing, ZHENG Shi-hao, HUANG Shao-song, LIN Wei
(DepartmentofNeurosurgery,FujianProvincialHospital,Fuzhou350001,China)
We explored the feature and therapeutic methods of cerebral cysticercosis. The effect of different surgical treatment was analyzed on 6 patients with cerebral cysticercosis who had undergone surgery at Fujian Provincial Hospital.Results showed that 2 of 6 cases underwent an excision of ventricle or cisternalcysticercus. Three cases were performed an excision of brain parenchyma cysticercus. The decompressivecraniectomy under bilateral temporalis was performed on 1 patient with cerebral cysticercosis. One case underwent ventriculo-peritoneal shunt because of hydrocephalus after a year of follow-up. The operations of 6 cases were all successfully performed. All patients recovered well after the operation. No newly neurobiological injuries were observed. Timely and accurate neurosurgery contributes to reduce the incidence of complications and cut down disability rate of cerebral cysticercosis, and buy time and fight for an opportunity for drug therapy of cerebral cysticercosis as well. It significantly improves the safety and therapeutic effect of anti-cysticercosis drugs.
cerebral cysticercosis; diagnosis; therapy
10.3969/j.issn.1002-2694.2017.10.019
福建省立医院神经外科,福州 350001
383
A
1002-2694(2017)10-0943-03
2017-06-14编辑李友松