Should we have a guard against therapeutic nihilism for patients with severe traumatic brain injury?
Many clinicians would agree that a vegetative outcome is a fate worse than death after a severe traumatic brain injury (TBI). In an effort to avoid poor outcomes of this nature, neurotrauma practitioners draw from their training and experience to make the monumental decision of when to recommend against aggressive care in severe TBI patients. Such judgements are,unfortunately and invariably, subjective with an inherent risk of depriving a patient of a reasonable chance of a good outcome. Substantially adding to this complexity is the fact that questions like “What is an acceptable outcome?” and “What is a reasonable chance of an acceptable outcome?” are highly personal and at least as philosophical as they are medical. We have found great variation in practitioner aggressiveness in different regions and even within the same department of a single hospital. Issues surrounding aggressiveness in severe TBI patients and variability in aggressiveness have been the subject of remarkably little study when considering the high frequency and the marked consequences of these decisions. Indeed, we are increasingly certain about what constitutes best care (Thomas et al., 2000; Carney et al., 2017) but we have very little guidance about when it is appropriate or not to apply best care in the most severely injured patients.
As our ability to accurately prognosticate outcome from severe TBI improves it is possible and important to discuss what constitutes therapeutic nihilism in a more objective fashion.The International Mission for Prognosis and Clinical Trial Design in Traumatic Brain Injury (IMPACT) and Corticosteroid Randomization after Significant Head Injury (CRASH)prognostic models have been a major advance in our ability to predict patient outcomes early after TBI (MRC CRASH Trial Collaborators et al., 2008; Steyerberg et al., 2008). It is,however, the opinion of the authors that even if 100% accurate these calculators could never serve as a basis for withdrawal of care decisions by themselves. At this point, though, the models could serve to protect patients by helping to guard against inappropriate nihilism – perhaps by mandating the agreement of a second physician before withdrawing care if a sufficiently favorable outcome is predicted. In a recently published study our group began exploring these ideas by performing a survey of neurotrauma practitioners and assessing what they might judge to constitute nihilism (Letsinger et al., 2017). Ultimately we found robust agreement that aggressive care should generally be pursued in patients less than 76 years of age and greater than a 15% chance of survival or good outcome if predicted by a model that is 100% accurate.
Futility, nihilism and reputation:Decisions to limit treatment of patients with severe acute neurological injuries are ethical when it would simply prolong patient suffering or when it would lead to an outcome that the patient would judge to be unacceptable. Restricting care in these circumstances also prevents the high cost of medical care which will ultimately be of insufficient benefit and it frees up resources for individuals who will benefit more from them. Unfortunately there is often great uncertainty as to what outcome might be achieved with aggressive care even despite recent advances in TBI prognostication. Indeed, these prediction models remain imperfect as they are based on a limited amount of objective data collected early after the injury. As such great caution is needed in applying the predictions to individual patients. Obviously, if it could be known for sure that a patient was not going to benefit sufficiently from aggressive treatment then futile care could be easily avoided.
Distinct from this is the notion of therapeutic nihilism.Nihilism is an inappropriately pessimistic view of a patient’s outcome and the ability of a patient to benefit from aggressive care. This can deprive patients of the chance of an outcome that would be acceptable to them and what they judge to be a reasonable chance of attaining that outcome.
An additional scenario problematic in modern medicine is the influence of performance in national hospital rankings. An unintended consequence of these rankings can be a decision to avoid aggressive care in patients with a high chance of a poor outcome which would adversely affect rankings. Public rankings are intended to promote the best care of patients but in this fashion they can have the opposite effect.
Self-fulfilling prophecies:In considering nihilism and level of care decisions following severe TBI it is critical to understand how the expectation of a poor outcome can become a self-fulfilling prophecy. This fallacy can occur when the prediction of an event becomes reality simply by virtue of having been predicted. Said differently – subjecting a patient to suboptimal care because it is believed they may not benefit from care has the potential to secure a poor outcome even if a good one could have been achieved. This idea was capably discussed by Hemphill and White who provided a hypothetical scenario of 100 patients with severe stroke in which 70 die. If the death of 70% of these patients was preceded by withdrawal of support,despite some having the capacity to survive if support was maintained, then the true mortality rate would actually be lower (Hemphill and White, 2009). In severe neurological injuries such as TBI, in order for a patient to achieve a good outcome they must first survive, of course. If support is withdrawn early after injury and the patient dies, it is impossible to determine whether or not this was inevitable. This phenomenon can also cloud our ability to accurately understand the natural history of severe insults. It is, of course, hoped that the self-fulfilling prophecy fallacy will not rob a patient of a reasonable chance of an acceptable outcome. An accurate prediction model and a protocol to protect against nihilism could help to protect patients from therapeutic nihilism secondary to biased or inaccurate outcome predictions.
Physician autonomy and ability to predict outcome from TBI:Subjecting physicians to a guard against nihilism would likely bring about objections for a variety of reasons, not the least of which is the fact that it would infringe upon the autonomy of highly trained, skilled and experienced care providers.An important consideration in this issue, however, is that evidence to date suggests that physicians are unable to prognosticate accurately following TBI and that their judgements tend to be excessively pessimistic.
Moore et al. (2013) found evidence for variation and systemic bias in clinicians’ perceptions of prognosis following brain injury. It was concluded that the predictions of clinical experts following traumatic brain injury are widely variable and systemically pessimistic compared to the IMPACT prognostic model, which uses objective data such as patient age, motor score, and other physical exam and imaging findings in prognostication. The study found that on average, clinicians estimated a 16.3% greater probability of death than the IMPACT calculator. Indeed, physicians often overlooked important variables strongly associated with outcome such as blood glucose level and type of hematoma (subduralvs.extradural).
A study by Kaufmann et al. (1992) also explored the ability of practitioners to accurately predict patient outcome. In this study, a neurosurgeon and a neuroradiologist examined 100 consecutive severely head-injured patients from the surgical intensive care unit and made outcome predictions. The predictions were made according to a contracted Glasgow outcome scale and were always made by the same experienced neurosurgeon and neuroradiologist. It was found that correct ‘firstday’ prognostic predictions were made in only 59% and 56% of cases by the neuroradiologist and neurosurgeon, respectively(Kaufmann et al., 1992). Additionally, the neurosurgeon consistently overestimated unfavorable outcomes. Interestingly,when the prognoses made by the neuroradiologist and neurosurgeon coincided, the accuracy of the prognoses increased from 56–59% to 73%. Nonetheless, even when both the clinical and radiologic prognosis predictions agreed, nearly 30% of initial prognoses were still incorrect.
In another study, Turgeon et al. (2013) sought to understand the attitudes of physicians caring for patients with severe TBI with respect to prognostication and clinical decision making.In a case-based scenario, a third of respondents to the study agreed, a third were neutral, and a third disagreed that patient prognosis would be unfavorable at one year (Turgeon et al.,2013). Additionally, only 10% were comfortable recommending withdrawal of life-sustaining therapy. This study further supports the notion that physician opinions regarding aggressiveness of care widely vary and are often pessimistic.
A related study of oncology patients by Randolph et al also demonstrated marked variability in physician opinion regarding patient care in critical situations (Randolph et al., 1999). In this study, hypothetical scenarios describing two critically ill oncology patients presenting to the intensive care unit (ICU)after initiating mechanical ventilation for acute respiratory failure were presented to pediatric intensivists and oncologists.Within these two scenarios, eight cases with varying probabilities of survival and parental preferences were presented to physicians for prognostication and decision making. In three out of the eight scenarios, ≥ 10% of respondents chose full aggressive management whereas another ≥ 10% chose comfort measures only. This is another example of the variability in physician prognostication and decision making in critically ill patients.

Figure 1 Implementation of the IMPACT TBI prognostic calculator into an electronic health record (EHR).In this work, the IMPACT TBI prognostic calculator was implemented directly into EpicCare® using a custom SmartForm, which allows for clinicians to complete the calculations at their preferred time within the workflow. Additionally, the sidebar report panel on the right side collates key patient data needed for the calculation including blood pressure, SpO2, motor score, pupil reactivity, hemoglobin and glucose level. The results of the calculation are placed into the patient note. This process allows for faster, more efficient calculations and documentation. IMPACT: International Mission for Prognosis and Clinical Trial Design in Traumatic Brain Injury; TBI: traumatic brain injury; SpO2: pulse oxygen saturation.
Making prognostic calculations more convenient:An impediment to the use of prognostic calculators, especially in the acute setting, can be the valuable time needed to gather the required data and enter it into an online calculator. Thus,our group worked to implement the IMPACT TBI prognostic calculator into the Epic® electronic health record (EHR)with the goal of creating a tool that could be completed more quickly and efficiently than the current online platform. The integration of the IMPACT TBI prognostic calculator within the EHR was done to account for clinician requests and with regard to both clinical decision support (CDS) ideals and existing EHR, EpicCare® (Epic Systems Corp., Verona, WI, USA)capabilities (Figure 1). The integrated calculator incorporates a sidebar report within the EHR which automatically collates information including blood pressure, pulse oxygen saturation(SpO2), Glasgow Coma Scale motor score, pupil reactivity, hemoglobin, glucose level, and a link to radiology reports needed for the calculation (Figure 1). Many unique and potentially effective ways exist for the inclusion of a web based prognostic calculator within the EHR, but specifically we chose to use a custom SmartForm. This choice had the bonus of being available directly within the NoteWriter, which allows for clinicians to complete the calculations at their preferred time within the workflow. Another feature of this integrated calculator is the ability to create ‘alerts’ which would advise that an opinion be obtained from a second physician. Also, the form can potentially be shared with other institutions using EpicCare®by creating their own custom SmartForm based upon this implementation. This implementation also serves as a potential inflection and launching point demonstrating the desire of clinicians for the integration of prognostic tools within the electronic health record and for companies, institutions and individuals providing CDS.
Additional work needed to develop a guard against inappropriate nihilism:We believe that a number of additional steps will be required before a guard against nihilism can be adopted into the clinical care of brain injured patients. In our initial publication we chose to assess thresholds for non-aggressive care based on a perfectly accurate prognostic calculator(Letsinger et al., 2017). We felt it was important to characterize the ideal scenario before introducing the added complexity of an imperfect prognostic model. A survey determining how imperfect prognostic calculations influence thresholds for non-aggressive care should be completed. It must also be considered that physician self-report likely differs from real-world behavior. We have thus initiated a study which will compare provider opinions on aggressiveness to their actual behavior.It will be important for physicians, ethicists and the public to debate the pros and cons of a nihilism guard – this may involve qualitative research strategies. Ultimately a clinical protocol will need to be proposed and tested. We suggest a model whereby an alert is generated by an EHR when an attempt is made to enter palliative care orders on a patient calculated to have an acceptable prognosis.
Conclusion:Prognostic models cannot replace the judgement of physicians. Recently developed and reasonably accurate prognostic models can help to more objectively define nihilism and to protect TBI patients from it, however. These models can also help to reduce variation in the aggressiveness of physicians caring for severe TBI patients. While physicians may object to a reduction in their autonomy, literature to date consistently demonstrates that predictions made by clinicians are inaccurate. This mandates the development of tools to assist with care limiting decisions. Here we propose a guard against therapeutic nihilism which, with further study, could ultimately protect patients from practitioners with excessively nihilistic views.
Ryan Hirschi, Casey Rommel, Gregory W. J. Hawryluk*
School of Medicine, University of Utah, Salt Lake City, UT, USA
(Hirschi R)
Department of Biomedical Informatics, School of Medicine,
University of Utah, Salt Lake City, UT, USA (Rommel C)
Department of Neurological Surgery, University of Utah, Clinical
Neurosciences Center, Salt Lake City, UT, USA (Hawryluk GWJ)
*Correspondence to:Gregory W. J. Hawryluk, M.D., Ph.D., FRCSC,gregory.hawryluk@hsc.utah.edu.
orcid:0000-0002-5604-7057 (Gregory W. J. Hawryluk)
How to cite this article:Hirschi R, Rommel C, Hawryluk GWJ (2017)Should we have a guard against therapeutic nihilism for patients with severe traumatic brain injury. Neural Regen Res 12(11):1801-1803.
Plagiarism check:Checked twice by iThenticate.
Peer review:Externally peer reviewed.
Open access statement:This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under identical terms.
Open peer review report:
Reviewer: Creed Stary, Stanford University School of Medicine, USA.
Comments to authors: The authors review the challenges of end-oflife decision making in patients with severe TBI and low probability of meaningful recovery. They highlight the risk of “therapeutic nihilism,”defined as “an inappropriately pessimistic view of a patient’s outcome and the ability of a patient to benefit from aggressive care,” and the risk that decision making within this context can be fall patients who would benefit from aggressive therapy. The Authors present prior work outlining algorithmic software available for the electronic medical record to help physicians avoid this pitfall and aid decision-making.
Carney N, Totten AM, O’Reilly C, Ullman JS, Hawryluk GW, Bell MJ,Bratton SL, Chesnut R, Harris OA, Kissoon N, Rubiano AM, Shutter L, Tasker RC, Vavilala MS, Wilberger J, Wright DW, Ghajar J(2017) Guidelines for the management of severe traumatic brain injury, fourth edition. Neurosurgery 80:6-15.
Hemphill JC 3rd, White DB (2009) Clinical nihilism in neuroemergencies. Emerg Med Clin North Am 27:27-37, vii-viii.
Kaufmann MA, Buchmann B, Scheidegger D, Gratzl O, Radü EW(1992) Severe head injury: should expected outcome influence resuscitation and first-day decisions? Resuscitation 23:199-206.
Letsinger J, Rommel C, Hirschi R, Nirula R, Hawryluk GWJ (2017)The aggressiveness of neurotrauma practitioners and the influence of the IMPACT prognostic calculator. PLoS One 12:e0183552.
Moore NA, Brennan PM, Baillie JK (2013) Wide variation and systematic bias in expert clinicians’ perceptions of prognosis following brain injury. Br J Neurosurg 27:340-343.
MRC CRASH Trial Collaborators, Perel P, Arango M, Clayton T,Edwards P, Komolafe E, Poccock S, Roberts I, Shakur H, Steyerberg E, Yutthakasemsunt S (2008) Predicting outcome after traumatic brain injury: practical prognostic models based on large cohort of international patients. BMJ 336:425-429.
Randolph AG, Zollo MB, Egger MJ, Guyatt GH, Nelson RM, Stidham GL (1999) Variability in physician opinion on limiting pediatric life support. Pediatrics 103:e46.
Steyerberg EW, Mushkudiani N, Perel P, Butcher I, Lu J, McHugh GS,Murray GD, Marmarou A, Roberts I, Habbema JD, Maas AI (2008)Predicting outcome after traumatic brain injury: development and international validation of prognostic scores based on admission characteristics. PLoS Med 5:e165; discussion e165.
Thomas L, Cullum N, McColl E, Rousseau N, Soutter J, Steen N (2000)Guidelines in professions allied to medicine. Cochrane Database Syst Rev:CD000349.
Turgeon AF, Lauzier F, Burns KE, Meade MO, Scales DC, Zarychanski R, Moore L, Zygun DA, McIntyre LA, Kanji S, Hébert PC, Murat V, Pagliarello G, Fergusson DA; Canadian Critical Care Trials Group (2013) Determination of neurologic prognosis and clinical decision making in adult patients with severe traumatic brain injury: a survey of Canadian intensivists, neurosurgeons, and neurologists. Crit Care Med 41:1086-1093.
- 中国神经再生研究(英文版)的其它文章
- The role of general anesthetics and the mechanisms of hippocampal and extra-hippocampal dysfunctions in the genesis of postoperative cognitive dysfunction
- Saponins from Panax japonicus attenuate age-related neuroinflammation via regulation of the mitogenactivated protein kinase and nuclear factor kappa B signaling pathways
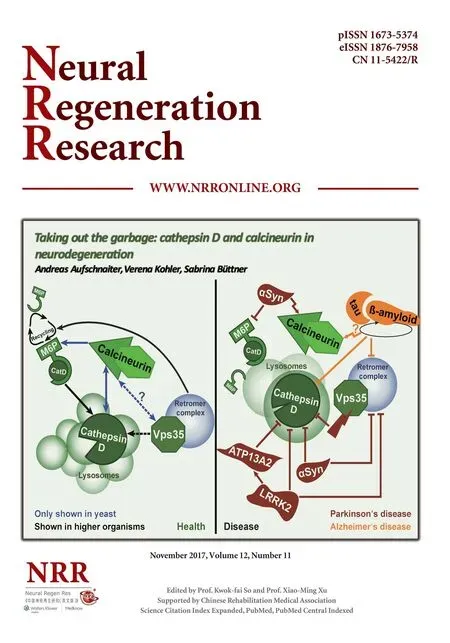
- Taking out the garbage: cathepsin D and calcineurin in neurodegeneration
- MicroRNAs as diagnostic markers and therapeutic targets for traumatic brain injury
- Interferon regulatory factor 2 binding protein 2: a new player of the innate immune response for stroke recovery
- Endogenous retinal neural stem cell reprogramming for neuronal regeneration