Therapeutic capacities of human and mouse skeletal muscle-derived stem cells for a long gap peripheral nerve injury
An overview of a long-gap peripheral nerve therapy:A longgap peripheral nerve transection injury is an irreparable injury to the living body, and mostly leads to permanent loss of related motor and sensory functions. In such long gap injuries,nerve end-to-end suture is physically impossible. Therefore,bridging a long nerve-gap is critical to re-establish adequate mechanical support for separated nerve ends, and prevent the diffusion of neurotrophic and neurotropic factors secreted by transected stumps (Deumens et al., 2010).
Autologous nerve grafts have been used as gold standard treatment (Deumens et al., 2010), with the expectation of proliferation and activation of graf t-associated Schwann cells,along with their production of neurotrophic factors and cytokines. However, the prognosis is not always favorable, despite the sacrifice of a healthy nerve graftfrom another unaffected normal body part.
Scaffold bridges, which can be of synthetic or biological origin and/or be resorbable or non-resorbable, have been studied with the hope that bridging conduits can provide sufficient mechanical support and concentration of neurotrophic/neurotropic factors. However, it appears clear that the use of these conduits alone does not sufficiently facilitate nerve regeneration across long gaps (Pfister et al., 2011).
Combinatorial use of acellular conduits with several cellular sources, such as Schwann cells and/or Schwann-like cells derived from cultivated bone morrow stromal cells (Dezawa et al., 2005), olfactory ensheathing cells (Radtke et al., 2011), and adipose tissue-derived cells (Kingham et al., 2007) have also been studied. However, these methods are unlikely to match or exceed the performance of autologous nerve grafts, whereas skeletal muscle-derived stem cells showed significantly higher performance than that of the autologous nerve graft(see next section).
Application of skeletal muscle-derived stem cells to the long-gap nerve injury:As an alternative method, we have reported the potential therapeutic use of mouse skeletal muscle-derived multipotent stem cells (Sk-MSCs) in long-gap nerve injury treatment by bridging using an acellular conduit(Tamaki et al., 2014), based on the original capacity of the Sk-MSCs as the synchronized reconstitution of the muscle-nerveblood vessel unit (Tamaki et al., 2005). As expected, transplanted mouse Sk-MSCs actively differentiated into all types of peripheral nerve support cells (Schwann cells and perineurial/endoneurial cells) and blood vessel-related cells (pericytes and vascular endothelial cells), and showed favorable numerical(the number of axons and myelin) and functional recoveries(Tamaki et al., 2014). A significant increase in the number of blood vessels was also observed, along with a potentially sufficient contribution of O2and nutrition supply and elimination of waste products, to enable faster recovery (Tamaki et al.,2014). These recovery achievements showed 2–3-fold higher scores than that of the reported gold standard treatment (Deumens et al., 2010), showing great promise in peripheral nerve therapy. However, this was a mouse study, and it was unclear whether human skeletal muscle included stem cells comparable to those in the mouse.
Recently, we also reported optimal methods for the therapeutic isolation and fractionation of human skeletal muscle-derived cells (Sk-Cs), and established appropriate cell expansion culture methods (Tamaki et al., 2015). Subsequently,we reported that human Sk-Cs also had stem cell potential for skeletal muscle and peripheral nerve-vascular lineage cells in severely damaged skeletal muscle (Tamaki et al., 2015), similar to mouse Sk-MSCs used previously (Tamaki et al., 2005,2007a, b). Therefore, it appeared that human Sk-Cs should be considered to be skeletal muscle-derived stem cells (Sk-SCs).
Sk-SCs have been isolated using various methods. However, regarding our cell isolation and fractionation method, the most important points are that 1) the muscle samples must not be minced before enzymatic treatment, 2) enzymatic treatment should be performed with as minimal effect protease/peptidase activity as much as possible, and 3) CD45, CD34,and CD29 should be used for cell sorting immediately after enzymatic isolation. We have consistently used this method throughout our mouse and human experiments, and obtained Sk-34 (CD45–/34+) and Sk-DN (CD45–/34–/29+) cells.
Then, we found that the mouse Sk-DN cells were situated hierarchically upstream of the Sk-34 cells, showing the identical differentiation and regenerative capacity as similar lineage cells (Tamaki et al., 2008). However, the human Sk-DN/29+and Sk-34 cells showed completely different differentiation and regenerative capacity. The Sk-DN/29+cells showed specific to myogenic differentiation/regeneration (probably mainly satellite cells), but the Sk-34 cells exerted multipotent differentiation into peripheral nerve and vascular cell lineages (Tamaki et al., 2015).
Further, we applied human Sk-34 and Sk-DN/29+cells to the long-nerve gap therapy study (Tamaki et al., 2016), strictly followed the previous mouse experiment protocol (Tamaki et al., 2014). The results clearly indicated that human Sk-34 cells showed comparable therapeutic capacities to those seen with the mouse Sk-MSCs, with regard to cell biology, tissue morphology, and physiology (Tamaki et al., 2016).
Comparison of the mouse Sk-MSCs and human Sk-SCs: The achievements of numerical, cell biological, and functional recoveries in cases of mouse Sk-MSCs (Tamaki et al., 2014) and human Sk-SCs (Sk-34 and Sk-DN/29+) (Tamaki et al., 2016)in long-gap nerve therapy are summarized inTable 1. The cell differentiation capacity of the mouse Sk-MSCs and the human Sk-34s are comparable, showing differentiation into peripheral nerve cells (Schwann cells and endoneurial/perineurial cells)and vascular cells (endothelial cells and pericytes). Favorable numerical recovery of the total number of axons and myelin is also similar, whereas an increase in the number of blood ves-sels was relatively higher in the mouse (7–9 foldvs.3–4 fold).Interestingly, significant numerical recovery of axon/myelin was also observed in Sk-DN cells (since they were clearly lower in number than those in the Sk-34 transplantation), whereas complete elimination of Sk-DN/29+cells occurred within 2–4 weeks after transplantation. In addition, an increase in the number of blood vessels was also evident (4–5 fold), associated with moderate functional recovery. Therefore, the paracrine effects of transplanted Sk-DN/29+cells during the first 2–4 weeks may have positively affected overall recovery, acting as an adjuvant for the repair of damaged nerve tissue.

Table 1 Comparison of numerical and functional recoveries and differentiation capacity of the mouse Sk-MSCs, human Sk-34, and human Sk-DN/29+ cells

Table 2 Paracrine capacity and expression of angiogenic cytokines
Several angiogenic paracrine factors were detected at the protein level in the three cell fractions, and these are summarized as paracrine capacity inTable 2. All three cell types showed active expression of angiogenesis-relating cytokines just before transplantation with only a few minor differences.Therefore, it is possible that the presence of these cytokines in the Sk-DN/29+cells may accelerate blood vessel formation during the early recovery phase, and lead to setup of a favorable oxygen/glucose environment in the nerve conduit. This also suggests the important observation that an appropriate treatment during the first 4 weeks after injury markedly affects subsequent numerical and functional nerve recovery. In fact,functional recovery of downstream muscle began at 2 weeks after surgery (Tamaki et al., 2016). Thus, this should be a consideration in future nerve injury therapy.
Elimination of skeletal muscle fiber formation in the peripheral nerve niche:Elimination of skeletal muscle cells,with an inhibition of maturation of the fibers, in the nerve regeneration niche has been also observed in the case of the mouse Sk-MSCs transplantation (Tamaki et al., 2014). In the mouse Sk-MSCs, it is impossible to separate myogenic cells and the other nerve-vascular cells, because of their clonal multipotency for muscle-nerve-vascular cell lineage (Tamaki et al.,2007b). Therefore, cell differentiation into three lineages begins together, but myogenic cell differentiation arrests during the first 2–3 weeks, probably owing to the lack of factors promoting differentiation into mature myofibers in the nerve specific niche (Tamaki et al., 2014). At least, myogenic capacity is not necessary for nerve regeneration, and preliminary separation of them is possible in the human case, and this is thought to be advantageous for therapeutic applications.
Prospect for therapeutic use:In terms of therapeutic application, we found that there were no differences in the differentiation/regenerative capacity of human Sk-SCs whether the muscle samples were obtained from the leg or abdominal muscles (Tamaki et al., 2015). Therefore, we propose that a small sample removal (around 3 g) from the abdominal wall muscle would allow donor cells to be obtained relatively easily and safely, with minimal sacrifice. In cases of open traumatic injury, sampling around the nerve-damaged site is also possible. For the nerve conduit, we presently think that an appropriate size vein, after acellular treatment by 70% ethanol,would be the best candidate. However, the use of an artificial biodegradable tube (probably polyglyconate and/or collagen)is less invasive and much better for the patient. However, further consideration/improvement, such as adjustable size, substance permeability, and physical tenderness of tubes, should be considered.
Conclusion:It is possible that human Sk-SCs have favorable properties similar to that of mouse Sk-MSCs in peripheral nerve regeneration therapy, when using our original cell isolation/fractionation/expansion method. Therefore, human Sk-SCs are a potential practical source for autologous stem cell therapy following severe nerve injury.
Tetsuro Tamaki*
Muscle Physiology & Cell Biology Unit, Department of Human Structure and Function, Tokai University School of Medicine, 143 Shimokasuya, Isehara, Kanagawa, Japan
*Correspondence to:Tetsuro Tamaki, tamaki@is.icc.u-tokai.ac.jp.
orcid:0000-0002-9071-049X (Tetsuro Tamaki)
How to cite this article:Tamaki T (2017) Therapeutic capacities of human and mouse skeletal muscle-derived stem cells for a long gap peripheral nerve injury. Neural Regen Res 12(11):1811-1813.
Plagiarism check:Checked twice by iThenticate.
Peer review:Externally peer reviewed.
Open access statement:This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak,and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under identical terms.
Deumens R, Bozkurt A, Meek MF, Marcus MA, Joosten EA, Weis J,Brook GA (2010) Repairing injured peripheral nerves: Bridging the gap. Prog Neurobiol 92:245-276.
Dezawa M, Ishikawa H, Hoshino M, Itokazu Y, Nabeshima Y (2005)Potential of bone marrow stromal cells in applications for neuro-degenerative, neuro-traumatic and muscle degenerative diseases. Curr Neuropharmacol 3:257-266.
Kingham PJ, Kalbermatten DF, Mahay D, Armstrong SJ, Wiberg M,Terenghi G (2007) Adipose-derived stem cells differentiate into a Schwann cell phenotype and promote neurite outgrowth in vitro.Exp Neurol 207:267-274.
Pfister BJ, Gordon T, Loverde JR, Kochar AS, Mackinnon SE, Cullen DK (2011) Biomedical engineering strategies for peripheral nerve repair: surgical applications, state of the art, and future challenges.Crit Rev Biomed Eng 39:81-124.
Radtke C, Wewetzer K, Reimers K, Vogt PM (2011) Transplantation of olfactory ensheathing cells as adjunct cell therapy for peripheral nerve injury. Cell Transplant 20:145-152.
Tamaki T, Uchiyama Y, Okada Y, Ishikawa T, Sato M, Akatsuka A,Asahara T (2005) Functional recovery of damaged skeletal muscle through synchronized vasculogenesis, myogenesis, and neurogenesis by muscle-derived stem cells. Circulation 112:2857-2866.
Tamaki T, Okada Y, Uchiyama Y, Tono K, Masuda M, Wada M,Hoshi A, Akatsuka A (2007a) Synchronized reconstitution of muscle fibers, peripheral nerves and blood vessels by murine skeletal muscle-derived CD34(-)/45 (-) cells. Histochem Cell Biol 128:349-360.
Tamaki T, Okada Y, Uchiyama Y, Tono K, Masuda M, Nitta M,Hoshi A, Akatsuka A (2008) Skeletal muscle-derived CD34+/45-and CD34-/45-stem cells are situated hierarchically upstream of Pax7+ cells. Stem Cells Dev 17:653-667.
Tamaki T, Uchiyama Y, Hirata M, Hashimoto H, Nakajima N, Saito K, Terachi T, Mochida J (2015) Therapeutic isolation and expansion of human skeletal muscle-derived stem cells for the use of muscle-nerve-blood vessel reconstitution. Front Physiol 6:165.
Tamaki T, Hirata M, Nakajima N, Saito K, Hashimoto H, Soeda S,Uchiyama Y, Watanabe M (2016) A long-gap peripheral nerve injury therapy using human skeletal muscle-derived stem cells (Sk-SCs): an achievement of significant morphological, numerical and functional recovery. PLoS One 11:e0166639.
Tamaki T, Okada Y, Uchiyama Y, Tono K, Masuda M, Wada M,Hoshi A, Ishikawa T, Akatsuka A (2007b) Clonal multipotency of skeletal muscle-derived stem cells between mesodermal and ectodermal lineage. Stem Cells 25:2283-2290.
Tamaki T, Hirata M, Soeda S, Nakajima N, Saito K, Nakazato K,Okada Y, Hashimoto H, Uchiyama Y, Mochida J (2014) Preferential and comprehensive reconstitution of severely damaged sciatic nerve using murine skeletal muscle-derived multipotent stem cells. PLoS One 9:e91257.
- 中国神经再生研究(英文版)的其它文章
- The role of general anesthetics and the mechanisms of hippocampal and extra-hippocampal dysfunctions in the genesis of postoperative cognitive dysfunction
- Saponins from Panax japonicus attenuate age-related neuroinflammation via regulation of the mitogenactivated protein kinase and nuclear factor kappa B signaling pathways
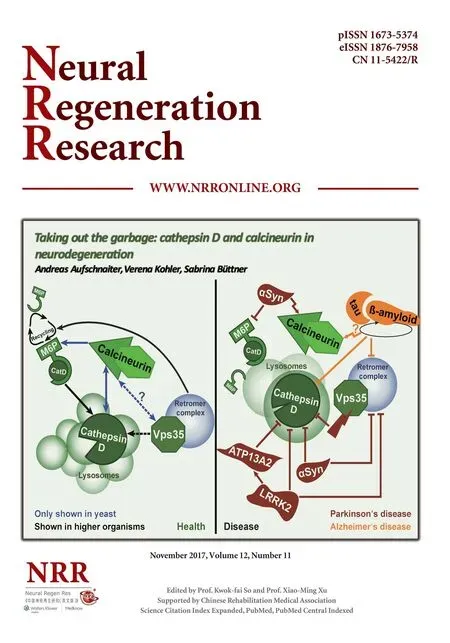
- Taking out the garbage: cathepsin D and calcineurin in neurodegeneration
- MicroRNAs as diagnostic markers and therapeutic targets for traumatic brain injury
- Interferon regulatory factor 2 binding protein 2: a new player of the innate immune response for stroke recovery
- Endogenous retinal neural stem cell reprogramming for neuronal regeneration