Research on human glioma stem cells in China
Yao-dong Zhao, Quan-bin Zhang, Hua Chen, Xi-feng Fei, Yun-tian Shen Xiao-yan Ji Jia-wei Ma Ai-dong Wang Jun DongQing Lan Qiang Huang
1 Department of Neurosurgery and Brain Tumor Research Laboratory, Second Affiliated Hospital of Soochow University, Suzhou, Jiangsu Province,China
2 Shanghai General Hospital, Shanghai, China
3 Shanghai 10th People’s Hospital, Shanghai, China
4 Nanjing First Hospital, Nanjing Medical University, Nanjing, Jiangsu Province, China
5 Suzhou Kowloon Hospital, School of Medicine, Shanghai Jiao Tong University, Shanghai, China
How to cite this article:Zhao YD, Zhang QB, Chen H, Fei XF, Shen YT, Ji XY, Ma JW, Wang AD, Dong J, Lan Q, Huang Q (2017) Research on human glioma stem cells in China. Neural Regen Res 12(11):1918-1926.
Funding: This study was supported by the National Natural Science Foundation of China, No. 81172400, 81101909, 81272793, 81302180,81302196, 81472739.
Introduction
Research on human glioma stem cells (GSCs), like other human cancer stem cells (CSCs), occupies a central role in the development, diagnosis, and treatment of cancers. Currently,GSCs are considered to be a small percentage of the G0-arrested cells located in the glioma niche. GSCs serve as the seed cells for tumorigenesis and metastasis within the tumor microenvironment (Adorno-Cruz et al., 2015).
The existence of CSCs was proposed by the Cancer Center of Michigan University approximately 150 years ago. More recently, Lapidot et al. (1994) identified acute myeloid leukemia-initiating cellsviatransplantation in severe combined immune deficiency mice. Confirmation of the existence of CSCs was first demonstrated by Reya et al. (2001). The relationship between malignant brain tumors and stem cells was suggested in the 1980s by Rosenblum et al. (1983), but 20 years later, Hemmati et al. (2003) identified neural stem-like cells in human glioma cell linesin vitro. Singh et al. (2003)isolated GSCs from pediatric medulloblastoma and astrocytoma. The following year, they reported that the injection of as few as a hundred CD133+cells was enough to produce a tumor, whereas the injection of a hundred thousand CD133–cells resulted in engraftment but no tumor formation (Singh et al., 2004b). Subsequently, Singh et al. (2004a) concluded that CD133+cells that also express the neural stem cell (NSC)marker, nestin, but not differentiated neural lineage markers, represent only a minority fraction of the entire brain tumor cell population that exclusively generate clonal tumor spheres in suspension culture and exhibit an increased self-renewal capacity. Subsequently, the study of GSCs has become the focus of research, mainly looking at cell culture techniques, molecular regulation, signaling pathways, cancer treatment, stem cell microenvironment and the cellular origin and function of GSCs.
Literature Analysis
To date (as of DEC, 2016), Chinese scholars have published approximately 28% (256/908) of the research papers worldwide (Figure 1). In this review, we have collected and analyzed articles from various Chinese universities and Chinese research institutions published in journals included in the Science Citation Index (SCI) system. In addition, we pay special attention to the progress of Chinese research on GSCs,while reviewing the overall global status of GSC research.
Research on human GSCs in China began when CD133+cells and side population cells excluding Hoechst 33342 from the human glioma cell line SHG-44 were first cloned in 2004 and 2005 (Huang, 2004; Wang et al., 2005). In 2006,we reported differences between the differentiation profiles of GSCs and NSCs (Zhang et al., 2006) in which the results of the Chinese research community was not in complete agreement with those of Singh et al. (2004a). Our results showed that these GSCs became CD133–after being induced to differentiate by sodium valproate. However, some of these cells may dedifferentiate into floating tumor spheres with a CD133+phenotype, differing from NSCs, which can be terminally differentiated. Research on human GSCs by other Chinese groups began in 2008 at Southwest Hospital of the Third Military Medical University of PLA, where Yu et al.(2008) harvested GSCs from the U87 glioma cell line. The top 14 Chinese universities publishing research on GSCs are shown in Figure 2.
GSC Culture and Molecular Characteristics of GSCs
The general method for culturing GSCs involves cultivating glioma cells or tissues after enzymatic dissociation with basic fibroblast growth factor, leukemia inhibitory factor, and epidermal growth factor in a serum-free medium (Zhou et al., 2012). The floating tumor spheres are then collected and examined for stemness. Finally, purified GSCs are harvested using immunomagnetic beads or a flow cytometer for CD133+cells. Several other revised methods have been applied including the isolation of GSCs from loose, irregular clone spheres (Cao et al., 2013). Alternatively, GSCs can be harvestedviathe passage and purification of CD133+cells directly from tumor spheres, without using immunomagnetic beads or a flow cytometer (Qiu et al., 2012b). Various other methods have been used to culture GSCs (Pollard et al., 2009; Kievit et al., 2014).
Several questions remain after harvesting GSCs: How do we identify and differentiate these cells from others? Are there some specific markers for GSCs? There are still no true specific markers for them, although CD133 is the marker that is used by most scholars. However, CD133 is also regarded as a marker protein for NSCs (Uchida et al., 2000)and CSCs of other types of cancers, and the existence of CD133–GSCs has also been demonstrated. There are some sub-markers that have been used for the identification of GSCs, such as CD15, neuronal cell adhesion molecule L1(L1CAM), CD90, B7-homologue 4 and 1 (B7-H4/1), CXC chemokine receptor 4 (CXCR4), and A2B5, stage-specific embryonic antigen 1. Of these, the CD15 is a type of adhesion molecule, and it was reported that the tumorigenicity of CD15+medulloblastoma cells was even higher than that of CD133+cells. (Read et al., 2009; Ward et al., 2009). L1CAM is also adhesion molecule, and it is required for maintaining the growth and survival of CD133+glioma cells bothin vitroandin vivo(Bao et al., 2008). B7-H4 is a member of B7 family that negatively regulates T cell-mediated immunity. However, studies showed that B7-H4 was preferentially expressed in GSCs (Yao et al., 2008). CXCR4 is a cell surface molecule expressed in a certain subset of glioma cells with enhanced tumorigenicity. Zheng et al. considered that CXCR4+subsets of glioma cells met the standard of “cancer stem cell” (Zheng et al., 2011). A2B5 is predominantly expressed in embryonic and neonatal neural tissue, and it is also considered as a marker for immature glial-committed precursors. However,some studies claimed that A2B5 was a possible marker of GSCs by comparing the different tumorigenicity of CD133+/–glioma cells and A2B5+/–cells (Ogden et al., 2008).
The differentiation trend appears to be more important than the so-called specific protein markers in the identification of GSCs. The definition of GSC follows the theory of NSCs, namely that GSCs are identified based on the presence of cells expressing markers for neurons, astrocytes, and microglia, in differentiated cell populations. This outlines the importance of surface markers for the identification of GSCs.
Side population cells have also been used by some researchers to identify CSCs on the basis of high expression of the ATP binding transporter G superfamily-2 protein on the surface of stem cells. ATP binding transporter G superfamily-2 can pump the Hoechst 33342 fluorochrome out of the cytoplasm, which facilitates the screening of side population cells with flow cytometry. The similar characteristics between side population cells and CSCs suggest they could be identical. However, the proportion of side population cells among SHG44 human glioma cells is approximately 29.1%,while that of CD133+cells is only about 2.3% (Wang et al.,2005). This implies an evident significant difference between them. Each of the methods for CD133 immunophenotyping,side population flow assays and neurosphere counting have their own uses and limitations.
Many of the substances that regulate GSCs are positive regulators, including pyruvate kinase isozymes M2 (which phosphorylates histone H3), the CDC20-anaphase promoting complex/sex determining region-box 2 signaling axis,cyclin-dependent kinase 7-MYCN, Beta1, 4-galactosyltransferas, vascular endothelial growth factor-vascular endothelial growth factor receptor, nuclear related factor 2 (Nrf2) (Zhu et al., 2013, 2014b), H3K4me3 and H3K27me3, topoisomerase II alpha, Bcl-2, S100A9 (Chen et al., 2013), reactive oxygen species (Yuan et al., 2015) and Zinc finger protein 217. Other signaling pathways show negative correlations with the activities of CSCs, such as Fas/FasL-L. GSCs can be induced to proliferate with 2% sevofluranein vitrowith the up-regulation of CD133, vascular endothelial growth factor,hypoxia-inducible factor-1, and hypoxia-inducible factor-2(Shi et al., 2015b).
There are gene mutations related to CSCs. For example, in GSC-SU2 (Zhao et al., 2009), there are many mutations of amino acid residues (from the 8thto 14thamino acid (AA),238thAA, and 398thAA) in the peptide chain of phosphate and tensin homologue (PTEN) deleted on chromosome ten. These mutated regions are involved in membrane interactions, particularly those involving the phospholipid phosphatidylinositol bisphosphate, and in maintaining the protein stability of PTEN. Therefore, these mutations not only lead to the rapid degradation of PTEN, but also inhibit the cellular function of PTEN to down-regulate PI3K signaling. Isocitrate dehydrogenase 1 mutation and dependent promoter methylation of O6-methylguanine-DNA methyltransferase (MGMT) were reported as predictive biomarkers for glioma patients (Wick et al., 2013).
In fact, the formation of GSCs results from not only one or two specific molecular mechanisms, but many other signaling pathways as well. CSCs are thought to be derived from the adult stem cells (ASCs) of the corresponding tissues or organs in which many of the pathways share a common molecular basis for both these cell types. Only molecules that are upregulated or downregulated may be different in ASCs,for tissue repair and regeneration, from CSC tumorigenesis.
Moreover, the Notch signaling pathway contributes to the maintenance of GSCs and NSCs and promotes the re-newal of GSCs (Hu et al., 2014). It has been reported that neurotensin signaling may maintain the stemness of GSCs through the activation of the interleukin-8/CXCR 1/signal transducer and activator of transcription 3 (IL-8/CXCR1/STAT3) signaling pathway (Zhou et al., 2014). Aurora A kinase could control GSC self-renewal through beta chain protein/Wnt signaling (Zhou et al., 2014). Activation of the Akt/phosphatidylinositol-3 kinases (Akt/PI3K) pathway through interaction with CD133-p85 promotes GSC oncogenicity (Wei et al., 2013). The stemness and radiation resistance of GSCs is maintained through regulation of the mi-croRNA-153/Nrf-2/ GPx1 pathway by reactive oxygen species (Yang et al., 2015). GSCs enhance the migration and proliferation of endothelial cells through the Hedge-hog pathway (Zhou et al., 2014). Gong et al. (2015) reported that FoxM1 promotes the self-renewal and tumorigenicity of GSCs by driving a feed-forward STAT3-activation signaling loop.
These findings are limited to the origin of CSCs as ASCs,a view that is still controversial. The epithelial-to-mesenchymal transition of CSCs and normal stem cells from their corresponding normal tissue involve similar stem cell programs.However, they differ significantly in terms of their paralogous epithelial-to-mesenchymal transition-inducing transcription factors Slug and Snail programs (Ye et al., 2015).
It has become increasingly clear that miRNAs and GSCs are connected. Studies have shown that miRNAs, such as miR-125b (Wan et al., 2012, 2014), miR-123b, miR 20a (Wang et al., 2015d), and miR-210 (Yang et al., 2014a), play a positive regulatory role in GSC invasion and proliferation. Other miRNAs, such as miR 181b, miR-134a, miR-21 (Shang et al., 2015), miR-124, miR-186 (Zheng et al., 2015), and miR-145 (Shi et al., 2014), negatively regulate GSC proliferation.In addition, miR-330 negatively regulates the expression of SH3GL2 in GSCs, which promotes the oncogenic progression of GSCs through activating the ERK and PI3K/AKT signaling pathways (Yao et al., 2014b), and miR-152 plays a tumor suppressor role in GSCs (Yao et al., 2015a).
Cellular Origin and Function of CSCs
There is still no consensus on the cellular origin of CSCs.There are four main theories. (1) Cloning evolution: tumors represent a molecular disease in which gene mutations within originating cells will be passed onto future daughter cells,where further gene mutations may occur. Thus, the accumulation of many genes in descendant cells leads to carcinogenesis and malignant development. (2) The CSC theory, which was first put forward by Hamburger and Salmon (1977) and later improved by Bonnet and Dick (1997) indicated that cancer originates from a single ASC. Cancer is also induced and driven by carcinogenic agents that activate the necessary pathways and related genes for ASC proliferation and differentiation. Therefore, CSCs are also referred to ASC-like cells(e.g., GSCs are also known as NSC-like cells). (3) The balance theory: there is considerable plasticity between non-CSCs(NCSCs) and CSCs. NCSCs can reacquire the phenotype of CSCs under certain environmental conditions, and that bidirectional conversion occurs between them (Marjanovic et al., 2013). In 2006, we found that differentiated glioma cells might dedifferentiate into GSCs when we compared the differentiation profiles between NSCs and GSCs. Zheng et al. (2007) found that most C6 cells were cancer stem cells.As CD133–C6 cells also possessed clonogenic, self-renewal,and tumorigenic capacities, this may indicate the reversion of CD133–cells to CD133+cells. (4) The precancerous stem cell (pCSCs) theory: Gao (2008) believed that pCSCs are at an early stage of development of CSCs, similar to the traditional theory about tumor formation;i.e., a similar histological development process from cell proliferation, metaplasia,and precancerous lesions to cancerous tissue. This process is regulated by Piwi like RNA-mediated gene silencing 2, and,while pCSCs can continue their malignant evolution, they can also revert back to a benign state different from that of CSCs.
The function of CSCs has been elucidated. The known characteristics include (1) self-renewal, which refers to the mitosis of CSCs and includes two types: symmetric mitosis and asymmetric mitosis. The former produces two CSCs, while the latter produces one CSC and one NCSC,followed by downstream differentiation. This is similar for ASCs, which produce a new stem cell to replace the old one. Further investigation is required to determine whether the self-renewal of GSCs and ASCs is truly identical. The self-renewal of ASCs only occurs in the stem cell niche,while the self-renewal of CSCs may occur outside of their niche or be completed by differentiated NCSCs after homing(Clarke and Fuller, 2006). (2) High tumorigenicity. It has also been reported that only one hundred CD133+GSCs produce tumors in non-obese diabetic/severe combined immune deficiency micein vivo, whereas even 100,000 CD133–NCSCs do not lead to tumor formation in the same period of time (Singh et al., 2004b). (3) Greater invasiveness. Qiu et al. (2012a) reported that GSCs are more invasive than their differentiated progeny cellsin vitro. Invasive cells exhibit higher tumorigenicityin vivo, and Akt activity is significantly increased in invasive cells compared with normal cells in the corresponding tumor mass. The molecules involved in invasion include Toll-like receptors and matrix metalloproteinases-9 (Wang et al., 2015b), TGF-β1, ADAM17, and IL-6. (4) Radiation resistance. Bao et al. (2006) believe that the increase of the proportion of CD133+cells in the glioma cell population after radiation therapy is due to the radiation resistance of GSCs, which are preferentially preserved.The molecules associated with radioresistance include Wnt/β-catenin, Notch, JAK/STAT and PI3k-mTOR, checkpoint kinase 1, CD133 and MGMT. (5) Chemotherapy resistance.Hu et al. (2012) reported that the chemoresistance of human GSCs is correlated with a low level of Tap73. Furthermore,down-regulation of autophagy in GSCs contributes to the strong ability of GSCs to resist temozolomide. High expression of ATP binding transporter G superfamily-2 in SU2-GSCs results in resistance to ACNU (Huang et al., 2008;Jin et al., 2009). It has been reported that GSCs adapt to reduce their glucose dependence and this is associated with radio-chemoresistance (Ye et al., 2013). High expression of MGMT has been reported to contribute to temozolomide resistance in GSCs (Qiu et al., 2014). However, interferon-α/β may enhance the sensitization of MGMT-positive GSCs to temozolomide by suppressing NF-κB activity (Shen et al.,2015a). (6) Angiogenesis. Tumor-derived endothelial cells originating from GSCs were detected in tumor tissues from a p53 (+/–) homozygous mouse model bearing GBM. Both Li et al. (2013) and our group (Zhao et al., 2010a) have reported the trans-differentiation of GSCs into vascular endothelial-like cellsin vitroand we demonstrated a novel mechanism for angiogenesis that GSCs contribute to the neovascularization of gliomaviatransdifferentiationin vivo(Dong et al.,2011; Sun et al., 2015). However, Cheng et al. (2013) reported that GSCs contribute to vascular pericytes. In addition, it has been demonstrated that GSCs have the potential to show vascular mimicry and trans-differentiate into vascular endothelial cells in different conditions (Mao et al., 2013a, b; Yao et al., 2013).al., 2003). The ASC niche serves two functions: to maintain ASC self-renewal, and to supply our bodies with different types of cellsviamulti-directional differentiation.
In the tumor microenvironment, there are tumor stroma in addition to the CSC niche. The stroma of a glioma contains myeloid-derived suppressor cells, including tumor-associated macrophages, dendritic cells, and secreted cytokines. GSCs can recruit macrophages and microglia in brain glioma cells to promote tumor cell growth (Shi et al., 2015c).We also observed malignant transformation of macrophages and microglia induced by GSCs (Chen et al., 2015; Dai et al.,2015; Wang et al., 2015a).
Microenvironment of GSCs
Reciprocal causation occurs when GSCs rebuild the tumor microenvironment, and the tumor microenvironment influences the phenotype of GSCs. Zhang et al. (2013b) cultivated U251 glioma cells under various culture conditions and harvested the GSC-like cells of different phenotypes (U251-Adh, U251-SC-Sph and U251-SC-Adh). These cells also showed distinct growth patterns and self-renewal capacities.The chemokines secreted by GSCs promote the migration of NSCs to GSCs. NSC co-culture with GSCs may also induce the differentiation of GSCsin vitro, and reduce their stemness. NSCs injected into the cerebral hemisphere,in vivo,migrate towards the GSCs in the tumor, reducing their malignancy (Zhang et al., 2014c). We reported that GSCs play an important role in the vascular remodeling of transplanted tumors (Zhao et al., 2010b). However, all the above studies were completedin vitroor in the so-called tumor microenvironmentin vivo.
The microenvironment of GSCs is where the GSCs are anchored, also known as the stem cell niche. Different stem cell niches may exhibit different structures, however, all stem cells including GSCs generally present unique niches(Fuchs et al., 2004). A niche exists along micro-blood vessels in cancerous tissue, acting as an umbrella to maintain stem cell self-renewal and prevent differentiation. The structure of niches includes niche cells, soluble factors from niche cells,and extracellular matrix (Lin, 2002).
A niche is composed of cells such as vascular endothelial cells, peripheral blood cells, and astrocytes. The niche cells produce cadherin and integrin molecules that mediate the adherence of ASCs and some other cell types in and around the niche (Lin, 1998; Song and Xie, 2002; Song et al., 2002;Zhang et al., 2003; Arai et al., 2005). Only the ASCs anchoring in the niche maintain quiescent conditions, whereas cells outside the niche enter the differentiation process (Zhang et
Treatment Strategies Targeting GSCs
Approximately three years ago, Cho et al. (2013) summarized and introduced five methods of targeting CSCs. These included new chemotherapy drugs, radiation-sensitizing agents, cell immunotherapy, induced differentiation, and gene therapy. The advances in this research have led to the following therapies.
Molecular targeted therapy
Treatment aimed at GSCs should be focused on specific molecular targets. Promising results have been demonstrated for some molecules,e.g., Knock-down of target genes of L1CAM, miR-101 (Yao et al., 2015b), and miR-152 (Ma et al., 2014); upregulation of Cx43; inhibition of Alox-5 with dl-nordihydroguaiaretic acid (Nordy); expression of an exogenous Endo-Angio fusion gene [VAE] (Zhu et al., 2011;Zhang et al., 2014a); use of the nuclear factor-κB inhibitor SN50 (Zhang et al., 2014b); endothelial-monocyte activating polypeptide-II (Liu et al., 2014); down-regulation of TGF-β2 with temozolomide; an attenuating the expression of ID1viaTGM2 inhibition (Fu et al., 2013). However, the problem of whether the specific target molecules of CSCs/GSCs have been blocked remains unclear. Targeted molecular therapy will continue to be inconclusive until a truly specific stem cell marker protein is found.
Smart nanomedicines
Smart nanomedicine refers to nanomedicines showing tumor-targeting properties and controlled release for use in tracing and combination therapyin vivo. Such nanoparticles can respond sensitively to stimuli including temperature,pH, the redox environment (Glutathione), ionic strength,and electromagnetic fields. Moreover, the size, shape, and structure of nanoparticles can be changed according to the treatment, delivery and release of the drug to the target GSCs/CSCs. However, it is not easy to fully meet the above requirements. Current research generally only meets a subset of these requirements. For example, nanoparticles conjugated with a CD133 monoclonal antibody can be used to treat CD133+GSCs and transplanted tumors when combined with infrared laser irradiation.
The metallofullerenol nanomaterial Gd@C82(OH)22 possesses intrinsic inhibitory activity against triple-negative breast cancer cells, while remaining relatively non-toxic to normal mammary epithelial cells (Liu et al., 2015). The de-livery of epirubicin by nanodiamonds is a highly effective nanomedicine-based approach for overcoming chemoresistance in hepatic CSCs (Wang et al., 2014). A transferrin-modified graphene oxide used as a glioma-targeted drug exhibited significantly improved therapeutic efficacy for glioma bothin vitroandin vivo(Liu et al., 2013). Silica nanorattle-doxorubicin-anchored mesenchymal stem cells used for tumor-tropic therapy show the potential to be developed as a robust and generalizable method for targeted tumor therapy,with a high efficiency and low systematic toxicity.
Chemotherapy
Some of the effective drugs targeting CSCs/GSCs include curcumin (Zhuang et al., 2012; Shi et al., 2015a), rapamycin, temozolomide (Zhitao et al., 2015), the topoisomerase I inhibitors shikonin and topotecan (Zhang et al., 2013a),TRAIL and paclitaxel, Nordy (Yang et al., 2014b), wheat germ agglutinin and tamoxifen (Li et al., 2014), TRF2 (Bai et al., 2014), metformin and temozolomide (Yu et al., 2015),Cisplatin, the glycolytic inhibitor 3-BrOP and carmustine(Yuan et al., 2013), Korean herbal recipe MSC500 (Yao et al., 2014a), and suberoylanilide hydroxamic acid (Chiao et al., 2013). There are also some medicines not designed to attack cancer that are effective in the treatment of CSCs/GSCs,such as metformin and gemcitabine (Chai et al., 2015) and nicardipine (Jin et al., 2009; Lou and Zhao, 2015).
Although many drugs have been designed to target GSCs,none have shown an effect on GSCs at G0phase within the niche. In fact, the niche does not existex vivo, and even in researchin vivo, most authors were not able to detect changes in GSCs in the niche. Reactions of the micro-vascular density are only changes in the vascular endothelium,and not in the niche and, particularly not in the GSCs.Therefore, the improved curative effects of most of the drugs mentioned above are not strictly through the targeting of CSCs/GSCs.
Radiotherapy
Sun et al. (2012, 2013) first reported that boron neutron capture therapy induces cell cycle arrest and cell apoptosis of glioma stem/progenitor cellsin vitro. Inhibition of the PI3K/mTOR pathway with NVP-BEZ235 may enhance the radiosensitivity of human glioma stem cellsin vitro(Wang et al., 2013), and it has been reported that induction of autophagy promotes the radiosensitivity of glioma-initiating cells.These authors also found that knockdown of the DNA-dependent protein kinase catalytic subunit could radiosensitize glioma-initiating cells by inducing autophagy. Inhibition of Notch signaling can enhance the radiosensitivity of malignant stromal cells induced by glioma stem/progenitor cells or GSCs themselves (Shen et al., 2015b).

Figure 1 Number of articles about human glioma stem cells published in China and worldwide is rising year by year.

Figure 2 Ranking of the top 14 universities in China that have published ≥ 5 original articles on human glioma stem cells.I: Soochow University; II: The Third Military Medical University; III:China Medical University; IV: The Fourth Military Medical University;V: Fudan University; VI: Jiangsu University; VII: Sun Yat-sen University; VIII: Southern Medical University; IX: Huazhong University of Science and Technology; X: Harbin Medical University; XI: Nanjing Medical University; XII: Jilin University; XIII: Shanghai Jiao Tong University; XIV: Anhui Medical University.

Figure 3 Schematic diagram showing the transformation between NGCs, NSCs and TSCs in the brains of glioma patients.The solid arrow indicates that the transformation of NSCs to NGCs and the transformation of NGCs to TSCs have been well established. The dotted arrow indicates that the transformation of TSCs to NGCs and the transformation of NSCs to TSCs have received support from some research results, but currently this support is not sufficient. The hollow arrow indicates that a few reports have provided support for the transformation of NGCs to NSCs and the transformation of TSCs to NSCs,but research in this field is meagre. NGCs: Normal glial cells; NSCs:neural stem cells; TSCs: tumor stem cells.
Summary and Prospects
Research on GSCs began more than 10 years ago and 908 articles on this topic have already been published. However,fully understanding the theory and mechanisms of GSCs remains a great challenge in considering the occurrence, development, prevention and treatment of glioma. Only when the GSCs are fully understood can glioma be overcome.Therefore, the focus of the study of glioma should still be placed on GSCs.
The number of relevant papers published in China addressing GSCs continues to show an increasing trend year by year, as in other countries around the world (Figures 1and2). However, what is more urgently needed is innovative research. The question is where to start? We believe that more in-depth research associated with induced pluripotent stem cells may be one of many directions to consider.
In 2010, we published in China’s cancer forum (Huang and Du, 2010) the hypothesis of transformation among normal glial cells (NGCs), neural stem cells (NSCs) and tumor stem cells (TSCs) in the tumor microenvironment where the concept of induced pluripotent stem cells was implied(Figure 3). First, can NGCs be translated into induced pluripotent stem-like NSCs (one of the two hollow arrows in the figure)? The transfection of neuronal differentiation-related gene Ngn2 or Dlx1 into astrocytes resulted in a subsequent transformation of astrocytes into functional neurons(Heinrich et al., 2010). Also, when reactive glial cells and fibroblasts were transfected with NeuroD1, it resultedin the reprogramming of both types of cells into functional neurons (Pang et al., 2011; Guo et al., 2014).
Second, can TSCs be transformed into NSCs? Introduction of Ngn2 in GSCs induces massive cell death, proliferation arrest and a drastic reduction of neurosphere formation. Moreover, the few surviving cells adopt a typical neuronal morphology, and some generated action potentials(Guichet et al., 2013).
The third question (dotted arrow in the figure) is whether TSCs can be translated into NGCs? Dimethylformamide and hexamethylene bisacetamide and all-trans retinoic acid,have been used to induce the differentiation of glioma cells or GSCs. Zhu et al. (2014a) induced the differentiation of GSCs by knocking down the expression of Nrf2. All of these results showed that GSCs differentiated in a benign direction after induction; however, none of these cells reached a terminal differentiation stage. The fourth question is whether NSCs can be transformed into TSCs, as mentioned in the“Cellular origin of GSCs/CSCs” section. It can be concluded that tumorigenesis originates from a single ASC, triggered and driven by carcinogenic factors, which can be considered to be ASCs with abnormal phenotypes. Therefore, scholars generally refer to CSCs as ASC-like cells (e.g., GSCs are known as NSC-like cells).
The two solid arrows inFigure 3represent traditional theories. However, tumor stromal cells, which are normal cells, may be transformed into cancer cells under malignant pressure from the tumor microenvironment. In gliomas, we have proven that macrophages, oligodendrocytes,and fibroblasts in the microenvironment of SU3-GSCs can transform into cancer cellsin vivo(Chen et al., 2015; Dai et al., 2015; Wang et al., 2015a). These progressions indicate that the three types of cells can be transformed into each other under specific microenvironmental conditions, as indicated by our hypothesis. However, the so-called specific microenvironmental conditions currently refer to the corresponding experimental conditions, and the situation in spontaneous human cancer remains unknown, which is a task to be addressed in the future.
Animal models are often used to understand certain processes and mechanisms that occur within the human body.According to our studies (Shen et al., 2015c; Wang et al.,2015c), nude mice transfected with GFP are generally an ideal model for research on the relationship between the tumor microenvironment and tumorigenesis/tumor development, because cells from the host microenvironment all show high expression of GFP, a “natural” tracer molecule.
In short, the future research on human GSCs should be expanded to examine the mutual influence between GSCs and tumor microenvironment, and to explore the key regulatory factors for the potential forward and reverse transformations among NSCs, NGCs and TSCs in glioma tissue.
Summary of work done by the contributors:Our team has been engaged in the research of glioma for a long time, and it has been more than 30 years since the establishment of the first human glioma cell line SHG-44 in China by us. In recent years, along with the international research hotspots, we focus on the research of glioma stem cells (GSC). And we are the first team in China to publish GSC research articles in journals e.g.Cell Res and BMC cancer, where we first present glioma cells could reverse differentiate into GSC, and GSC from recurrent glioma tumor tissues are more invasive and aggressive than that of primary glioma. These articles now have been cited for more than 150 times.
Author contributions:YDZ, QBZ, HC and XFF drafted the paper and took part in the literature reviews. YTS, XYJ, JWM, and ADW were in charge of literature reviews. JD, QL, and QH were responsible for the design of this paper. All authors approved the final version of this paper.
Conflicts of interest:None declared.
Plagiarism check:Checked twice by iThenticate.
Peer review:Externally peer reviewed.
Open access statement:This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under identical terms.
Open peer reviewer:Paul Lu, University of California, USA.
Adorno-Cruz V, Kibria G, Liu X, Doherty M, Junk DJ, Guan D, Hubert C, Venere M, Mulkearns-Hubert E, Sinyuk M, Alvarado A, Caplan AI, Rich J, Gerson SL, Lathia J, Liu H (2015) Cancer stem cells: targeting the roots of cancer, seeds of metastasis, and sources of therapy resistance. Cancer Res 75:924-929.
Arai F, Hirao A, Suda T (2005) Regulation of hematopoiesis and its interaction with stem cell niches. Int J Hematol 82:371-376.
Bai Y, Lathia JD, Zhang P, Flavahan W, Rich JN, Mattson MP (2014)Molecular targeting of TRF2 suppresses the growth and tumorigenesis of glioblastoma stem cells. Glia 62:1687-1698.
Bao S, Wu Q, Li Z, Sathornsumetee S, Wang H, McLendon RE,Hjelmeland AB, Rich JN (2008) Targeting cancer stem cells through L1CAM suppresses glioma growth. Cancer Res 68:6043-6048.
Bao S, Wu Q, McLendon RE, Hao Y, Shi Q, Hjelmeland AB, Dewhirst MW, Bigner DD, Rich JN (2006) Glioma stem cells promote radioresistance by preferential activation of the DNA damage response.Nature 444:756-760.
Bonnet D, Dick JE (1997) Human acute myeloid leukemia is organized as a hierarchy that originates from a primitive hematopoietic cell.Nat Med 3:730-737.
Cao X, Gu Y, Jiang L, Wang Y, Liu F, Xu Y, Deng J, Nan Y, Zhang L, Ye J,Li Q (2013) A new approach to screening cancer stem cells from the U251 human glioma cell line based on cell growth state. Oncol Rep 29:1013-1018.
Chai X, Chu H, Yang X, Meng Y, Shi P, Gou S (2015) Metformin increases sensitivity of pancreatic cancer cells to gemcitabine by reducing CD133+cell populations and suppressing ERK/P70S6K signaling.Sci Rep 5:14404.
Chen S, Zhao H, Deng J, Liao P, Xu Z, Cheng Y (2013) Comparative proteomics of glioma stem cells and differentiated tumor cells identifies S100A9 as a potential therapeutic target. J Cell Biochem 114:2795-2808.
Chen Y, Wang Z, Dai X, Fei X, Shen Y, Zhang M, Wang A, Li X, Wang Z,Huang Q, Dong J (2015) Glioma initiating cells contribute to malignant transformation of host glial cells during tumor tissue remodeling via PDGF signaling. Cancer Lett 365:174-181.
Chiao MT, Cheng WY, Yang YC, Shen CC, Ko JL (2013) Suberoylanilide hydroxamic acid (SAHA) causes tumor growth slowdown and triggers autophagy in glioblastoma stem cells. Autophagy 9:1509-1526.
Cho DY, Lin SZ, Yang WK, Lee HC, Hsu DM, Lin HL, Chen CC, Liu CL, Lee WY, Ho LH (2013) Targeting cancer stem cells for treatment of glioblastoma multiforme. Cell Transplant 22:731-739.
Clarke MF, Fuller M (2006) Stem cells and cancer: two faces of eve. Cell 124:1111-1115.
Dai X, Chen H, Chen Y, Wu J, Wang H, Shi J, Fei X, Wang Z, Wang A,Dong J, Lan Q, Huang Q (2015) Malignant transformation of host stromal fibroblasts derived from the bone marrow traced in a dual-color fluorescence xenogra ft tumor model. Oncol Rep 34:2997-3006.
Dong J, Zhao Y, Huang Q, Fei X, Diao Y, Shen Y, Xiao H, Zhang T, Lan Q, Gu X (2011) Glioma stem/progenitor cells contribute to neovascularization via transdifferentiation. Stem Cell Rev 7:141-152.
Fu J, Yang QY, Sai K, Chen FR, Pang JC, Ng HK, Kwan AL, Chen ZP(2013) TGM2 inhibition attenuates ID1 expression in CD44-high glioma-initiating cells. Neuro Oncol 15:1353-1365.
Fuchs E, Tumbar T, Guasch G (2004) Socializing with the Neighbors.Cell 116:769-778.
Gao JX (2008) Cancer stem cells: the lessons from pre-cancerous stem cells. J Cell Mol Med 12:67-96.
Guichet PO, Bieche I, Teigell M, Serguera C, Rothhut B, Rigau V,Scamps F, Ripoll C, Vacher S, Taviaux S, Chevassus H, Duffau H,Mallet J, Susini A, Joubert D, Bauchet L, Hugnot JP (2013) Cell death and neuronal differentiation of glioblastoma stem-like cells induced by neurogenic transcription factors. Glia 61:225-239.
Guo Z, Zhang L, Wu Z, Chen Y, Wang F, Chen G (2014) In vivo direct reprogramming of reactive glial cells into functional neurons after brain injury and in an Alzheimer’s disease model. Cell Stem Cell 14:188-202.
Hamburger A, Salmon SE (1977) Primary bioassay of human myeloma stem cells. J Clin Invest 60:846-854.
Heinrich C, Blum R, Gascon S, Masserdotti G, Tripathi P, Sanchez R,Tiedt S, Schroeder T, Gotz M, Berninger B (2010) Directing astroglia from the cerebral cortex into subtype specific functional neurons.PLoS Biol 8:e1000373.
Hemmati HD, Nakano I, LazareffJA, Masterman-Smith M, Geschwind DH, Bronner-Fraser M, Kornblum HI (2003) Cancerous stem cells can arise from pediatric brain tumors. Proc Natl Acad Sci U S A 100:15178-15183.
Hu X, Wu N, Xia P, Yu S, Sun F, Chen J (2012) Correlation between low-level expression of the tumor suppressor gene TAp73 and the chemoresistance of human glioma stem cells. Cancer Chemother Pharmacol 69:1205-1212.
Hu YY, Fu LA, Li SZ, Chen Y, Li JC, Han J, Liang L, Li L, Ji CC, Zheng MH, Han H (2014) Hif-1alpha and Hif-2alpha differentially regulate Notch signaling through competitive interaction with the intracellular domain of Notch receptors in glioma stem cells. Cancer Lett 349:67-76.
Huang Q (2004) The research of glioma stem cells and neural stem cells. Shiyong Zhongliu Zazhi 19:267-269.
Huang Q, Zhang QB, Dong J, Wu YY, Shen YT, Zhao YD, Zhu YD, Diao Y, Wang AD, Lan Q (2008) Glioma stem cells are more aggressive in recurrent tumors with malignant progression than in the primary tumor, and both can be maintained long-term in vitro. BMC Cancer 8:304.
Jin Y, Bin ZQ, Qiang H, Liang C, Hua C, Jun D, Dong WA, Qing L(2009) ABCG2 is related with the grade of glioma and resistance to mitoxantone, a chemotherapeutic drug for glioma. J Cancer Res Clin Oncol 135:1369-1376.
Kievit FM, Florczyk SJ, Leung MC, Wang K, Wu JD, Silber JR, Ellenbogen RG, Lee JS, Zhang M (2014) Proliferation and enrichment of CD133(+) glioblastoma cancer stem cells on 3D chitosan-alginate scaffolds. Biomaterials 35:9137-9143.
Lapidot T, Sirard C, Vormoor J, Murdoch B, Hoang T, Caceres-Cortes J, Minden M, Paterson B, Caligiuri MA, Dick JE (1994) A cell initiating human acute myeloid leukaemia after transplantation into SCID mice. Nature 367:645-648.
Li P, Zhou C, Xu L, Xiao H (2013) Hypoxia enhances stemness of cancer stem cells in glioblastoma: an in vitro study. Int J Med Sci 10:399-407.
Li XT, Ju RJ, Li XY, Zeng F, Shi JF, Liu L, Zhang CX, Sun MG, Lou JN, Lu WL (2014) Multifunctional targeting daunorubicin plus quinacrine liposomes, modified by wheat germ agglutinin and tamoxifen, for treating brain glioma and glioma stem cells. Oncotarget 5:6497-6511.
Lin H (1998) The self-renewing mechanism of stem cells in the germline. Curr Opin Cell Biol 10:687-693.
Lin H (2002) The stem-cell niche theory: lessons from flies. Nat Rev Genet 3:931-940.
Liu G, Shen H, Mao J, Zhang L, Jiang Z, Sun T, Lan Q, Zhang Z (2013)Transferrin modified graphene oxide for glioma-targeted drug delivery: in vitro and in vivo evaluations. ACS Appl Mater Interfaces 5:6909-6914.
Liu J, Liu L, Xue Y, Meng F, Li S, Wang P, Liu Y (2014) Anti-neoplastic activity of low-dose endothelial-monocyte activating polypeptide-II results from defective autophagy and G2/M arrest mediated by PI3K/Akt/FoxO1 axis in human glioblastoma stem cells. Biochem Pharmacol 89:477-489.
Liu Y, Chen C, Qian P, Lu X, Sun B, Zhang X, Wang L, Gao X,Li H, Chen Z, Tang J, Zhang W, Dong J, Bai R, Lobie PE, Wu Q, Liu S, Zhang H, Zhao F, Wicha MS, Zhu T, Zhao Y (2015)Gd-metallofullerenol nanomaterial as non-toxic breast cancer stem cell-specific inhibitor. Nat Commun 6:5988.
Lou M, Zhao Y (2015) Satisfactory therapy results of combining nimustine with nicardipine against glioma at advanced stage. J Cancer Res Ther 11:1030.
Ma J, Yao Y, Wang P, Liu Y, Zhao L, Li Z, Li Z, Xue Y (2014) MiR-152 functions as a tumor suppressor in glioblastoma stem cells by targeting Kruppel-like factor 4. Cancer Lett 355:85-95.
Mao XG, Song SJ, Xue XY, Yan M, Wang L, Lin W, Guo G, Zhang X(2013a) LGR5 is a proneural factor and is regulated by OLIG2 in glioma stem-like cells. Cell Mol Neurobiol 33:851-865.
Mao XG, Xue XY, Wang L, Zhang X, Yan M, Tu YY, Lin W, Jiang XF,Ren HG, Zhang W, Song SJ (2013b) CDH5 is specifically activated in glioblastoma stemlike cells and contributes to vasculogenic mimicry induced by hypoxia. Neuro Oncol 15:865-879.
Marjanovic ND, Weinberg RA, Chaffer CL (2013) Cell plasticity and heterogeneity in cancer. Clin Chem 59:168-179.
Ogden AT, Waziri AE, Lochhead RA, Fusco D, Lopez K, Ellis JA, Kang J,Assanah M, McKhann GM, Sisti MB, McCormick PC, Canoll P, Bruce JN (2008) Identification of A2B5+CD133-tumor-initiating cells in adult human gliomas. Neurosurgery 62:505-514; discussion 514-515.
Pang ZP, Yang N, Vierbuchen T, Ostermeier A, Fuentes DR, Yang TQ,Citri A, Sebastiano V, Marro S, Sudhof TC, Wernig M (2011) Induction of human neuronal cells by defined transcription factors. Nature 476:220-223.
Pollard SM, Yoshikawa K, Clarke ID, Danovi D, Stricker S, Russell R,Bayani J, Head R, Lee M, Bernstein M, Squire JA, Smith A, Dirks P (2009) Glioma stem cell lines expanded in adherent culture have tumor-specific phenotypes and are suitable for chemical and genetic screens. Cell Stem Cell 4:568-580.
Qiu B, Zhang D, Tao J, Tie X, Wu A, Wang Y (2012a) Human brain glioma stem cells are more invasive than their differentiated progeny cells in vitro. JClin Neurosci 19:130-134.
Qiu B, Zhang D, Tao J, Wu A, Wang Y (2012b) A simplified and modified procedure to culture brain glioma stem cells from clinical specimens. Oncol Lett 3:50-54.
Qiu ZK, Shen D, Chen YS, Yang QY, Guo CC, Feng BH, Chen ZP (2014)Enhanced MGMT expression contributes to temozolomide resistance in glioma stem-like cells. Chin J Cancer 33:115-122.
Read TA, Fogarty MP, Markant SL, McLendon RE, Wei Z, Ellison DW,Febbo PG, Wechsler-Reya RJ (2009) Identification of CD15 as a marker for tumor-propagating cells in a mouse model of medulloblastoma. Cancer Cell 15:135-147.
Reya T, Morrison SJ, Clarke MF, Weissman IL (2001) Stem cells, cancer,and cancer stem cells. Nature 414:105-111.
Rosenblum ML, Gerosa MA, Wilson CB, Barger GR, Pertuiset BF, de Tribolet N, Dougherty DV (1983) Stem cell studies of human malignant brain tumors. Part 1: Development of the stem cell assay and its potential. J Neurosurg 58:170-176.
Shang C, Guo Y, Hong Y, Liu YH, Xue YX (2015) MiR-21 up-regulation mediates glioblastoma cancer stem cells apoptosis and proliferation by targeting FASLG. Mol Biol Rep 42:721-727.
Shen D, Guo CC, Wang J, Qiu ZK, Sai K, Yang QY, Chen YS, Chen FR,Wang J, Panasci L, Chen ZP (2015a) Interferon-α/β enhances temozolomide activity against MGMT-positive glioma stem-like cells.Oncol Rep 34:2715-2721.
Shen Y, Chen H, Zhang J, Chen Y, Wang M, Ma J, Hong L, Liu N, Fan Q, Lu X, Tian Y, Wang A, Dong J, Lan Q, Huang Q (2015b) Increased Notch signaling enhances radioresistance of malignant stromal cells induced by glioma stem/progenitor cells. PLoS One 10:e0142594.
Shen Y, Zhang Q, Zhang J, Lu Z, Wang A, Fei X, Dai X, Wu J, Wang Z,Zhao Y, Tian YE, Dong J, Lan Q, Huang Q (2015c) Advantages of a dual-color fluorescence-tracing glioma orthotopic implantation model: Detecting tumor location, angiogenesis, cellular fusion and the tumor microenvironment. Exp Ther Med 10:2047-2054.
Shi L, Fei X, Wang Z (2015a) Demethoxycurcumin was prior to temozolomide on inhibiting proliferation and induced apoptosis of glioblastoma stem cells. Tumour Biol 36:7107-7119.
Shi L, Wang Z, Sun G, Wan Y, Guo J, Fu X (2014) miR-145 inhibits migration and invasion of glioma stem cells by targeting ABCG2.Neuromolecular Med 16:517-528.
Shi QY, Zhang SJ, Liu L, Chen QS, Yu LN, Zhang FJ, Yan M (2015b)Sevoflurane promotes the expansion of glioma stem cells through activation of hypoxia-inducible factors in vitro. Br J Anaesth 114:825-830.
Shi Y, Ping YF, Zhang X, Bian XW (2015c) Hostile Takeover: glioma stem cells recruit tams to support tumor progression. Cell Stem Cell 16:219-220.
Singh SK, Clarke ID, Hide T, Dirks PB (2004a) Cancer stem cells in nervous system tumors. Oncogene 23:7267-7273.
Singh SK, Clarke ID, Terasaki M, Bonn VE, Hawkins C, Squire J, Dirks PB (2003) Identification of a cancer stem cell in human brain tumors.Cancer Res 63:5821-5828.
Singh SK, Hawkins C, Clarke ID, Squire JA, Bayani J, Hide T, Henkelman RM, Cusimano MD, Dirks PB (2004b) Identification of human brain tumour initiating cells. Nature 432:396-401.
Song X, Xie T (2002) DE-cadherin-mediated cell adhesion is essential for maintaining somatic stem cells in the Drosophila ovary. Proc Natl Acad Sci U S A 99:14813-14818.
Song X, Zhu CH, Doan C, Xie T (2002) Germline stem cells anchored by adherens junctions in the Drosophila ovary niches. Science 296:1855-1857.
Sun C, Zhao D, Dai X, Chen J, Rong X, Wang H, Wang A, Li M, Dong J, Huang Q, Lan Q (2015) Fusion of cancer stem cells and mesenchymal stem cells contributes to glioma neovascularization. Oncol Rep 34:2022-2030.
Sun T, Zhang Z, Li B, Chen G, Xie X, Wei Y, Wu J, Zhou Y, Du Z (2013)Boron neutron capture therapy induces cell cycle arrest and cell apoptosis of glioma stem/progenitor cells in vitro. Radiat Oncol 8:195.
Sun T, Zhou Y, Xie X, Chen G, Li B, Wei Y, Chen J, Huang Q, Du Z (2012)Selective uptake of boronophenylalanine by glioma stem/progenitor cells. Appl Radiat Isot 70:1512-1518.
Uchida N, Buck DW, He D, Reitsma MJ, Masek M, Phan TV, Tsukamoto AS, Gage FH, Weissman IL (2000) Direct isolation of human central nervous system stem cells. Proc Natl Acad Sci U S A 97:14720-14725.
Wan Y, Fei XF, Wang ZM, Jiang DY, Chen HC, Yang J, Shi L, Huang Q (2012) Expression of miR-125b in the new, highly invasive glioma stem cell and progenitor cell line SU3. Chin J Cancer 31:207-214.
Wan Y, Sun G, Wang Z, Guo J, Shi L (2014) miR-125b promotes cell proliferation by directly targeting Lin28 in glioblastoma stem cells with low expression levels of miR-125b. Neuroreport 25:289-296.
Wang A, Dai X, Cui B, Fei X, Chen Y, Zhang J, Zhang Q, Zhao Y,Wang Z, Chen H, Lan Q, Dong J, Huang Q (2015a) Experimental research of host macrophage canceration induced by glioma stem progenitor cells. Mol Med Rep 11:2435-2442.
Wang F, Zhang P, Yang L, Yu X, Ye X, Yang J, Qian C, Zhang X, Cui YH,Bian XW (2015b) Activation of toll-like receptor 2 promotes invasion by upregulating MMPs in glioma stem cells. Am J Transl Res 7:607-615.
Wang JP, Huang Q, Zhang QB, Dong J, Zhu YD, Wang AD, Lan Q (2005)Isolation and preliminary identification of brain tumor stem cells in human glioma cell line SHG-44. Zhongguo Zhongliu Linchuang 32:604-606.
Wang WJ, Long LM, Yang N, Zhang QQ, Ji WJ, Zhao JH, Qin ZH,Wang Z, Chen G, Liang ZQ (2013) NVP-BEZ235, a novel dual PI3K/mTOR inhibitor, enhances the radiosensitivity of human glioma stem cells in vitro. Acta Pharmacol Sin 34:681-690.
Wang X, Low XC, Hou W, Abdullah LN, Toh TB, Mohd Abdul Rashid M, Ho D, Chow EK (2014) Epirubicin-adsorbed nanodiamonds kill chemoresistant hepatic cancer stem cells. ACS Nano 8:12151-12166.
Wang Z, Fei X, Dai X, Chen H, Tian H, Wang A, Dong J, Huang Q(2015c) Differentiation of glioma stem cells and progenitor cells into local host cell-like cells: a study based on choroidcarcinoma differentiation of choroid plexus of GFP transgenic nude mouse. Cancer Biother Radiopharm 30:225-232.
Wang Z, Wang B, Shi Y, Xu C, Xiao HL, Ma LN, Xu SL, Yang L, Wang QL, Dang WQ, Cui W, Yu SC, Ping YF, Cui YH, Kung HF, Qian C,Zhang X, Bian XW (2015d) Oncogenic miR-20a and miR-106a enhance the invasiveness of human glioma stem cells by directly targeting TIMP-2. Oncogene 34:1407-1419.
Ward RJ, Lee L, Graham K, Satkunendran T, Yoshikawa K, Ling E,Harper L, Austin R, Nieuwenhuis E, Clarke ID, Hui CC, Dirks PB(2009) Multipotent CD15+ cancer stem cells in patched-1-deficient mouse medulloblastoma. Cancer Res 69:4682-4690.
Wei Y, Jiang Y, Zou F, Liu Y, Wang S, Xu N, Xu W, Cui C, Xing Y, Liu Y, Cao B, Liu C, Wu G, Ao H, Zhang X, Jiang J (2013) Activation of PI3K/Akt pathway by CD133-p85 interaction promotes tumorigenic capacity of glioma stem cells. Proc Natl Acad Sci U S A 110:6829-6834.
Wick W, Meisner C, Hentschel B, Platten M, Schilling A, Wiestler B,Sabel MC, Koeppen S, Ketter R, Weiler M, Tabatabai G, von Deimling A, Gramatzki D, Westphal M, Schackert G, Loeffler M, Simon M,Reifenberger G, Weller M (2013) Prognostic or predictive value of MGMT promoter methylation in gliomas depends on IDH1 mutation. Neurology 81:1515-1522.
Yang W, Shen Y, Wei J, Liu F (2015) MicroRNA-153/Nrf-2/GPx1 pathway regulates radiosensitivity and stemness of glioma stem cells via reactive oxygen species. Oncotarget 6:22006-22027.
Yang W, Wei J, Guo T, Shen Y, Liu F (2014a) Knockdown of miR-210 decreases hypoxic glioma stem cells stemness and radioresistance.Exp Cell Res 326:22-35.
Yang X, Cui W, Yu S, Xu C, Chen G, Gu A, Li T, Cui Y, Zhang X, Bian X(2014b) A synthetic dl-nordihydroguaiaretic acid (Nordy), inhibits angiogenesis, invasion and proliferation of glioma stem cells within a zebrafish xenotransplantation model. PLoS One 9:e85759.
Yao CJ, Han TY, Shih PH, Yi TY, Lai IC, Chang KH, Lai TY, Chang CL,Lai GM (2014a) Elimination of cancer stem-like side population in human glioblastoma cells accompanied with stemness gene suppression by Korean herbal recipe MSC500. Integr Cancer Ther 13:541-554.
Yao X, Ping Y, Liu Y, Chen K, Yoshimura T, Liu M, Gong W, Chen C,Niu Q, Guo D, Zhang X, Wang JM, Bian X (2013) Vascular endothelial growth factor receptor 2 (VEGFR-2) plays a key role in vasculogenic mimicry formation, neovascularization and tumor initiation by Glioma stem-like cells. PLoS One 8:e57188.
Yao Y, Ma J, Xue Y, Wang P, Li Z, Liu J, Chen L, Xi Z, Teng H, Wang Z, Li Z, Liu Y (2015a) Knockdown of long non-coding RNA XIST exerts tumor-suppressive functions in human glioblastoma stem cells by up-regulating miR-152. Cancer Lett 359:75-86.
Yao Y, Wang X, Jin K, Zhu J, Wang Y, Xiong S, Mao Y, Zhou L (2008)B7-H4 is preferentially expressed in non-dividing brain tumor cells and in a subset of brain tumor stem-like cells. J Neurooncol 89:121-129.
Yao Y, Xue Y, Ma J, Shang C, Wang P, Liu L, Liu W, Li Z, Qu S, Li Z, Liu Y (2014b) MiR-330-mediated regulation of sh3gl2 expression enhances malignant behaviors of glioblastoma stem cells by activating erk and PI3K/AKT signaling pathways. PLoS One 9:e95060.
Yao YL, Ma J, Wang P, Xue YX, Li Z, Zhao LN, Li ZQ, Feng TD, Liu YH (2015b) miR-101 acts as a tumor suppressor by targeting Kruppel-like factor 6 in glioblastoma stem cells. CNS Neurosci Ther 21:40-51.
Ye F, Zhang Y, Liu Y, Yamada K, Tso JL, Menjivar JC, Tian JY, Yong WH, Schaue D, Mischel PS, Cloughesy TF, Nelson SF, Liau LM,McBride W, Tso CL (2013) Protective properties of radio-chemoresistant glioblastoma stem cell clones are associated with metabolic adaptation to reduced glucose dependence. PLoS One 8:e80397.
Ye X, Tam WL, Shibue T, Kaygusuz Y, Reinhardt F, Ng Eaton E, Weinberg RA (2015) Distinct EMT programs control normal mammary stem cells and tumour-initiating cells. Nature 525:256-260.
Yu SC, Ping YF, Yi L, Zhou ZH, Chen JH, Yao XH, Gao L, Wang JM,Bian XW (2008) Isolation and characterization of cancer stem cells from a human glioblastoma cell line U87. Cancer Lett 265:124-134.
Yu Z, Zhao G, Xie G, Zhao L, Chen Y, Yu H, Zhang Z, Li C, Li Y (2015)Metformin and temozolomide act synergistically to inhibit growth of glioma cells and glioma stem cells in vitro and in vivo. Oncotarget 6:32930-32943.
Yuan S, Lu Y, Yang J, Chen G, Kim S, Feng L, Ogasawara M, Hammoudi N, Lu W, Zhang H, Liu J, Colman H, Lee JS, Li XN, Xu RH, Huang P, Wang F (2015) Metabolic activation of mitochondria in glioma stem cells promotes cancer development through a reactive oxygen species-mediated mechanism. Stem Cell Res Ther 6:198.
Yuan S, Wang F, Chen G, Zhang H, Feng L, Wang L, Colman H, Keating MJ, Li X, Xu RH, Wang J, Huang P (2013) Effective elimination of cancer stem cells by a novel drug combination strategy. Stem Cells 31:23-34.
Zhang FL, Wang P, Liu YH, Liu LB, Liu XB, Li Z, Xue YX (2013a) Topoisomerase I inhibitors, shikonin and topotecan, inhibit growth and induce apoptosis of glioma cells and glioma stem cells. PLoS One 8:e81815.
Zhang G, Jin G, Nie X, Mi R, Zhu G, Jia W, Liu F (2014a) Enhanced antitumor efficacy of an oncolytic herpes simplex virus expressing an endostatin-angiostatin fusion gene in human glioblastoma stem cell xenografts. PLoS One 9:e95872.
Zhang J, Niu C, Ye L, Huang H, He X, Tong WG, Ross J, Haug J, Johnson T, Feng JQ, Harris S, Wiedemann LM, Mishina Y, Li L (2003)Identification of the haematopoietic stem cell niche and control of the niche size. Nature 425:836-841.
Zhang L, Ren X, Cheng Y, Liu X, Allen JE, Zhang Y, Yuan Y, Huang SY,Yang W, Berg A, Webb BS, Connor J, Liu CG, Lu Z, El-Deiry WS,Yang JM (2014b) The NFkappaB inhibitor, SN50, induces differentiation of glioma stem cells and suppresses their oncogenic phenotype.Cancer Biol Ther 15:602-611.
Zhang QB, Ji XY, Huang Q, Dong J, Zhu YD, Lan Q (2006) Differentiation profile of brain tumor stem cells: a comparative study with neural stem cells. Cell Res 16:909-915.
Zhang S, Xie R, Wan F, Ye F, Guo D, Lei T (2013b) Identification of U251 glioma stem cells and their heterogeneous stem-like phenotypes. Oncol Lett 6:1649-1655.
Zhang S, Xie R, Zhao T, Yang X, Han L, Ye F, Lei T, Wan F (2014c) Neural stem cells preferentially migrate to glioma stem cells and reduce their stemness phenotypes. Int J Oncol 45:1989-1996.
Zhao Y, Dong J, Huang Q, Lou M, Wang A, Lan Q (2010a) Endothelial cell transdifferentiation of human glioma stem progenitor cells in vitro. Brain Res Bull 82:308-312.
Zhao Y, Huang Q, Wang A, Dong J, Lan Q (2009) Mutation of PTEN in glioma stem/progenitor cells: a case report. Cancer Genet Cytogenet 195:183-185.
Zhao Y, Huang Q, Yang J, Lou M, Wang A, Dong J, Qin Z, Zhang T(2010b) Autophagy impairment inhibits differentiation of glioma stem/progenitor cells. Brain Res 1313:250-258.
Zheng J, Li XD, Wang P, Liu XB, Xue YX, Hu Y, Li Z, Li ZQ, Wang ZH,Liu YH (2015) CRNDE affects the malignant biological characteristics of human glioma stem cells by negatively regulating miR-186.Oncotarget 6:25339-25355.
Zheng X, Shen G, Yang X, Liu W (2007) Most C6 cells are cancer stem cells: evidence from clonal and population analyses. Cancer Research 67:3691-3697.
Zheng X, Xie Q, Li S, Zhang W (2011) CXCR4-positive subset of glioma is enriched for cancer stem cells. Oncol Res 19:555-561.
Zhitao J, Long L, Jia L, Yunchao B, Anhua W (2015) Temozolomide sensitizes stem-like cells of glioma spheres to TRAIL-induced apoptosis via upregulation of casitas B-lineage lymphoma (c-Cbl) protein.Tumour Biol 36:9621-9630.
Zhou J, Yi L, Ouyang Q, Xu L, Cui H, Xu M (2014) Neurotensin signaling regulates stem-like traits of glioblastoma stem cells through activation of IL-8/CXCR1/STAT3 pathway. Cellular signalling 26:2896-2902.
Zhou X, Zheng C, Shi Q, Li X, Shen Z, Yu R (2012) Isolation, cultivation and identification of brain glioma stem cells by magnetic bead sorting. Neural Regen Res 7:985-992.
Zhu G, Su W, Jin G, Xu F, Hao S, Guan F, Jia W, Liu F (2011) Glioma stem cells targeted by oncolytic virus carrying endostatin-angiostatin fusion gene and the expression of its exogenous gene in vitro. Brain Res 1390:59-69.
Zhu J, Wang H, Fan Y, Hu Y, Ji X, Sun Q, Liu H (2014a) Knockdown of nuclear factor erythroid 2-related factor 2 by lentivirus induces differentiation of glioma stem-like cells. Oncol Rep 32:1170-1178.
Zhu J, Wang H, Ji X, Zhu L, Sun Q, Cong Z, Zhou Y, Liu H, Zhou M(2014b) Differential Nrf2 expression between glioma stem cells and non-stem-like cells in glioblastoma. Oncol Lett 7:693-698.
Zhu J, Wang H, Sun Q, Ji X, Zhu L, Cong Z, Zhou Y, Liu H, Zhou M(2013) Nrf2 is required to maintain the self-renewal of glioma stem cells. BMC Cancer 13:380.
Zhuang W, Long L, Zheng B, Ji W, Yang N, Zhang Q, Liang Z (2012)Curcumin promotes differentiation of glioma-initiating cells by inducing autophagy. Cancer Sci 103:684-690.
- 中国神经再生研究(英文版)的其它文章
- The role of general anesthetics and the mechanisms of hippocampal and extra-hippocampal dysfunctions in the genesis of postoperative cognitive dysfunction
- Saponins from Panax japonicus attenuate age-related neuroinflammation via regulation of the mitogenactivated protein kinase and nuclear factor kappa B signaling pathways
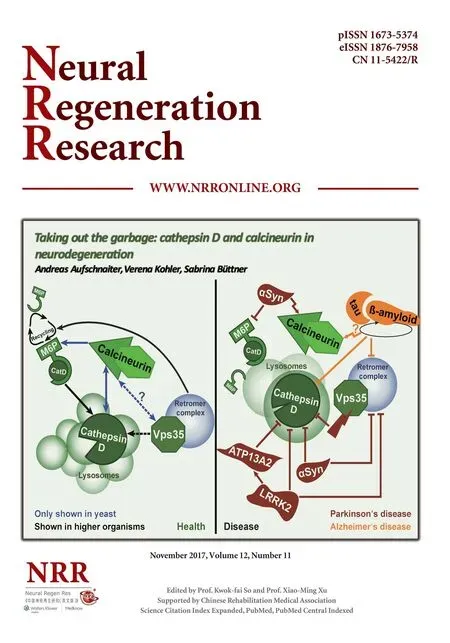
- Taking out the garbage: cathepsin D and calcineurin in neurodegeneration
- MicroRNAs as diagnostic markers and therapeutic targets for traumatic brain injury
- Interferon regulatory factor 2 binding protein 2: a new player of the innate immune response for stroke recovery
- Endogenous retinal neural stem cell reprogramming for neuronal regeneration