骨质疏松性椎体压缩骨折PKP术后长期效果不佳的危险因素分析
王中英 侯建文 王其尊 郭建伟 王亭 李书忠

[摘要]目的 探討骨质疏松性椎体压缩骨折(OVCF)经皮穿刺椎体后凸成形术(PKP)治疗后疗效不佳的相关因素。方法 回顾性分析本院2016年1月—2017年12月因OVCF行PKP的201例病人的临床资料。病人术后随访12.0~36.0个月,平均25.5个月,根据随访影像学结果分为效果良好组和效果不佳组。对两组病人的性别、年龄、身高、体质量、体质量指数(BMI)、伤椎数、抗骨质疏松治疗、骨水泥分布类型、骨水泥渗漏、骨水泥用量、Cobb角恢复度等进行单因素分析,并对单因素分析差异有统计学意义者进行多因素Logistic回归分析。结果 单因素分析显示,两组抗骨质疏松治疗、骨水泥分布类型、骨水泥用量及Cobb角恢复度存在统计学差异(χ2=11.015、33.091,t=7.200、12.530,P<0.01);多因素Logistic回归分析结果显示,抗骨质疏松治疗(OR=3.903)、骨水泥分布类型(OR=0.123)、骨水泥用量(OR=0.168)以及Cobb角恢复度(OR=0.008)均为PKP术后疗效不佳的影响因素。结论 无抗骨质疏松治疗、致密型骨水泥分布类型、过度骨水泥用量以及Cobb角恢复过度是造成OVCF病人PKP术后疗效不佳的独立危险因素。
[关键词] 椎体后凸成形术;骨折,压缩性;骨质疏松性骨折;治疗结果;危险因素
[中图分类号] R687.4[文献标志码] A[文章编号] 2096-5532(2020)04-0427-05
doi:10.11712/jms.2096-5532.2020.56.052
[网络出版] http://kns.cnki.net/kcms/detail/37.1517.r.20200325.1005.004.html;2020-03-026 13:58
AN ANALYSIS OF RISK FACTORS FOR POOR LONG-TERM OUTCOME AFTER PERCUTANEOUS KYPHOPLASTY FOR OSTEOPOROTIC VERTEBRAL COMPRESSION FRACTURES
WANG Zhongying, HOU Jianwen, WANG Qizun, GUO Jianwei, WANG Ting, LI Shuzhong
(Department of Orthopedics, The Affiliated Hospital of Qingdao University, Qingdao 266021, China)
[ABSTRACT]Objective To investigate the factors associated with poor efficacy of percutaneous kyphoplasty (PKP) for osteoporotic vertebral compression fractures (OVCF).Methods The clinical data of 201 patients with OVCF who underwent PKP from January 2016 to December 2017 in our hospital were retrospectively analyzed. The patients were followed up for 12.0 to 36.0 months after operation, with an average of 25.5 months. According to the imaging results at follow-up, they were divided into good-outcome group and poor-outcome group. Univariate analysis was conducted for comparing the differences between the two groups in terms of sex, age, body height, body weight, body mass index, the number of injured vertebrae, anti-osteoporosis treatment, the distribution of bone cement, the leakage of bone cement, the amount of bone cement, and the degree of Cobb angle correction. The significant variables derived from the univariate analysis were further analyzed by Logistic regression analysis. Results Univariate analysis showed significant between-group differences in anti-osteoporosis treatment, the distribution of bone cement, the amount of bone cement, and the degree of Cobb angle correction (χ2=11.015,33.091;t=7.200,12.530;P<0.01). Multivariate Logistic regression analysis showed that anti-osteoporosis treatment (odds ratio (OR)=3.903), the distribution of bone cement (OR=0.123), the amount of bone cement (OR=0.168), and the degree of Cobb angle correction (OR=0.008) were inf-luencing factors for poor efficacy of PKP.Conclusion An absence of anti-osteoporosis therapy, a dense distribution of bone cement, excessive bone cement, and excessive Cobb angle correction are independent risk factors for poor efficacy of PKP in OVCF patients.
[KEY WORDS] kyphoplasty; fractures, compression; osteoporotic fractures; treatment outcome; risk factors
在我国,骨质疏松性椎体压缩骨折(OVCF)已经成为影响中老年人生活质量的重要疾病之一[1]。在世界各地,每年新发的OVCF有100余万例[2]。目前治疗OVCF的方式多种多样,保守治疗方式包括抗骨质疏松、卧床休息、抗凝、镇痛、佩戴支具等。但由于OVCF的症状缓解时间较长,病人常常因持续性腰背痛导致生活质量严重下降,从而大大增加神经系统并发症的发生率和病死率[3]。经皮穿刺椎体后凸成形术(PKP)是目前大家比較认可的治疗OVCF的方式,具有手术创伤小、病人恢复快、缓解疼痛效果明显等优点[4]。PKP的短期手术效果明显优于保守治疗[5],但其长期效果存在争议[6]。本次研究通过长期随访,回顾性分析PKP术后疗效不佳的危险因素,旨在为今后OVCF病人的治疗提供参考。现将结果报告如下。
1 资料与方法
1.1 病例选择
本次研究选择2016年1月—2017年12月在我院接受PKP治疗的OVCF病人。病人均因腰背部疼痛就诊,有或无明显外伤史,术前均行X线片、CT及核磁共振成像(MRI)、骨密度测定等检查,明确伤椎数量和部位、椎体水肿情况、椎体后壁完整性、有无脊髓及神经根压迫症状等。纳入标准:①符合骨质疏松(T≤-2.0)诊断;②X线检查确诊为胸椎或腰椎椎体压缩性骨折;③CT检查明确受伤椎体后壁完整;④临床表现主要为严重的腰背痛,无脊髓及神经根症状;⑤既往未发生过椎体骨折;⑥病人行PKP治疗,临床与随访资料完整。排除标准:①转移性骨肿瘤等所致病理性椎体骨折者;②严重暴力等外伤性椎体压缩性骨折;③椎体后壁破坏,有脊髓或神经根压迫症状。共纳入201例OVCF病人,男42例,女159例;年龄(72.56±9.23)岁;骨折椎体共271个,多集中于T11~L2。
1.2 研究方法
①分组:术后随访12~30个月,平均25.5个月,根据随访X线或三维CT等影像学检查结果,将存在椎体再骨折、邻近椎体骨折或骨水泥移位等表现者归为效果不佳组,骨水泥位置良好、无上述表现者归为效果良好组。②分别于术前、术后3 d和末次随访时,采用视觉模拟评分法(VAS)评估病人的疼痛程度,采用Oswestry功能障碍指数(ODI)评价病人功能恢复情况。③根据相关文献报道[7-8],对PKP术后疗效不佳可能存在的危险因素,包括性别、年龄、身高、体质量、体质量指数(BMI)、伤椎数、抗骨质疏松治疗、骨水泥渗漏、骨水泥分布类型(弥散型和致密型)、骨水泥用量、Cobb角恢复度、高血压、糖尿病等,进行单因素分析和多因素Logistic回归分析。其中Cobb角恢复度=术后Cobb角-术前Cobb角。
1.3 统计学分析
采用SPSS 20.0统计软件对所得数据进行统计学分析。正态分布的计量资料以[AKx-D]±s表示,组间比较采用t检验;计数资料以例数表示,组间比较采用卡方检验。对单因素分析中差异有显著性的危险因素,采用多因素Logistic回归模型进行分析。以P<0.05为差异有统计学意义。
2 结果
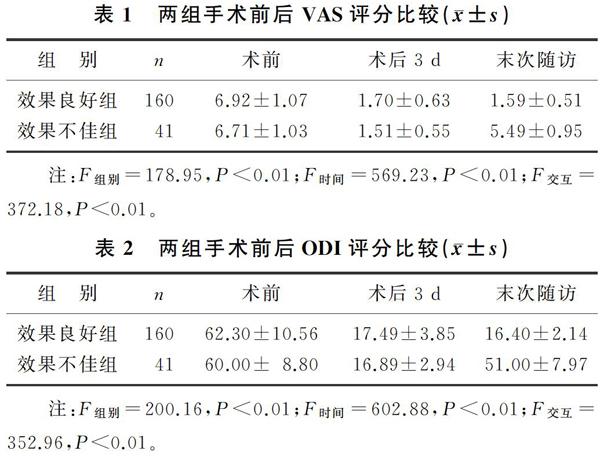
2.1 两组手术前后VAS和ODI评分比较
本文201例OVCF病人中,效果不佳组41例,效果良好组160例。术后3 d与术前相比较,两组病人VAS、ODI评分均明显降低,差异有统计学意义(F=159.42~225.72,P<0.01),说明两组术后近期效果良好。术前、术后3 d时,两组VAS、ODI评分比较差异无显著性(P>0.05);而末次随访时,两组VAS、ODI评分比较差异有显著意义(F=4.050、4.583,P<0.01)。见表1、2。
2.2 单因素分析
两组间相比,性别、年龄、身高、体质量、BMI、伤椎数、骨水泥渗漏、高血压及糖尿病差异无统计学意义(P>0.05),而抗骨质疏松治疗、骨水泥分布类型、Cobb角恢复度以及骨水泥用量差异有显著性(χ2=11.015、33.091,t=7.200、12.530,P<0.01)。见表3。
2.3 多因素Logistic回归分析
对上述4项存在统计学差异的因素进行多因素Logistic回归分析,结果显示,抗骨质疏松治疗、骨水泥分布类型、骨水泥用量以及Cobb角恢复度均为PKP术后疗效不佳的影响因素,其中保护因素为术后抗骨质疏松治疗(OR=3.903),危险因素为致密型骨水泥分布类型(OR=0.123)、骨水泥用量过多(OR=0.168)以及Cobb角恢复度过大(OR=0.008)。见表4。
3 讨论
目前,全世界骨质疏松的中老年人已有1亿人,而其中约1/4的停经后女性受到OVCF的危害[9]。PKP是目前治疗OVCF的重要手术方式之一。由于其创伤小、效果好、操作简单等特点,目前PKP已经广泛应用于临床。但随着PKP在临床的应用增多,其术后疗效不佳的原因也逐渐引起国内外学者的关注。本研究201例病人中,有41例术后效果不佳,将病人分为效果不佳组和效果良好组进行单因素分析显示,两组病人性别、年龄、身高、体质量、BMI、骨水泥渗漏以及伤椎数量等差异无统计学意义。既往研究表明,骨水泥渗漏以及伤椎数量是OVCF病人PKP术后效果不佳的危险因素[10-11]。但本研究中二者并不影响手术效果,而抗骨质疏松治疗、骨水泥分布类型、骨水泥用量以及Cobb角恢复度是PKP治疗OVCF病人术后效果不佳的危险因素。
PKP治疗OVCF已取得良好的近期效果,不仅能短期内缓解疼痛,还可以使病人尽早下地活动,大大减少老年人卧床休息引起的并发症[12]。但PKP术后规范长期的抗骨质疏松治疗往往被忽视。本研究中,效果不佳组抗骨质疏松治疗病人仅有13例,抗骨质疏松治疗率仅为31.7%。而SUN等[13]研究认为,OVCF病人PKP术后再发生椎体骨折等并发症为骨质疏松的自然病程。KIM等[14]研究表明,骨密度T值越低,术后其他椎体骨折的发生率越高。KAUFMAN等[15]报道,OVCF病人PKP术后骨密度T值每提高1%,其发生再骨折等的风险降低3%。故术后规范的抗骨质疏松治疗对降低其他椎体骨折的发生率有重要意义[16]。ZHANG等[17]也强调,PKP术后应进行规范的抗骨质疏松治疗。因此,在PKP术后,应指导病人坚持长期规范的抗骨质疏松治疗,以降低其他椎体骨折再发生的概率。
本文研究结果表明,骨水泥用量并不是越多越好。这与JIN等[18]研究认为的骨水泥注射量越多,邻近椎体骨折风险越高的观点相同。LIN等[19]研究显示,骨水泥注入量与PKP术后邻近椎体骨折呈正相关。本研究中效果不佳组骨水泥用量明显高于效果良好组。骨水泥用量过多会增加骨水泥渗漏风险。本研究中发生骨水泥渗漏病人42例,发生率为20.9%,略高于有关文献报道的7%~15%[20-21],其中效果不佳组发生9例,发生率为22.0%。此外,骨水泥用量还会影响骨水泥在伤椎内的分布类型。KIM等[22]研究认为,PKP术后骨水泥多为致密型(团块型)分布。本研究通过术后X线或术后CT判断骨水泥在術椎内的弥散情况,结果显示,效果不佳组骨水泥为致密型分布者27例,占65.9%。而有研究结果表明,骨水泥分布呈致密型是影响OVCF病人PKP术后效果的危险因素[23-24]。骨水泥呈致密型分布,会导致骨水泥在术椎内分布不均匀,使手术椎体无法获得理想的生物力学支撑,增加术后椎体再骨折的风险。LIANG等[25]研究发现,骨水泥分布呈致密型(团块状),会使周围松质骨的最大冯米斯应力增加,进而破坏周围区域的松质骨,从而增加手术后再骨折风险。因此行PKP时,应提高骨水泥注射技巧,尽量使骨水泥均匀弥散在术椎内[26]。国内有相关研究结果表明,低黏度的骨水泥有利于骨
水泥在手术椎体内的弥散,但其会增加发生骨水泥渗漏的风险[27-28]。而高黏度的骨水泥大大降低了骨水泥渗漏的风险,但不利于骨水泥在手术椎体内的弥散[29]。因此,建议在行PKP时按次序依次注入不同黏度的骨水泥:先注入少量的高黏度的骨水泥用以封堵伤椎外周空隙,然后缓慢注入相对低黏度的骨水泥,使其在伤椎内充分均匀弥散;其次,操作过程中在C臂X线全程透视下注射骨水泥,密切关注骨水泥弥散方向及形态,以保证更加安全地增加骨水泥在手术椎体内的弥散。
此外,骨水泥用量过多,还会导致术椎Cobb角恢复度过大。术后Cobb角恢复度过大是影响手术效果的危险因素[30-31]。有研究认为,Cobb角恢复过高和新发术后椎体骨折呈正相关[32-34]。这可能是由于过高恢复Cobb角引起生物力学改变造成的,术后Cobb角恢复过高,致使周围软组织张力增加,进而增加术椎与邻近椎体的应力以及椎体间的不稳定性,从而影响手术效果[35-36]。
综上所述,PKP治疗OVCF的短期效果值得肯定;从长期效果分析,术中骨水泥用量、骨水泥的分布类型、Cobb角恢复度以及抗骨质疏松治疗均为PKP术后疗效不佳的影响因素。因此,OVCF病人在PKP中不宜追求骨折椎体完美复位,后凸Cobb角的适度恢复可使病人术后长期效果更佳;在骨水泥方面,术中应重视骨水泥的弥散情况以及用量;术后应指导病人进行长期规范化的抗骨质疏松治疗,提高病人的术后长期效果。
[参考文献]
[1]SUN Zhiyong, LI Xuefeng, ZHAO Huan, et al. Percutaneous balloon kyphoplasty in treatment of painful osteoporotic occult vertebral fracture: a retrospective study of 89 cases[J]. Medical Science Monitor: International Medical Journal of Experimental and Clinical Research, 2017,23:1682-1690.
[2]JOHNELL O, KANIS J A. An estimate of the worldwide prevalence and disability associated with osteoporotic fractures[J]. Osteoporosis International: a Journal Established as Result of Cooperation Between the European Foundation for Osteoporosis and the National Osteoporosis Foundation of the USA, 2006,17(12):1726-1733.
[3]STEPHENSON M B, GLAENZER B, MALAMIS A. Percutaneous minimally invasive techniques in the treatment of spinal metastases[J]. Current Treatment Options in Oncology, 2016,17(11):56.
[4]GUARNIERI G, MASALA S, MUTO M. Update of vertebral cementoplasty in porotic patients[J]. Interventional Neuroradiology: Journal of Peritherapeutic Neuroradiology, Surgical Procedures and Related Neurosciences, 2015,21(3):372-380.
[5]YOKOYAMA K, KAWANISHI M, YAMADA M, et al. Long-term therapeutic effects of vertebroplasty for painful vertebral compression fracture: a retrospective comparative study[J]. British Journal of Neurosurgery, 2017,31(2):184-188.
[6]KLAZEN C H, LOHLE P M, VRIES J D, et al. Vertebroplasty versus conservative treatment in acute osteoporotic vertebral compression fractures (Vertos Ⅱ): an open-label randomised trial[J]. The Lancet, 2010,376(9746):1085-1092.
[7]LI Yongxian, GUO Danqing, ZHANG Shuncong, et al. Risk factor analysis for re-collapse of cemented vertebrae after percutaneous vertebroplasty (PVP) or percutaneous kyphoplasty (PKP)[J]. International Orthopaedics, 2018,42(9):2131-2139.
[8]HU K Z, CHEN S C, XU L. Comparison of percutaneous balloon dilation kyphoplasty and percutaneous vertebroplasty in treatment for thoracolumbar vertebral compression fractures[J]. European Review for Medical and Pharmacological Sciences, 2018,22(1):96-102.
[9]LEXANDRU D, SO W. Evaluation and management of vertebral compression fractures[J]. Permanente Journal, 2012,16(4):46-51.
[10]WU Jian, GUAN Yuehong, FAN Shengli. Risk factors of non-surgical vertebral fracture after percutaneous kyphoplasty of single segment thoracolumbar fracture[J]. China Journal of Orthopaedics and Traumatology, 2017,30(9):833-837.
[11]KIM S H, CHOI H S, RHEE Y, et al. Prevalent vertebral fractures predict subsequent radiographic vertebral fractures in postmenopausal Korean women receiving antiresorptive agent[J]. Osteoporosis International: a Journal Established as Result of Cooperation Between the European Foundation for Osteoporosis and the National Osteoporosis Foundation of the USA, 2011,22(3):781-787.
[12]BUCHBINDER R, OSBORNE R H, EBELING P R, et al. A randomized trial of vertebroplasty for painful osteoporotic vertebral fractures[J]. New England Journal of Medicine, 2009,361(6):557-568.
[13]SUN Gang, TANG Hai, LI Min, et al. Analysis of risk factors of subsequent fractures after vertebroplasty[J]. European Spine Journal: Official Publication of the European Spine So-ciety, the European Spinal Deformity Society, and the Euro-pean Section of the Cervical Spine Research Society, 2014,23(6):1339-1345.
[14]KIM M H, LEE A S, MIN S H, et al. Risk factors of new compression fractures in adjacent vertebrae after percutaneous vertebroplasty[J]. Asian Spine Journal, 2011,5(3):180-187.
[15]KAUFMAN J M, PALACIOS S, SILVERMAN S, et al. An evaluation of the Fracture Risk Assessment Tool (FRAX) as an indicator of treatment efficacy: the effects of bazedoxifene and raloxifene on vertebral, nonvertebral, and all clinical frac-tures as a function of baseline fracture risk assessed by FRAX[J]. Osteoporosis International: a Journal Established as Result of Cooperation Between the European Foundation for Osteoporosis and the National Osteoporosis Foundation of the USA, 2013,24(10):2561-2569.
[16]BAWA H S, WEICK J, DIRSCHL D R. Anti-osteoporotic therapy after fragility fracture lowers rate of subsequent fracture: analysis of a large population sample[J]. The Journal of Bone and Joint Surgery. American Volume, 2015,97(19):1555-1562.
[17]ZHANG Kaining, SHEN Yingchun, REN Yanjun, et al. Prevention and treatment of bone cement-related complications in patients receiving percutaneous kyphoplasty[J]. International Journal of Clinical and Experimental Medicine, 2015,8(2):2371-2377.
[18]JIN Y J, YOON S H, PARK K W, et al. The volumetric analysis of cement in vertebroplasty: relationship with clinical outcome and complications[J]. Spine, 2011,36(12):E761-E772.
[19]LIN Dasheng, HAO Jianming, LI Lin, et al. Effect of bone cement volume fraction on adjacent vertebral fractures after unilateral percutaneous kyphoplasty[J]. Journal of Spinal Di-
sorders & Techniques, 2016,30(3):E270-E275.
[20]BERGMANN M, OBERKIRCHER L, BLIEMEL C, et al. Early clinical outcome and complications related to balloon kyphoplasty[J]. Orthopedic Reviews, 2012,4(2):e25.
[21]TOM-BERMEJO F, PIERA A R, DURAN-ALVAREZ C, et al. Identification of risk factors for the occurrence of cement leakage during percutaneous vertebroplasty for painful osteoporotic or malignant vertebral fracture[J]. Spine, 2014,39(11):E693-E700.
[22]KIM Y Y, RHYU K W. Recompression of vertebral body after balloon kyphoplasty for osteoporotic vertebral compression fracture[J]. European Spine Journal: Official Publication of the European Spine Society, the European Spinal Deformity Society, and the European Section of the Cervical Spine Research Society, 2010,19(11):1907-1912.
[23]謝清华,陈忠羡,薛忠林,等. 计算机术前设计辅助椎体成形术治疗重度骨质疏松性椎体压缩骨折[J]. 中国医药科学, 2016,6(12):22-25,72.
[24]CHEN L H, HSIEH M K, LIAO J C, et al. Repeated percutaneous vertebroplasty for refracture of cemented vertebrae[J]. Archives of Orthopaedic and Trauma Surgery, 2011,131(7):927-933.
[25]LIANG De, YE Linqiang, JIANG Xiaobing, et al. Biomecha-
nical effects of cement distribution in the fractured area on osteoporotic vertebral compression fractures: a three-dimensio-
nal finite element analysis[J]. Journal of Surgical Research, 2015,195(1):246-256.
[26]HE X, LI H, MENG Y, et al. Percutaneous kyphoplasty eva-luated by cement volume and distribution: an analysis of clinical data.[J]. Pain Physician, 2016,19(7):495.
[27]刘洋. 不同黏度骨水泥椎体成形系统治疗骨质疏松性椎体压缩性骨折的比较[J]. 中国组织工程研究, 2018,22(30):4774-4781.
[28]张亮,王静成,冯新民,等. 不同黏度骨水泥椎体成形术治疗重度骨质疏松性骨折的疗效研究[J]. 实用骨科杂志, 2016,22(7):577-581.
[29]康健,冯大雄. 高粘度与低粘度骨水泥椎体成形术在治疗骨质疏松椎体压缩性骨折中的价值比较[J]. 颈腰痛杂志, 2018,39(4):468-470.
[30]CHIU Y C, YANG S C, CHEN H S, et al. Clinical evaluation of repeat percutaneous vertebroplasty for symptomatic cemented vertebrae[J]. Journal of Spinal Disorders & Techniques, 2012,25(8):E245-E253.
[31]KANG S K, LEE C W, PARK N K, et al. Predictive risk factors for refracture after percutaneous vertebroplasty[J]. Annals of Rehabilitation Medicine, 2011,35(6):844-851.
[32]LI Xigong, LU Yang, LIN Xiangjin. Refracture of osteoporo-tic vertebral body after treatment by balloon kyphoplasty: three cases report[J]. Medicine, 2017,96(49):e8961.
[33]LI Dapeng, WU Yan, HUANG Yonghui, et al. Risk factors of recompression of cemented vertebrae after kyphoplasty for osteoporotic vertebral compression fractures[J]. International Orthopaedics, 2016,40(6):1285-1290.
[34]BORENSZTEIN M, CAMINO W G, POSADASM M, et al. Analysis of risk factors for new vertebral fracture after percutaneous vertebroplasty[J]. GlobalSpineJ, 2018,8(5):446-452.
[35]KIM Y J, LEE J W, KIM K J, et al. Percutaneous vertebroplasty for intravertebral cleft: analysis of therapeutic effects and outcome predictors[J]. Skeletal Radiology, 2010,39(8):757-766.
[36]BAEK S W, KIM C, CHANG H. The relationship between the spinopelvic balance and the incidence of adjacent vertebral fractures following percutaneous vertebroplasty[J]. Osteoporosis International, 2015,26(5):1507-1513.
(本文編辑 马伟平)
[收稿日期]2019-07-06; [修订日期]2020-02-23
[基金项目]山东省自然科学基金项目(ZR2016HM31)
[第一作者]王中英(1991-),男,硕士研究生。
[通信作者]李书忠(1958-),男,硕士,教授,主任医师,博士生导师。E-mail:yfylsz2018@126.com。王亭(1972-),男,博士后,主任医师,硕士生导师。E-mail:qyfywt2018@126.com。