基于美国FAERS的新型口服抗凝药物致女性生殖系统异常出血风险的数据分析
田晓江 贾运涛 王柯静 陈琳


中圖分类号 R973+.2 文献标志码 A 文章编号 1001-0408(2020)14-1751-05
DOI 10.6039/j.issn.1001-0408.2020.14.16
摘 要 目的:评价新型口服抗凝药(NOACs)致女性生殖系统异常出血的风险。方法:收集2004年1月1日-2019年5月31日美国FDA不良事件报告系统(FAERS)数据库中收录的以“达比加群酯”“利伐沙班”“阿哌沙班”“依度沙班”等4种NOACs为首要怀疑药物的女性生殖系统异常出血的不良事件(ADE)报告,采用报告比值比法(ROR)对NOACs致女性生殖系统异常出血事件进行信号检测。结果:FAERS数据库中共收录涉及NOACs致女性生殖系统异常出血的ADE报告2 658份,其中达比加群酯330份、利伐沙班2 049份、阿哌沙班267份、依度沙班12份。达比加群酯、阿哌沙班、依度沙班诱发女性生殖系统异常出血的患者均以≥75岁为主,分别占37.27%、36.70%、58.33%;利伐沙班以45~64岁为主,占33.04%。达比加群酯、利伐沙班、阿哌沙班、依度沙班致严重的不良事件的发生率分别为96.36%、84.53%、47.19%、58.33%,均以住院/住院时间延长为主(分别占64.78%、90.01%、86.51%、71.43%)。共检测到12个可疑信号,涉及出血部位包括宫颈、输卵管、卵巢、盆腔、子宫、阴道、尿路等。其中,利伐沙班的可疑信号有11个,出血事件主要表现为阴道血肿[ROR=12.07,95%CI(8.51,17.12)]、绝经后出血[ROR=9.89,95%CI(8.31,11.77)]、盆腔血肿[ROR=7.68,95%CI(5.66,10.43)]等;达比加群酯、阿哌沙班、依度沙班的可疑信号分别有4、4、2个,阿哌沙班[ROR=5.18,95%CI(1.81,5.85)]和依度沙班[ROR=48.19,95%CI(6.76,343.77)]均以阴道血肿为主;达比加群酯以盆腔血肿[ROR=12.56,95%CI(8.92,17.70)]信号最强,其次为尿路出血[ROR=5.41,95%CI(3.34,8.76)]和盆腔出血[ROR=2.53,95%CI(1.88,3.40)]。结论:4种NOACs均可诱发女性生殖系统异常出血,且严重的不良事件发生率较高,常需住院治疗或延长住院时间。利伐沙班的出血风险最高,表现为阴道血肿、绝经后出血及盆腔血肿;达比加群酯以盆腔血肿为主,阿哌沙班和依度沙班均为阴道血肿为主。
关键词 新型口服抗凝药;女性;生殖系统异常出血;信号检测;不良事件;用药安全;美国FDA不良反应报告系统
Data Analysis of the Risks of Abnormal Female Reproductive System Haemorrhages Induced by Novel Oral Anticoagulants Based on FAERS
TIAN Xiaojiang1,JIA Yuntao2,WANG Kejing1,CHEN Lin1(1. Dept. of Pharmacy, Chongqing Health Center for Women and Children, Chongqing 400021 China; 2. Dept. of Pharmacy, Childrens Hospital of Chongqing Medical University, Chongqing 400014, China)
ABSTRACT OBJECTIVE: To evaluate the risk of abnormal female reproductive system haemorrhage induced by novel oral anticoagulants (NOACs). METHODS: The abnormal female reproductive system haemorrhage reports induced by 4 kinds of NOACs as “dabigatran etexilate”, “rivaroxaban”, “apixaban” and “edoxaban” were used as the first suspected dugs to collected from FDA adverse event reporting system (FAERS) database during Jan. 1st, 2004-May 31st, 2019. The report odd ratio (ROR) method was used to detect the signal of abnormal female reproductive system haemorrhage induced by NOACs. RESULTS: A total of 2 658 adverse events related to abnormal female reproductive system haemorrhage were collected from FAERS database, involving 330 reports of dabigatran etexilate, 2 049 reports of rivaroxaban, 267 reports of apixaban, and 12 reports of edoxaban. The abnormal female reproductive system haemorrhage caused by dabigatran etexilate, apixaban and edoxaban mainly occurred in patients aged 75 and older, accounting for 37.27%, 36.70% and 58.33% respectively; that of rivaroxaban mainly occurred in patients with 45-64 years old, accounting for 33.04%. The incidence of severe adverse events (SAE) induced by dabigatran etexilate, rivaroxaban, apixaban and edoxaban were 96.36%, 84.53%,47.19% and 58.33%, respectively. All of patients in the included reports were mainly hospitalized and hospitalization stay was prolonged, accounting for 64.78%, 90.01%, 86.51% and 71.43%, respectively. A total of 12 suspected signals were detected, involving cervix uteri, fallopian tube, ovary, pelvis cavity, uterus, vagina, urinary tract, etc. Among them, there were 11 positive signals of rivaroxaban, and the bleeding events were concentrated in vaginal hematoma [ROR=12.07, 95%CI(8.51, 17.12)], postmenopausal hemorrhage [ROR=9.89, 95%CI(8.31, 11.77)], pelvic hematoma [ROR=7.68, 95%CI(5.66, 10.43)]. There were 4, 4 and 2 suspicious signals for dabigatran etexilate, apixaban and edoxaban. The main bleeding events of both apixaban [ROR=5.18, 95%CI(1.81,5.85)] and edoxaban [ROR=48.19,95%CI(6.76,343.77)] were vaginal hematoma; dabigatran etexilate-induced pelvic hematoma [ROR=12.56, 95%CI(8.92,17.70)] had the strongest signal, followed by urinary tract bleeding [ROR=5.41, 95%CI(3.34,8.76)] and pelvic hemorrhage [ROR=2.53, 95%CI(1.88,3.40)]. CONCLUSIONS: Totally 4 kinds of NOACs can cause abnormal female reproductive system haemorrhage, and the incidence of SAE is high, of requiring hospitalization or prolonging hospitalization time. The risk of haemorrhage in rivaroxaban is the highest, usually manifesting as vaginal hematoma, postmenopausal hemorrhage and pelvic hematoma. Dabigatran etexilate mainly induce pelvic hematoma, while apixaban and edoxaban are mainly cause vaginal hematoma.
KEYWORDS Novel oral anticoagulants; Female; Abnormal female reproductive system haemorrhage; Signal detection; Adverse drug event; Drug use safety; FDA adverse event reporting system
血栓形成和栓塞是多种全身性疾病的常见并发症,而抗凝是主要治疗手段[1]。常用的抗凝药物主要有低分子肝素类、维生素K拮抗药及新型口服抗凝药(Novel oral anticoagulants,NOACs)等。相对于前两类抗凝药物,NOACs具有起效快、治疗窗宽、个体差异小等优点,现已成为预防和治疗血栓栓塞性疾病的重要药物[2-4]。但有研究认为,NOACs可诱发消化道出血、颅内出血等致命性不良反应[5-7],提示长期应用NOACs所致出血风险是临床需重点关注的问题。
近年来,NOACs在女性血栓栓塞性疾病患者中的应用越来越广泛[8],其诱发的生殖系统异常出血也越来越受到临床重视。2017年3月,美国FDA官方发布警告,NOACs可能会诱发“经期延长”的不良事件(ADE),提示临床需重点关注女性生殖系统异常出血事件[9]。封学伟等[10]经文献调研发现,6 篇关于NOACs诱发女性生殖系统异常出血的观察性研究的结果显示,NOACs致女性生殖系统异常出血的发生率高达15%~70%[11-16];以發表年份排序后发现,上述文献的发表时间均在 2015 年及以后,且均为国外研究。目前,虽然有研究对NOACs诱发威胁生命的大出血事件进行了报道,但多为消化道出血、颅内出血等[5-7],对于女性生殖系统异常出血的研究较少。为此,本研究通过信号检测方法对美国FDA不良事件报告系统(FDA adverse event reporting system,FAERS)数据库中NOACs(如达比加群酯、利伐沙班、阿哌沙班、依度沙班等)致女性生殖系统异常出血事件的信号进行检测,以评估该类药物致女性生殖系统异常出血发生的风险,旨在为其临床用药的安全性提供参考。
1 资料与方法
1.1 数据来源
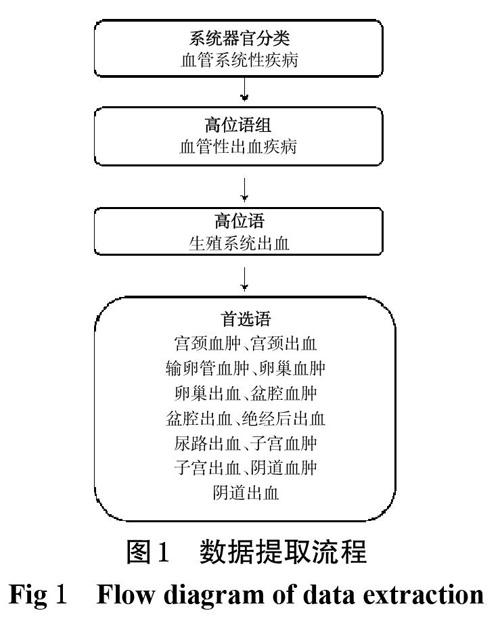
利用OpenFDA平台,收集2004年1月1日-2019年5月31日FAERS数据库中收录的以“达比加群酯”“利伐沙班”“阿哌沙班”“依度沙班”为首要怀疑药物的ADE报告。本研究限定目标药物通用名为“Dabigatran etexilate”“Rivaroxaban”“Apixaban”“Edoxaban”,采用由人用药品注册技术规范国际协调会(ICH)开发的监管活动医学词典(MedDRA)对女性生殖系统异常出血事件进行分类及信息提取,提取信息包括患者年龄、ADE结局等。数据提取流程见图1。
1.2 ADE信号检测方法
采用报告比值比法(ROR)对NOACs诱发女性生殖系统异常出血事件进行信号检测,ROR算法列表见表1(表中,a 表示数据库中某段时间内目标药物的目标 ADE 的报告数,b 为目标药物的其余所有ADE的报告数,c 为数据库中除目标药物外的其余药物的目标ADE的报告数,d 为数据库中除目标药物和目标ADE外的其余报告数)[17]。
2 结果
2.1 基本信息
FAERS数据库中共收录ADE报告10 432 108份,其中以达比加群酯为首要怀疑药物的ADE报告58 886份、利伐沙班125 522份、阿哌沙班68 630份、依度沙班774份,共涉及胃肠道系统、皮肤/皮下系统、肾脏系统、肝脏系统、生殖系统等,4种NOACs的ADE上报情况见图2。涉及女性生殖系统异常出血的ADE报告共2 658份,其中达比加群酯330份(12.41%)、利伐沙班2 049份(77.09%)、阿哌沙班267份(10.05%)、依度沙班12份(0.45%)。
达比加群酯、阿哌沙班、依度沙班诱发女性生殖系统异常出血的患者均以≥75岁为主,分别占37.27%、36.70%、58.33%;利伐沙班以45~64岁为主,占33.04%。患者年龄分布见表2。
美国FDA对出现下列情形之一者界定为严重的不良事件(SAE):住院/住院时间延长、威胁生命、致残、死亡[18]。在4种NOACs致女性生殖系统异常出血的ADE报告中,达比加群酯SAE的发生率96.36%、利伐沙班为84.53%,阿哌沙班为47.19%,依度沙班为58.33%;均以住院/住院时间延长为主,分别占64.78%、90.01%、86.51%、71.43%。SAE发生情况见表3。
2.2 信号检测结果
MedDRA将ADE分为:系统器官分类、高位语组、高位语、首选语等多个层级[19]。本研究以首选语的MedDRA术语进行信号检测。结果,共检测到12个可疑信号,涉及出血部位包括宫颈、输卵管、卵巢、盆腔、子宫、阴道、尿路等。其中,利伐沙班的可疑信号最多,为11个,出血事件主要表现为阴道血肿[ROR=12.07,95%CI(8.51,17.12)]、绝经后出血[ROR=9.89,95%CI(8.31,11.77)]、盆腔血肿[ROR=7.68,95%CI(5.66,10.43)]等。达比加群酯、阿哌沙班、依度沙班分别有可疑信号4、4、2个:阿哌沙班[ROR=5.18,95%CI(1.81,5.85)]、依度沙班[ROR=48.19,95%CI(6.76,343.77)]均以阴道血肿为主;达比加群酯以盆腔血肿[ROR=12.56,95%CI(8.92,17.70)]信号最强,其次为尿路出血[ROR=5.41,95%CI(3.34,8.76)]和盆腔出血[ROR=2.53,95%CI(1.88,3.40)],详见表4(表中,“*”表示可疑信号,“-”表示未检出)。
3 討论
NOACs上市前的相关临床试验并未重点关注女性生殖系统异常出血事件,通过查阅美国FDA发布的药品说明书,发现达比加群酯、利伐沙班、依度沙班均未提及女性生殖系统异常出血的相关ADE,仅有阿哌沙班明确提出“接受本药2.5 mg,bid,po治疗的患者(n=5 924)出现的生殖道血管性异常出血(包括阴道及尿道血肿、出血)的发生率为‘常见(1%~10%)”。一项回顾性研究发现,在15~59岁女性使用抗凝药的过程中,重度异常子宫出血的发生率,从抗凝治疗前的17.8%增加到抗凝后的29.5%[16]。本研究通过检索FAERS数据库,对4种NOCAs(达比加群酯、利伐沙班、依度沙班、阿哌沙班)诱发女性生殖系统异常出血的ADE 进行分析,结果发现,4种药物均出现了女性生殖系统异常出血的相关可疑信号,其中利伐沙班信号最多(11个),其次为阿哌沙班(4个)和达比加群酯(4个),依度沙班(2个)。这提示NOACs存在诱发女性生殖系统异常出血的风险。SAE发生率分别为达比加群酯96.36%、利伐沙班84.53%、阿哌沙班47.19%、依度沙班58.33%;其中“死亡”发生率分别为达比加群酯26.10%、利伐沙班7.74%、阿哌沙班6.35%,依度沙班14.29%。这提示NOACs致女性生殖系统异常出血事件较为严重,且患者预后不良、死亡率较高。Martinelli I等[20]研究显示,60岁以上的女性患者在接受利伐沙班治疗后,其生殖系统异常出血的发生率为29.8%,且有19 例患者出现需要输血治疗的重要出血事件。本研究对出现死亡事件的报告进行逐一查看后发现,死亡者主要为75岁以上老年女性。这提示临床在使用NOACs时应加强对女性患者生殖系统异常出血的监护,特别是年龄在75岁以上的老年患者[14]。
本研究结果还显示,NOACs诱发女性生殖系统异常出血主要涉及的出血部位包括宫颈、输卵管、卵巢、盆腔、子宫、阴道、尿路等。出血风险主要来自于利伐沙班,占报告总数的77.09%,其中有8个信号的ROR值超过2,最大出血风险为阴道血肿,此外还出现了绝经后出血及盆腔血肿等,该结果目前尚未见国内外相关研究报道。此外,值得注意的是,利伐沙班、阿哌沙班、依度沙班均为 Ⅹa因子抑制剂类NOACs,均出现了阴道血肿,笔者推测这可能为Ⅹa因子抑制剂类NOACs共有的ADE。本研究中,达比加群酯诱发女性生殖系统异常出血主要表现为盆腔血肿、尿路出血、盆腔出血。依度沙班由于上市时间较短,自上市以来仅报告12例女性患者出现生殖系统异常出血(2例子宫出血、8例阴道出血、2例阴道血肿),由于新药上市5年内为新发ADE高峰期[17],因此对该药还需持续、重点关注。
本研究的局限性如下:通过ROR法检测出的ADE信号只能表明药物-ADE组合间有统计学关联,而非必然的因果关系;加之目前国内关于NOCAs诱发女性生殖系统异常出血的研究较少,因此本研究所得结论需要更多的临床试验加以验证。
参考文献
[ 1 ] KOTSEVA K,WOOD D,BACKER GD,et al. Cardiovascular prevention guidelines in daily practice:a comparison of EUROASPIRE Ⅰ,Ⅱ,and Ⅲ surveys in eight European countries[J]. Lancet,2009,373(9667):929-940.
[ 2 ] LANE DA,WOOD K. Cardiology patient page.Patient guide for taking the non-vitamin K antagonist oral anticoagulants for atrial fibrillation[J]. Circulation,2015,131(16):e412-e415.
[ 3 ] KIRCHHOF P,BENUSSI S,KOTECHA D,et al. 2016 ESC guidelines for the management of atrial fibrillation developed in collaboration with EACTS[J]. Europace,2016,18(11):1609-1678.
[ 4 ] KEARON C,AKL EA,ORNELAS J,et al. Antithrombotic therapy for VTE disease:chest guideline and expert panel report[J]. Chest,2016,149(2):315-352.
[ 5 ] SCHULMAN S. Advantages and limitations of the new anticoagulants[J]. Intern Med,2014,275(1):1-11.
[ 6 ] FU WB,GUO HY,GUO JP,et al. Relative efficacy and safety of direct oral anticoagulants in patients with atrial fibrillation by net work meta-analysis[J]. Cardiovasc Med:Hagerstown,2014,15(12):873-879.
[ 7 ] TAMAYO S,PEACOCK WF,PATEL M,et al. Characterizing major bleeding in patients with nonvalvular atrial fibrillation:a pharmacovigilance study of 27 467 patients taking rivaroxaban[J]. Clin Cardiol,2015,38(2):63-68.
[ 8 ] TOWFIGHI A,ZHENG L,OVBIAGELE B. Sex-specific trends in midlife coronary heart disease risk and prevalence[J]. Arch Intern Med,2009,169(19):1762-1766.
[ 9 ] FDA. FDA drug safety communication:safety review of post-market reports of serious bleeding events with anticoagulant Pradaxa(dabigatran etexilate mesylate)[EB/OL].[2020-03-01]. https://www.fda.gov/drugs/drug-safety-and- availability.
[10] 封学伟,冯欣,刘小艳,等.新型口服抗凝药预防和治疗静脉血栓栓塞时对异常子宫出血的影响[J].临床药物治疗杂志,2018,16(2):27-30.
[11] DE CREM N,PEERLINCK K,VANASSCHE T,et al. Abnormal uterine bleeding in VTE patients treated with rivaroxaban compared to vitamin K antagonists[J]. Thromb Res,2015,136(4):749-753.
[12] KLINE JA,KAHLER ZP,BEAM DM. Outpatient treatment of low-risk venous thromboembolism with monotherapy oral anticoagulation:patient quality of life outcomes and clinician acceptance[J]. Patient Prefer Adher,2016. DOI:10.2147/PPA.S104446.
[13] BEYER-WESTENDORF J,MICHALSKI F,TITTL L,et al. Management and outcomes of vaginal bleeding and heavy menstrual bleeding in women of reproductive age on direct oral anti-factor Ⅹa inhibitor therapy:a case series[J]. Lancet Haematol,2016,3(10):e480-e488.
[14] FERREIRA M,BARSAM S,PATEL JP,et al. Heavy menstrual bleeding on rivaroxaban[J]. Br J Haematol,2016,173(2):314-315.
[15] BRYK AH,PIROG M,PLENS K,et al. Heavy menstrual bleeding in women treated with rivaroxaban and vitamin K antagonists and the risk of recurrent venous thromboembolism[J]. Vascul Pharmacol,2016. DOI:10.1016/j.vph. 2016.11.003.
[16] MYERS B,WEBSTER A. Heavy menstrual bleeding on rivaroxaban comparison with apixaban[J]. Br J Haematol,2017,176(5):833-835.
[17] BATE A,EVANS SJ. Quantitative signal detection using spontaneous ADR reporting[J]. Pharmacoepidemiol Drug Saf,2009,18(6):427-436.
[18] COLILLA S,TOV EY,ZHANG L,et al. Validation of new signal detection methods for web query log data compared to signal detection algorithms used with FAERS[J]. Drug Saf,2017,40(5);399-408.
[19] TIEU C,BREDER CD. A critical evaluation of safety signal analysis using algorithmic standardised MedDRA queries[J]. Drug Saf,2018,41(12):1375-1385.
[20] MARTINELLI I,LENSING AW,MIDDELDORP S,et al.Recurrent venous thromboembolism and abnormal uterine bleeding with anticoagulant and hormone therapy use[J]. Blood,2016,127(11):1417-1425.
(收稿日期:2020-03-23 修回日期:2020-05-28)
(編辑:陈 宏)

