肝素类药物防治肝硬化静脉血栓栓塞的研究进展
0 引言
传统观点认为肝硬化患者处于低凝状态,出血风险高
.然而,当前的证据提示肝硬化患者凝血系统处于“再平衡”状态,不仅存在出血倾向,而且常伴发多种静脉血栓栓塞性疾病(venous thromboembolism,VTE)
.肝硬化患者中,最常发生VTE的部位是门静脉
.肝硬化患者发生门静脉血栓(portal vein thrombosis,PVT)的风险是普通人群的7倍
,其发病率为3%-17%,患病率为5%-26%
.PVT可增加肝硬化患者消化道出血、腹水、急性肾损伤及肝移植术后死亡的风险
.此外,肝硬化患者发生其他部位VTE的风险是普通人群的1.7倍
,主要包括深静脉血栓(deep vein thrombosis,DVT)和肺栓塞(pulmonary embolism,PE).肝硬化患者DVT或PE发病率为0.2%-6.3%
,患病率为0.4%-4.7%
.肝硬化合并DVT患者30 d死亡率为7%,为非肝硬化患者的2.17倍;肝硬化合并PE患者30 d死亡率为35%,为非肝硬化患者的1.3倍
.
抗凝是预防及治疗肝硬化VTE的重要手段之一,可显著减少肝硬化患者血栓发生率、增加血栓再通率,甚至可以降低肝脏失代偿率并提高总体生存率
.肝素类药物是目前临床最常用的抗凝药物
,主要包括普通肝素、低分子肝素(依诺肝素、那曲肝素、达肝素、达那肝素等)以及合成肝素(磺达肝癸钠等)
.2020年美国重症医学会指南
推荐普通肝素及低分子肝素可用于预防及治疗肝硬化患者VTE,但该推荐强度弱、证据质量低.更值得一提的是,肝硬化患者常合并食管胃底静脉曲张及血小板减少症,故在临床实践中需考虑肝素类药物在肝硬化患者中应用的安全性
.目前,肝硬化患者应用肝素类药物的适应症、药物种类、药物剂量及监测等问题尚无定论.为此,本文通过回顾国内外相关文献,总结肝素类药物防治肝硬化VTE的研究进展,为临床合理用药提供参考.
1 肝素类药物的种类与特点
普通肝素是一种硫酸化的葡萄糖胺聚糖混合物,平均分子量为12 kDa
.其通过与抗凝血酶Ⅲ(AT-Ⅲ)特异性结合,加速灭活血浆中凝血因子Ⅱa、Ⅸa、Ⅹa、Ⅺa和Ⅻa
,进而发挥抗凝作用.普通肝素的生物利用度约为30%,药物半衰期为30 min-60 min
.出血是普通肝素主要的不良反应,可表现为各种黏膜出血、关节腔积血和伤口出血等.普通肝素也可导致免疫诱导性血小板减少症,发生率达5%,多发生在给药后7 d -10 d.
低分子肝素是从普通肝素中分离或由普通肝素降解后得到的短链制剂,一般分子量低于7 kDa
.由于分子链较短,不能与AT-Ⅲ和凝血因子Ⅱa同时结合形成复合物,故主要对凝血因子Ⅹa发挥作用.生物利用度约为90%.药物半衰期为119 min-180 min,约为普通肝素的2-4倍.常见的不良反应有出血、免疫诱导性血小板减少症等.临床常用的低分子肝素包括依诺肝素、那曲肝素、达肝素、达那肝素等.
广东语文高职高考说明文阅读主要考查的是考生信息的收集、概括和归纳的能力,难度其实不大,如下一些解题方法可以借鉴。
最近,我国抗凝药物指南推荐低分子肝素可作为预防肝硬化患者DVT/PE的首选药物
,但证据尚不充分.一项回顾性研究发现
,与未接受低分子肝素预防的患者相比,接受低分子肝素预防的患者DVT/PE发生率更低(0.63%
1.38%,
=0.530),出血发生率更高(3.18%
1.38%,
=0.380),但两组间无显著差异(表1).荟萃分析结果显示
,接受与未接受肝素类药物预防的肝硬化患者之间DVT/PE发生率也无显著性差异(OR=1.65,95%CI:0.36-7.54,
>0.05).因此,肝素类药物预防肝硬化DVT/PE的确切疗效仍有待更为严格的随机对照试验加以验证.
磺达肝癸钠是一种以AT-Ⅲ-肝素结合位点结构为基础人工合成的戊多糖.仅对凝血因子Ⅹa发挥抑制作用.与普通肝素和低分子肝素相比,该药具有更高的生物利用度(100%)及更长的药物半衰期(17 h以上),且基本上不会导致出血及免疫诱导性血小板减少症的不良反应
.
2 肝素类药物的剂量与监测
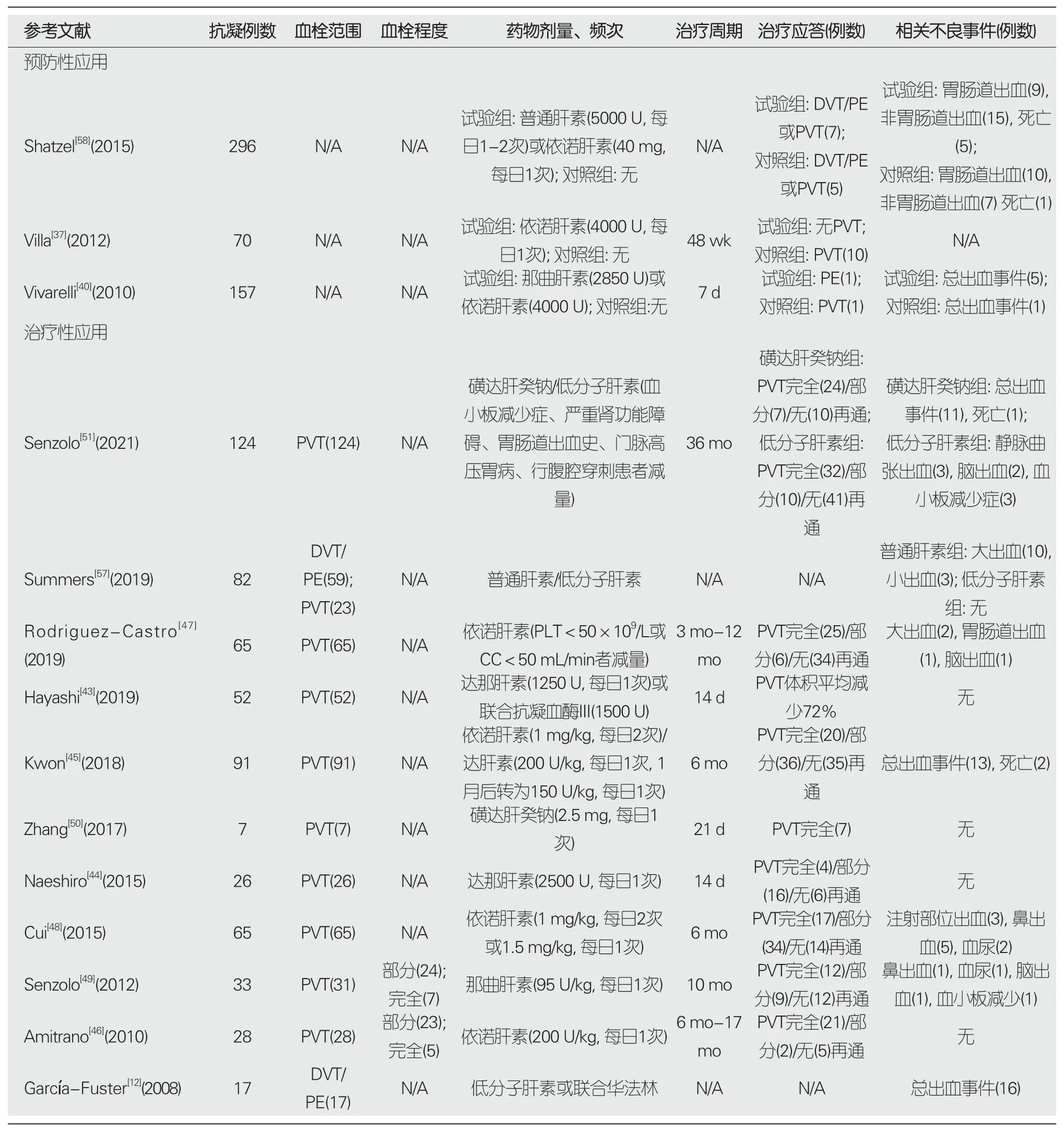
2020年,我国《肝硬化门静脉血栓管理专家共识》建议
,肝硬化PVT抗凝治疗的主要适应证为急性症状性PVT、等待肝移植、合并肠系膜静脉血栓.主要禁忌证为近期出血史、严重的食管胃静脉曲张、严重的血小板减少症.近年的研究发现,肝素类药物治疗肝硬化PVT具有重要作用,但易引起出血事件及血小板减少症等不良反应
(表1).肝硬化PVT患者经达那肝素治疗2 wk后
,PVT体积可平均缩小72%-77%,完全再通率为15%,部分再通率为62%,未发生大出血、血小板减少、肝损伤等不良反应.肝硬化PVT患者经达肝素或依诺肝素抗凝治疗6 mo后
,治疗应答率(包括完全再通及部分再通)为61%-78.5%,无应答率为16.7%-30.8%,PVT进展率为4.4%,总体出血率为4%-23.5%
,致死性出血率为2.1%
.肝硬化PVT患者经那曲肝素治疗5.5 mo后
,治疗应答率(包括完全再通及部分再通)为63%,总体出血率为8.5%.肝硬化PVT患者经磺达肝癸钠治疗21 d后
,完全再通率为100%,未发生出血或血小板减少等不良反应,但该研究样本量小(仅7例患者),且治疗时间较短(仅21 d).最近,一项回顾性研究比较了低分子肝素与磺达肝癸钠治疗肝硬化PVT患者36 mo后的疗效
,接受磺达肝癸钠治疗患者的治疗应答率(77%
51%,
=0.001)及出血事件发生率(27%
13%,
=0.06)均高于接受低分子肝素治疗患者.荟萃分析结果显示
,低分子肝素及磺达肝癸钠治疗肝硬化PVT后,治疗应答率分别为71.2%及71.6%,完全再通率分别为41.0%及43.0%,总体出血事件发生率分别为6.5%及15.1%.尽管磺达肝癸钠给药剂量固定
,且无血小板减少等不良反应
,但该药在肝硬化患者中似乎有着较高的出血率.因此,低分子肝素被推荐作为治疗肝硬化PVT的首选肝素类药物
,疗程为6 mo或直至门静脉再通
.
3 肝素类药物在肝硬化VTE中的预防价值
低分子肝素可有效安全地预防肝硬化患者发生PVT(表1).一项随机对照试验结果显示
,48 wk及96 wk时,接受依诺肝素预防的患者无一例发生PVT,未接受依诺肝素的患者PVT发生率分别为16.6%及27.7%;随访结束时,接受依诺肝素预防的患者PVT发生率显著低于未接受依诺肝素的患者(8.8%
27.7%,
=0.006);两组间出血事件发生率无显著性差异(5.8%
2.7%,
=0.521).该研究也显示
,接受依诺肝素预防的患者肝脏失代偿率(38.2%
83.0%,
<0.0001)及死亡率(23.5%
36.1%,
=0.251)均更低.基于此,2016年意大利肝病学会和意大利医学学会有关肝硬化止血平衡的共识建议将低分子肝素用于预防肝硬化PVT
.
在紧张的复习阶段,大家肯定遇到了各种顺利或是不顺利的事情。在这里,我想和大家分享一下我酸甜苦辣的期末复习之旅。
4 肝素类药物在肝硬化VTE中的治疗价值
通常情况下,普通肝素预防剂量为首剂皮下注射5000 U,之后每12 h注射5000 U
,治疗剂量为首剂静脉注射5000 U,之后每1 h持续注射18 U/kg
,用药4 h后应监测抗Ⅹa因子活性,参考范围为0.35 U/mL-0.7 U/mL
;低分子肝素预防剂量为皮下注射4000 U-5000 U,每日1次
.治疗剂量为皮下注射100 U/kg,每日2次
,用药4 h后同样应监测抗Ⅹa因子活性,参考范围为0.6 U/mL-1.3 U/mL
;磺达肝癸钠治疗剂量为皮下注射2.5 mg,每日1次
.然而,目前研究不建议肝硬化患者根据抗Ⅹa因子活性调整剂量
,可使用总体止血试验作为补充监测
.Bechmann等
发现,接受标准剂量依诺肝素的肝硬化患者未能达到推荐的预防性及治疗性抗Ⅹa因子活性.该研究纳入了84例肝硬化患者,分别给予预防剂量(4000 U,每日1次)及治疗剂量(100 U/kg,每日1次)依诺肝素,给药4 h后,接受预防及治疗剂量的肝硬化患者的平均抗Ⅹa因子活性分别为(0.169±0.122) U/mL及(0.432±0.173) U/mL,均低于参考范围.此外,依诺肝素给药后发生出血的患者比未发生出血的患者抗Ⅹa因子活性更低[(0.088±0.038) U/mL
(0.174±0.016 U/mL)].因此,肝硬化患者根据抗Ⅹa因子活性调整剂量并不可靠.相比于抗Ⅹa因子活性监测,总体止血试验,如凝血酶生成试验,可能会更精确、更高效地反映肝素类药物在肝硬化患者中的抗凝活性
.Potze等
留取了30例肝硬化患者及30例健康对照者的血浆样本,分别添加0.3 U/mL普通肝素、0.2 U/mL依诺肝素及0.5 μg/mL磺达肝癸钠.结果显示,肝硬化患者凝血酶生成曲线下面积的下降幅度较健康对照者更大,这说明肝硬化患者对普通肝素及低分子肝素的反应增加
,抗凝效果增强,建议减量使用
;而磺达肝癸钠在肝硬化患者血浆中的反应降低,抗凝效果减弱,建议增加剂量
.然而,这一结论并未考虑到肝硬化患者体内血小板对凝血过程的影响.尚不清楚调整剂量后的肝素类药物是否能在肝硬化患者体内最大限度地发挥药物疗效以及减少不良反应.总之,目前仍需更多的临床研究探讨凝血酶生成试验以及其他监测方法对指导肝素类药物剂量调整的临床实用价值.
(3)《老甲》简9:“竺(孰)能浊以静者,将徐清。”《老甲》简10:“竺(孰)能安以动者。”(竺,端母觉部;孰,禅母觉部。)
两项回顾性研究探讨了普通肝素及低分子肝素治疗肝硬化DVT/PE患者的安全性(表1);2008年,García-Fuster等发现
,接受低分子肝素治疗的患者有着较高的出血率.该研究纳入了1992-2007住院的17例肝硬化DVT/PE患者.其中,11例接受低分子肝素治疗,6例接受低分子肝素序贯华法林治疗.治疗期间,16例发生出血,6例需要输注血液制品,14例因严重的出血事件不得不提前中止应用抗凝药物,出血率达83%.然而,2020年,Summers等发现
,相比于普通肝素,接受低分子肝素治疗的肝硬化DVT/PE及PVT患者有着较低的出血率.该研究纳入了59例肝硬化DVT/PE患者及23例PVT患者,其中接受普通肝素治疗52例,大出血率为19.2%,小出血率为5.8%;低分子肝素治疗30例,大、小出血率均为0%.因此,普通肝素及低分子肝素在肝硬化DVT/PE患者中的安全性仍存在争议.
5 结论
肝硬化患者使用肝素类药物时,不推荐通过监测抗Ⅹa因子活性调整用药剂量;相比之下,总体止血试验可能会更好地评估肝素类药物的抗凝效果及安全性.肝素类药物可有效防治肝硬化PVT,但对DVT/PE的防治效果尚有待进一步验证.
1 Tripodi A,Mannucci PM.The coagulopathy of chronic liver disease.
2011;365:147-156 [PMID:21751907 DOI:10.1056/NEJMra1011170]
2 He Y,Yuan S,Guo X,Yi F,Xu X,An Y,Xu S,Ageno W,Qi X.Association of thromboelastography profile with severity of liver cirrhosis and portal venous system thrombosis.
2021;21:253 [PMID:34098892 DOI:10.1186/s12876-021-01832-3]
3 Zhang X,Qi X,De Stefano V,Zhu Z,Qiao R,Guo X.Impact of liver cirrhosis on the outcomes of patients with venous thromboembolism:A case-control study.
2017;2:26 [DOI:10.21037/amj.2017.02.11]
4 Amitrano L,Guardascione MA,Brancaccio V,Balzano A.Coagulation disorders in liver disease.
2002;22:83-96 [PMID:11928081 DOI:10.1055/s-2002-23205]
5 Chun HS,Choe AR,Lee M,Cho Y,Kim HY,Yoo K,Kim TH.Treatment of direct oral anticoagulants in patients with liver cirrhosis and portal vein thrombosis.
2021;27:535-552 [PMID:34130370 DOI:10.3350/cmh.2021.0109]
6 祁兴顺,杨玲.肝硬化门静脉血栓管理专家共识(2020年,上海).临床肝胆病杂志 2020;36:2667-2674 [DOI:10.3969/j.issn.1001-5256]
7 Qi X,Su C,Ren W,Yang M,Jia J,Dai J,Xu W,Guo X.Association between portal vein thrombosis and risk of bleeding in liver cirrhosis:A systematic review of the literature.
2015;39:683-691 [PMID:25956490 DOI:10.1016/j.clinre.2015.02.012]
8 Ghabril M,Agarwal S,Lacerda M,Chalasani N,Kwo P,Tector AJ.Portal vein thrombosis is a risk factor for poor early outcomes after liver transplantation:Analysis of risk factors and outcomes for portal vein thrombosis in waitlisted patients.
2016;100:126-133 [PMID:26050013 DOI:10.1097/tp.0000000000000785]
9 Ambrosino P,Tarantino L,Di Minno G,Paternoster M,Graziano V,Petitto M,Nasto A,Di Minno MN.The risk of venous thromboembolism in patients with cirrhosis.A systematic review and meta-analysis.
2017;117:139-148 [PMID:27761574 DOI:10.1160/th16-06-0450]
10 Qi X,Ren W,Guo X,Fan D.Epidemiology of venous thromboembolism in patients with liver diseases:A systematic review and meta-analysis.
2015;10:205-217 [PMID:25472621 DOI:10.1007/s11739-014-1163-7]
11 Zhang X,Qi X,De Stefano V,Hou F,Ning Z,Zhao J,Peng Y,Li J,Deng H,Li H,Guo X.Epidemiology,risk factors,and in-hospital mortality of venous thromboembolism in liver cirrhosis:A singlecenter retrospective observational study.
2016;22:969-976 [PMID:27009380 DOI:10.12659/msm.896153]
12 García-Fuster MJ,Abdilla N,Fabiá MJ,Fernández C,Oliver V,Forner M J.Venous thromboembolism and liver cirrhosis.
2008;100:259-262 [PMID:18662076 DOI:10.4321/s1130-01082008000500002]
13 Søgaard KK,Horváth-Puhó E,Montomoli J,Vilstrup H,Sørensen HT.Cirrhosis is associated with an increased 30-day mortality after venous thromboembolism.
2015;6:e97 [PMID:26133110 DOI:10.1038/ctg.2015.27]
14 Qi X,Mancuso A.Venous thromboembolism in liver cirrhosis:An emerging issue.
2017;6 [DOI:10.5772/67707]
15 Qi X,De Stefano V,Li H,Dai J,Guo X,Fan D.Anticoagulation for the treatment of portal vein thrombosis in liver cirrhosis:A systematic review and meta-analysis of observational studies.
2015;26:23-29 [PMID:25566699 DOI:10.1016/j.ejim.2014.12.002]
16 Qi X,Han G,Fan D.Management of portal vein thrombosis in liver cirrhosis.
2014;11:435-446 [PMID:24686266 DOI:10.1038/nrgastro.2014.36]
17 Loffredo L,Pastori D,Farcomeni A,Violi F.Effects of anticoagulants in patients with cirrhosis and portal vein thrombosis:A systematic review and meta-analysis.
2017;153:480-487 [PMID:28479379 DOI:10.1053/j.gastro.2017.04.042]
18 Nanchal R,Subramanian R,Karvellas CJ,Hollenberg SM,Peppard WJ,Singbartl K,Truwit J,Al-Khafaji AH,Killian AJ,Alquraini M,Alshammari K,Alshamsi F,Belley-Cote E,Cartin-Ceba R,Dionne JC,Galusca DM,Huang DT,Hyzy RC,Junek M,Kandiah P,Kumar G,Morgan RL,Morris PE,Olson JC,Sieracki R,Steadman R,Taylor B,Alhazzani W.Guidelines for the management of adult acute and acute-on-chronic liver failure in the ICU:Cardiovascular,endocrine,hematologic,pulmonary,and renal considerations.
2020;48:e173-e191 [PMID:32058387 DOI:10.1097/ccm.0000000000004192]
19 Onishi A,St Ange K,Dordick JS,Linhardt RJ.Heparin and anticoagulation.
2016;21:1372-1392 [PMID:27100512 DOI:10.2741/4462]
20 Wang L,Xu X,Hou Y,Shao X,Guo X,Qi X.Acute mesenteric vein thrombosis after endoscopic injection sclerotherapy for esophageal varices in a patient with liver cirrhosis.
2019;13:118-121 [PMID:31080203 DOI:10.5582/ddt.2019.01014]
21 Xu X,Guo X,Wang R,Wang L,Li Q,Yi F,Li H,Qi X.Lowmolecular-weight heparin followed by rivaroxaban for acute occlusive portomesenteric vein thrombosis in a cirrhotic patient treated with multiple endoscopic variceal procedures.
2020;19:573-577 [PMID:31521463 DOI:10.1016/j.aohep.2019.08.002]
22 季晖.药理学.南京东南大学出版社,2019
23 Baglin T,Barrowcliffe TW,Cohen A,Greaves M;British Committee for Standards in Haematology.Guidelines on the use and monitoring of heparin.
2006;133:19-34 [PMID:16512825 DOI:10.1111/j.1365-2141.2005.05953.x]
24 罗振,张天民.低分子肝素的分子量与抗血栓作用的关系.中国医药工业杂志 1991;3:140-141 [DOI:10.16522/j.cnki.cjph.1991.03.018]
25 Ashish K,Bandyopadhyay D,Hajra A,Ghosh RK.Possible use of fondaparinux in heparin-induced thrombocytopenia.
2018;256:3 [PMID:29454410 DOI:10.1016/j.ijcard.2017.12.029]
26 Carson JL.Subcutaneous unfractionated heparin vs lowmolecular-weight heparin for acute thromboembolic disease:issues of efficacy and cost.
2006;296:991-993 [PMID:16926359 DOI:10.1001/jama.296.8.991]
27 《中国血栓性疾病防治指南》专家委员会.中国血栓性疾病防治指南.中华医学杂志 2018;98:2861-2888 [DOI:10.3760/cma.j.issn.0376-2491.2018.36.002]
28 吴雯玥,孔德润.门静脉血栓诊治的一些新认识.世界华人消化杂志 2021;4:165-173 [DOI:10.11569/wcjd.v29.i4.165]
29 邸平,李绵洋.抗Ⅹa活性检测在抗凝治疗中的临床应用现状与前景.协和医学杂志 2021;12:456-459 [DOI:10.12290/xhyxzz.2021-0424]
30 Bechmann LP,Sichau M,Wichert M,Gerken G,Kröger K,Hilgard P.Low-molecular-weight heparin in patients with advanced cirrhosis.
2011;31:75-82 [PMID:20958919 DOI:10.1111/j.1478-3231.2010.02358.x]
31 Potze W,Arshad F,Adelmeijer J,Blokzijl H,van den Berg AP,Porte RJ,Lisman T.Routine coagulation assays underestimate levels of antithrombin-dependent drugs but not of direct anticoagulant drugs in plasma from patients with cirrhosis.
2013;163:666-673 [PMID:24219333 DOI:10.1111/bjh.12593]
32 Franz ND,Brancaccio A,Robinson AC,Regal RE.Cirrhosis,Thrombosis,Finding FaXts about doses:Dosing of unfractionated heparin for venous thromboembolism in cirrhosis.
2020;54:450-456 [PMID:31766856 DOI:10.1177/1060028019890028]
33 Altman R,Scazziota AS,Pons S,Herrera L,Keller AG,Assefi AR,Di Girolamo G.Effects of enoxaparin preparations on thrombin generation and their correlation with their anti-FXa activity.
2011;27:1-9 [PMID:21083516 DOI:10.1185/03007995.2010.535512]
34 Potze W,Arshad F,Adelmeijer J,Blokzijl H,van den Berg AP,Meijers JC,Porte RJ,Lisman T.Differential in vitro inhibition of thrombin generation by anticoagulant drugs in plasma from patients with cirrhosis.
2014;9:e88390 [PMID:24505487 DOI:10.1371/journal.pone.0088390]
35 Tripodi A,Primignani M,Braham S,Chantarangkul V,Clerici M,Moia M,Peyvandi F.Coagulation parameters in patients with cirrhosis and portal vein thrombosis treated sequentially with low molecular weight heparin and vitamin K antagonists.
2016;48:1208-1213 [PMID:27470055 DOI:10.1016/j.dld.2016.06.027]
36 Thomas O,Lybeck E,Strandberg K,Tynngård N,Schött U.Monitoring low molecular weight heparins at therapeutic levels:dose-responses of,and correlations and differences between aPTT,anti-factor Xa and thrombin generation assays.
2015;10:e0116835 [PMID:25625201 DOI:10.1371/journal.pone.0116835]
37 Villa E,Cammà C,Marietta M,Luongo M,Critelli R,Colopi S,Tata C,Zecchini R,Gitto S,Petta S,Lei B,Bernabucci V,Vukotic R,De Maria N,Schepis F,Karampatou A,Caporali C,Simoni L,Del Buono M,Zambotto B,Turola E,Fornaciari G,Schianchi S,Ferrari A,Valla D.Enoxaparin prevents portal vein thrombosis and liver decompensation in patients with advanced cirrhosis.
2012;143:1253-1260 [PMID:22819864 DOI:10.1053/j.gastro.2012.07.018]
38 Italian Association for the Study of Liver Diseases (AISF) and the Italian Society of Internal Medicine (SIMI).Hemostatic balance in patients with liver cirrhosis:Report of a consensus conference.
2016;48:455-467 [PMID:27012444 DOI:10.1016/j.dld.2016.02.008]
39 王乔宇,武明芬,柳鑫,王晓岩,陈耀龙,赵志刚.2021中国静脉血栓栓塞症防治抗凝药物的选用与药学监护指南.中国临床药理学杂志 2021;37:2999-3016 [DOI:10.13699/j.cnki.1001-6821.2021.21.032]
40 Vivarelli M,Zanello M,Zanfi C,Cucchetti A,Ravaioli M,Del Gaudio M,Cescon M,Lauro A,Montanari E,Grazi GL,Pinna AD.Prophylaxis for venous thromboembolism after resection of hepatocellular carcinoma on cirrhosis:is it necessary?
2010;16:2146-2150 [PMID:20440855 DOI:10.3748/wjg.v16.i17.2146]
41 Gómez Cuervo C,Bisbal Pardo O,Pérez-Jacoiste Asín MA.Efficacy and safety of the use of heparin as thromboprophylaxis in patients with liver cirrhosis:A systematic review and metaanalysis.
2013;132:414-419 [PMID:23993900 DOI:10.1016/j.thromres.2013.08.001]
42 Lee GY,Hua N,Yu M,Hsieh TC.Unusual cause for abdominal pain:Portal vein thrombosis.
2020;115:S1824 [DOI:10.14309/01.ajg.0000716164.87480.7a]
43 Hayashi T,Takatori H,Horii R,Nio K,Terashima T,Iida N,Kitahara M,Shimakami T,Arai K,Kitamura K,Kawaguchi K,Yamashita T,Sakai Y,Yamashita T,Mizukoshi E,Honda M,Toyama T,Okumura K,Kozaka K,Kaneko S.Danaparoid sodium-based anticoagulation therapy for portal vein thrombosis in cirrhosis patients.
2019;19:217 [PMID:31842768 DOI:10.1186/s12876-019-1140-8]
44 Naeshiro N,Aikata H,Hyogo H,Kan H,Fujino H,Kobayashi T,Fukuhara T,Honda Y,Nakahara T,Ohno A,Miyaki D,Murakami E,Kawaoka T,Tsuge M,Hiraga N,Hiramatsu A,Imamura M,Kawakami Y,Ochi H,Chayama K.Efficacy and safety of the anticoagulant drug,danaparoid sodium,in the treatment of portal vein thrombosis in patients with liver cirrhosis.
2015;45:656-662 [PMID:25088236 DOI:10.1111/hepr.12400]
45 Kwon J,Koh Y,Yu SJ,Yoon JH.Low-molecular-weight heparin treatment for portal vein thrombosis in liver cirrhosis:Efficacy and the risk of hemorrhagic complications.
2018;163:71-76 [PMID:29407630 DOI:10.1016/j.thromres.2018.01.032]
46 Amitrano L,Guardascione MA,Menchise A,Martino R,Scaglione M,Giovine S,Romano L,Balzano A.Safety and efficacy of anticoagulation therapy with low molecular weight heparin for portal vein thrombosis in patients with liver cirrhosis.
2010;44:448-451 [PMID:19730112 DOI:10.1097/MCG.0b013e3181b3ab44]
47 Rodriguez-Castro KI,Vitale A,Fadin M,Shalaby S,Zerbinati P,Sartori MT,Landi S,Pettinari I,Piscaglia F,Han G,Burra P,Simioni P,Senzolo M.A prediction model for successful anticoagulation in cirrhotic portal vein thrombosis.
2019;31:34-42 [PMID:30188408 DOI:10.1097/meg.0000000000001237]
48 Cui SB,Shu RH,Yan SP,Wu H,Chen Y,Wang L,Zhu Q.Efficacy and safety of anticoagulation therapy with different doses of enoxaparin for portal vein thrombosis in cirrhotic patients with hepatitis B.
2015;27:914-919 [PMID:25856686 DOI:10.1097/meg.0000000000000351]
49 Senzolo M,M Sartori T,Rossetto V,Burra P,Cillo U,Boccagni P,Gasparini D,Miotto D,Simioni P,Tsochatzis E,A Burroughs K.Prospective evaluation of anticoagulation and transjugular intrahepatic portosystemic shunt for the management of portal vein thrombosis in cirrhosis.
2012;32:919-927 [PMID:22435854 DOI:10.1111/j.1478-3231.2012.02785.x]
50 Zhang ZH,Zhang JW,He P,Zhou Y,Sun CY.Fondaparinux is effective for acute portal vein thrombosis in decompensated cirrhotic patients.
2017;96:e8256 [PMID:29049216 DOI:10.1097/MD.0000000000008256]
51 Senzolo M,Piano S,Shalaby S,Tonon M,Tonello S,Zanetto A,Sacerdoti D,Simioni P,Bombonato G,Burra P,Angeli P.Comparison of fondaparinux and low-molecular-weight heparin in the treatment of portal vein thrombosis in cirrhosis.
2021;134:1278-1285.e2 [PMID:34197784 DOI:10.1016/j.amjmed.2021.05.013]
52 Wang L,Guo X,Xu X,De Stefano V,Plessier A,Noronha Ferreira C,Qi X.Anticoagulation favors thrombus recanalization and survival in patients with liver cirrhosis and portal vein thrombosis:
of a meta-analysis.
2021;38:495-520 [PMID:33155180 DOI:10.1007/s12325-020-01550-4]
53 Bauer KA,Hawkins DW,Peters PC,Petitou M,Herbert JM,van Boeckel CA,Meuleman DG.Fondaparinux,a synthetic pentasaccharide:The first in a new class of antithrombotic agents -the selective factor Xa inhibitors.
2002;20:37-52 [PMID:12070533 DOI:10.1111/j.1527-3466.2002.tb00081.x]
54 Schindewolf M,Steindl J,Beyer-Westendorf J,Schellong S,Dohmen PM,Brachmann J,Madlener K,Pötzsch B,Klamroth R,Hankowitz J,Banik N,Eberle S,Müller MM,Kropff S,Lindhoff-Last E.Use of fondaparinux off-label or approved anticoagulants for management of heparin-induced thrombocytopenia.
2017;70:2636-2648 [PMID:29169470 DOI:10.1016/j.jacc.2017.09.1099]
55 Northup PG,Garcia-Pagan JC,Garcia-Tsao G,Intagliata NM,Superina RA,Roberts LN,Lisman T,Valla DC.Vascular liver disorders,portal vein thrombosis,and procedural bleeding in patients with liver disease:2020 practice guidance by the American Association for the Study of Liver Diseases.
2021;73:366-413 [PMID:33219529 DOI:10.1002/hep.31646]
56 de Franchis R,Bosch J,Garcia-Tsao G,Reiberger T,Ripoll C;Baveno VII Faculty.Baveno VII -Renewing consensus in portal hypertension.
2022;76:959-974 [PMID:35120736 DOI:10.1016/j.jhep.2021.12.022]
57 Summers KL,Davis KA,Nisly SA.Bleeding risk of therapeutic unfractionated heparin and low molecular weight heparin in patients with cirrhosis.
2020;40:191-196 [PMID:31755014 DOI:10.1007/s40261-019-00875-5]
58 Shatzel J,Dulai PS,Harbin D,Cheung H,Reid TN,Kim J,James SL,Khine H,Batman S,Whyman J,Dickson RC,Ornstein DL.Safety and efficacy of pharmacological thromboprophylaxis for hospitalized patients with cirrhosis:A single-center retrospective cohort study.
2015;13:1245-1253 [PMID:25955079 DOI:10.1111/jth.13000]