Meta-analysis of influencing factors associating with treatment outcome of multidrug resistant tuberculosis
LUO Qie-ning, OUYANG Fan-xian, LIANG Cui-dan, WANG Wei-tong, YU Huang
1.International School of Public Health and One Health, Hainan Medical University, HaiKou 571199,China
2.Department of Nosocomial Infection Management and Preventive Medicine of Second Clinical College of Hainan Medical University, HaiKou 570311,China
3.Preventive medicine of Second Clinical College of Hainan Medical University, HaiKou 570311,China
Keywords:
ABSTRACT Objective: To systematically review the influencing factors of the treatment outcome of multidrug-resistant pulmonary tuberculosis and provide reference for the prevention and treatment of multidrug-resistant pulmonary tuberculosis.Method: Case control studies on the factors influencing the treatment outcome of multidrug-resistant pulmonary tuberculosis in Chinese databases (CNKI, VIP, Wanfang, Sinomed) and English databases (Pubmed,Web of science, Medline, Embase, Scopus) were searched and collected by computer.The search period was from the establishment of the database to January 2023.After screening and quality evaluation, RevMan5.4 was used for meta-analysis.Result: Totally 18 articles were ultimately included, with a sample size of 7 328 people.The results showed that retreatment,complications, adverse reactions, and gender were related to the treatment outcome of multidrug-resistant pulmonary tuberculosis.The OR values and 95% CI of each factor were 0.22 (0.17-0.29), 0.38 (0.32-0.46), 0.27 (0.17-0.44), and 0.43 (0.33-0.56), respectively.Conclusion: Complications, retreatment, adverse reactions, and male gender are effective risk factors for the treatment outcome of multidrug-resistant pulmonary tuberculosis.In clinical practice, more targeted measures are needed for different types of patients.Due to the limitations of the number of studies, the above conclusions require more research to support them.
1.Introduction
Tuberculosis is a chronic infectious disease caused by mycobacterium tuberculosis infection, which has already become a global public health problem.According to the World Health Organization (WHO) report on tuberculosis, in 2021, it is estimated that 10.6 million new tuberculosis patients will be added globally.Among the 30 countries with high burden of tuberculosis, China ranks third, with 780 000 new cases of tuberculosis and a incidence rate of about 55/100 000, making it the third largest country with high burden of tuberculosis[1,2].Multidrug resistant tuberculosis(MDR-TB) is caused by infection with Mycobacterium tuberculosis,which is at least resistant to isoniazid and rifampicin, two firstline antituberculosis drugs.Extensively drug-resistant tuberculosis(XDR-TB) is characterized by a wider drug resistance spectrum of Mycobacterium tuberculosis, which is resistant to a variety of first-line and second-line drugs.Multidrug resistant tuberculosis mostly occurs in the lungs.It is characterized by strong infectivity,long treatment time, difficult treatment, poor treatment effect,high treatment cost and low cure rate.The mortality rate is also significantly higher than that of non drug resistant tuberculosis[3].According to WHO, in 2021, about 450 000 new cases of pulmonary tuberculosis will develop into rifampicin resistant tuberculosis (RRTB).In 2021, the proportion of new MDR-TB/RR-TB in China will be about 3.4%, of which the treatment coverage rate will be 67%, higher than the global level, but the treatment efficiency will be only 53%, lower than the global level[4].Multidrug resistant pulmonary tuberculosis (MDR-PTB) is difficult to manage, and infected individuals are the main source of infection, bringing huge economic burden to society and families, and seriously affecting the quality of life of patients.Therefore, it is necessary to intervene in patients and potential risk groups to reduce social risks.Due to the current lack of rapid screening methods and specific treatment methods for MDR-PTB, it is particularly important to optimize existing patient management and treatment measures, as well as evaluate their effectiveness.The former focuses on hygiene, health,and disease prevention education for patients and their surrounding potential risk populations, while the latter focuses on identifying factors that affect the efficacy.There are still shortcomings in the treatment effectiveness and management of MDR-PTB patients in China, it is necessary to strengthen and standardize patient management while analyzing and summarizing the relevant factors that affect the efficacy of MDR-PTB, in order to provide clinical reference and improve its efficacy.By integrating literature on factors influencing the efficacy of MDR-PTB both domestically and internationally through systematic assessment and meta-analysis, the best evidence is provided to improve the efficacy of MDR-PTB.
2.Materials and Methods
2.1 Search strategy
Retrieve research on the influencing factors of MDR-PTB efficacy from Chinese databases such as CNKI, VIP, Wanfang, Sinomed,and English databases such as PubMed, Medline, Embase, Web of science, and Scopus.The Chinese search terms include “multidrugresistant tuberculosis”, “efficacy OR treatment effect OR outcome”,“analysis of OR factors”, and the English search terms “multidrugresistant tuberculosis”, “MDR-PTB”, “treatment outcome” The search period for ‘predictor OR factor’ is from the establishment of the database to January 2023.
2.2 Selection criteria
Inclusion criteria: (1) Independent published case control studies about influencing factors of MDR-PTB efficacy(2) The efficacy is defined according to the WHO standards, and the treatment plan is based on the multidrug-resistant tuberculosis treatment specifications, which can be adjusted according to the specific situation of patients, such as the type of drug resistance,The total duration is 18 to 24 months (3) All multidrug-resistant tuberculosis patients need to be confirmed by drug sensitivity test (4) Each literature must have the OR value and its 95%CIand data of each grouping, such as the number of successful and failed treatment groups and the total number of people in the group (5) If the same research group publishes more than two related literature, Select only the most recent research literature with a large sample (6) Trreatment outcome : MDR-PTB patient treatment outcome, including treatment effective (completion and cure) and treatment ineffective (failure,death, and loss).
Exclusion criteria: (1) Repeated publications, review literature, (2)Not human studies, extrapulmonary tuberculosis studies, (3) Failure to conduct multivariate analysis, inability to calculate OR values and 95%CI, and failure to provide specific data for each group of literature.
2.3 Quality assessment and data extraction
Import the relevant literature into EndNote X9, and two researchers independently screen literature according to the inclusion and exclusion criteria and cross-check it.If the results are different, a third researcher discusses and confirms them.The initial screening is done by reading the abstracts, and the full-text reading.Extract the basic information of the re-screened literature: (1) author,the publication year, region of the research institution (2) basic characteristics of the research subjects, such as sample size, average age or median age (3) research factors and specific data, such as the specific distribution of samples in the treatment effect grouping, OR value, and 95% confidence interval.
2.4 Quality assessment
The assessment of literature was based on the Newcastle-Ottawa Scale (NOS) (case-control study), which included three sections including population selection, comparability, and exposure, with a total of eight items.The maximum score was 9, and literature with a score of 5 or above was considered high-quality and included in the final meta-analysis.
2.5 Statistical analysis
Using Revman5.4 software for meta-analysis, collecting the required data and establish a database, use Mantel-Haenszel statistical method, in the heterogeneity analysis, CochraneQ testP>0.05 indicates no statistical heterogeneity between studies, when the I² value exceeds 25%, 50%, 75%, it indicates low, moderate,high heterogeneity between studies, generally considered thatI²>50 exists substantial heterogeneity, and use random and fixed effect models for comparative analysis, with a confidence interval of 95%.Form a forest plot to represent relative risk and confidence interval.Determine the stability of the analysis results through the sensitivity analysis.When the number of studies included in the literature is greater than or equal to 10, use funnel plot analysis to determine publication bias.
3.Results
3.1 Basic information
According to the rules of search , a total of 3,349 articles were retrieved.After reading the titles, abstracts, and data of the articles,those related to drug and treatment regimen studies were excluded.Based on the exclusion criteria, 185 articles were initially screened.After reading the full text, 44 articles that met the inclusion criteria were evaluated and screened for quality.The process is shown in Figure 1.Total 29 articles achieved the score of 5 or above in quality assessment(Table 1).
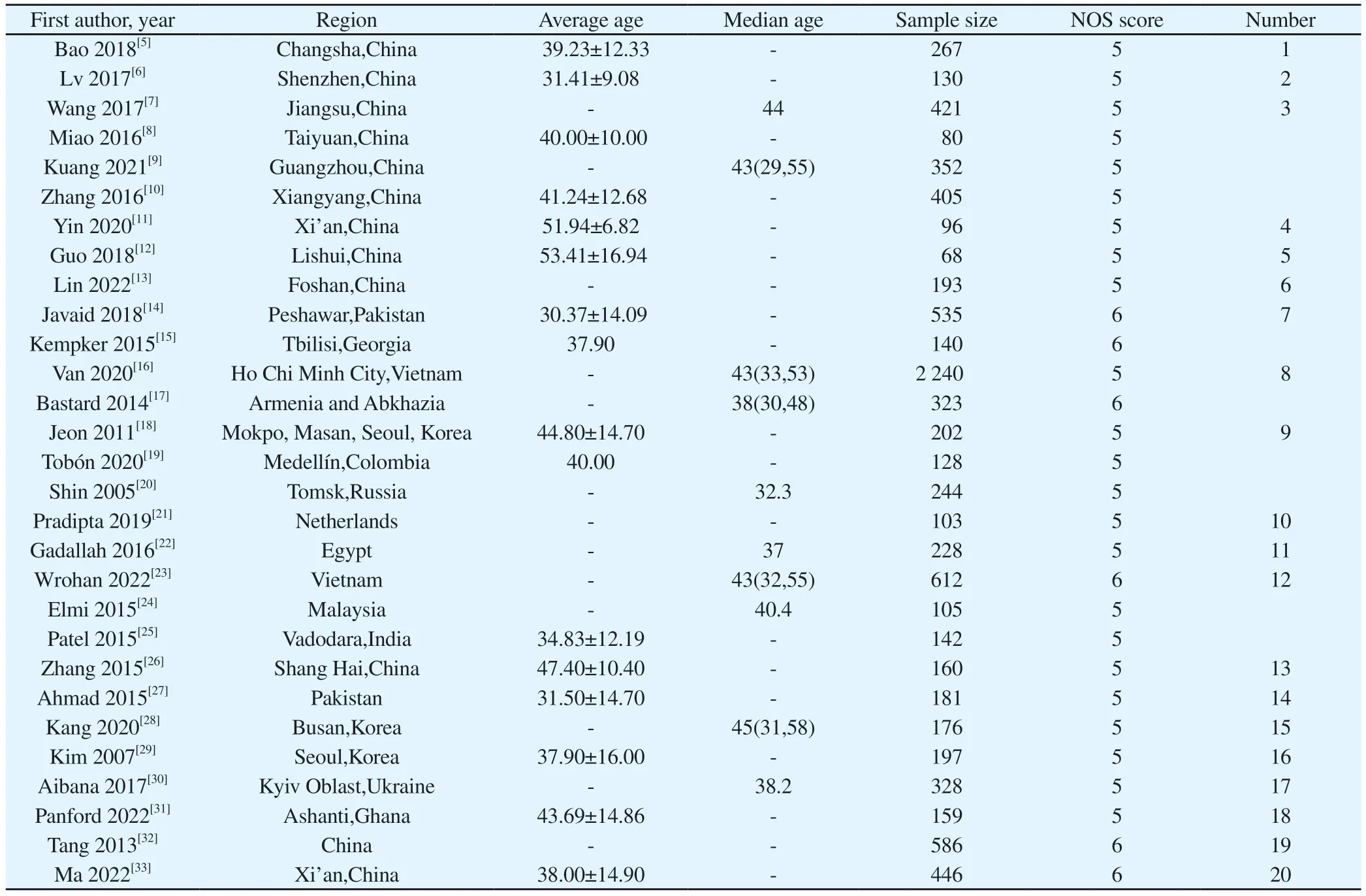
Tab 1 Basic characteristics and quality rating of literature
3.2 Inclusion of research literature
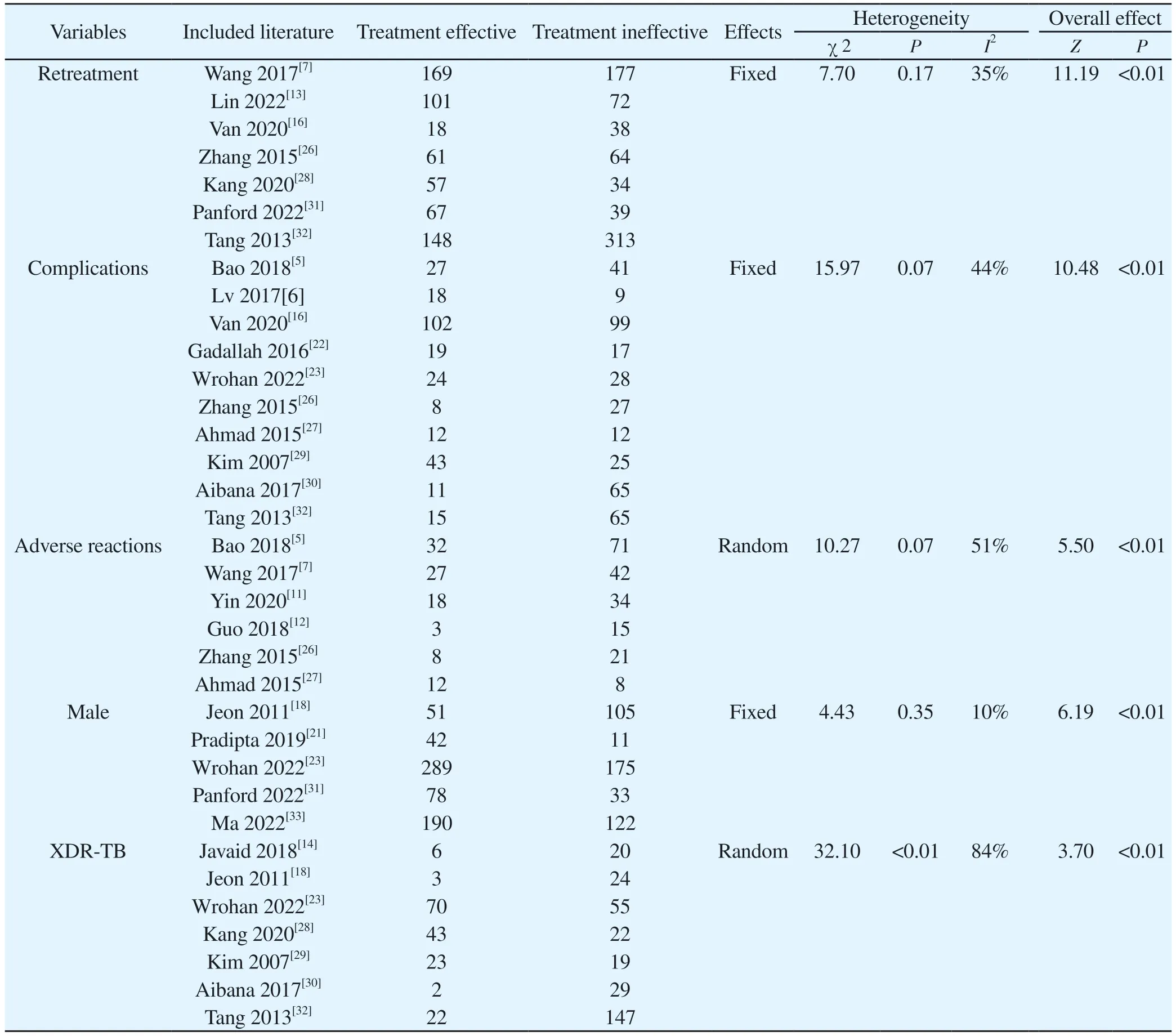
The included studies covered 36 regions in 14 countries, with a total sample size of 9217 people.The influencing factors related to the efficacy of MDR-TB included age, weight, marriage, education,BMI, smoking and drinking history, sputum culture negative conversion, sputum smear grade, second-line drug resistance,widespread drug resistance, pulmonary cavities, complications (such as HIV, diabetes.), adverse reactions, retreatment, irregular treatment.However, due to the limited number of literature, some factors were not suitable for combined analysis.In the end, only 20 articles were included in the final Meta-analysis, with a total sample size of 7,328 individuals.The study factors, their distribution in the treatmenteffective and ineffective groups, and heterogeneity tests are shown in Table 2.
3.3 Meta-analysis results
Retreatment, complications, adverse reactions, and gender were associated with the efficacy of multidrug-resistant tuberculosis treatment, with OR values and 95%CIof 0.22 (0.17-0.29), 0.38(0.32-0.46), 0.27 (0.17-0.44), and 0.43 (0.33-0.56), respectively.The results of the combined analysis of each factor were consistent after using fixed-effect models and random-effect models, with no significant differences.
3.3.1 The effect of retreatment on efficacy
A total of 6 articles were included in the heterogeneity test, and the results were low heterogeneity (I2=35%,χ2=7.70,P=0.17),OR (95%CI)=0.22 (0.17-0.29), and the pooled results were located on the left side of the null line, indicating a statistically significant pooled effect (Z=11.19,P<0.01), indicating that the treatment efficacy of the previously treated group was higher than that of the retreated group.In the sensitivity analysis, after excluding the study by Wang 2017[7], I2 was 0%, and heterogeneity was significantly reduced.The age range of the population included in this article was 18-65 years old, while other articles did not limit the age range of the population, indicating that the selection of the age range of the population in this article may be the source of heterogeneity.The forest plot is shown in Figure 2.
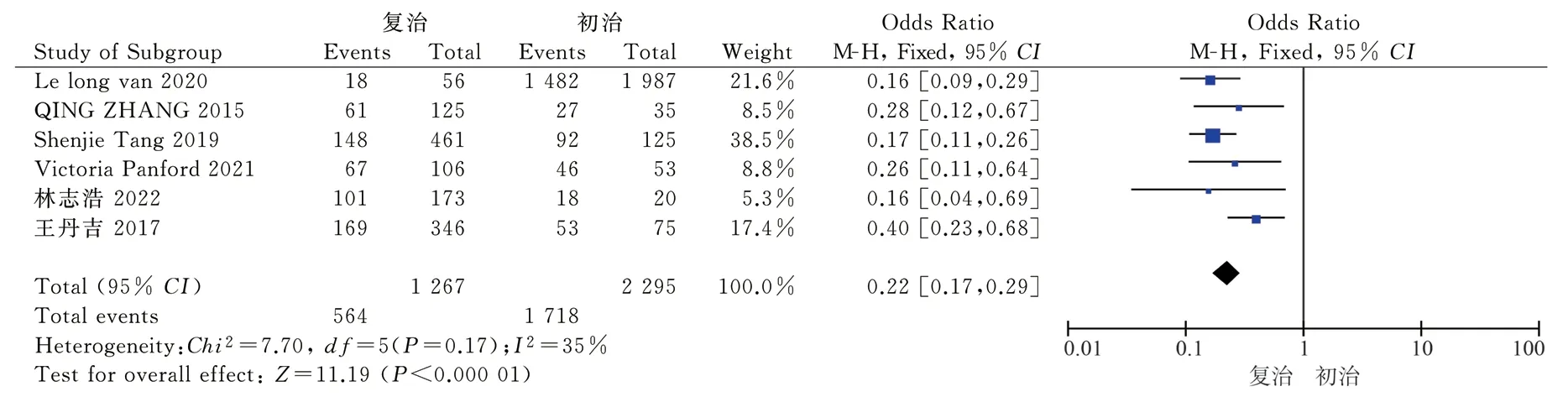
Fig 2 Meta analysis of the efficacy of retreatment and multidrug-resistant pulmonary tuberculosis patients
Tab 2 Distribution and heterogeneity test of various research factors in the treatment effective and ineffective groups
3.3.2 The impact of complications on the efficacy of treatment
A total of 10 articles were included in the heterogeneity test, and the results showed low heterogeneity (I2=44%,χ2=15.97,P=0.07),OR (95%CI)=0.38 (0.32-0.46), and the pooled effect was statistically significant (Z=10.48,P<0.01), indicating that the treatment efficacy in the group without complications was higher than that in the group with complications.In the sensitivity analysis, after excluding the study by Kim 2007[29], I2 was 23%, and the heterogeneity was significantly reduced.The population source of this article was non-HIV-infected patients, while other articles did not limit the population source.This article suggests that the population selection in this article may be the source of heterogeneity.The forest plot is shown in Figure 3.
3.3.3 The impact of adverse reactions on efficacy was analyzed in 6 articles
And the heterogeneity test results showed moderate heterogeneity(I2=51%,χ2=10.27,P=0.07), OR (95%CI)=0.27 (0.17-0.44), and the pooled effect was statistically significant (Z=5.50,P<0.01),indicating that the treatment efficiency of the group without adverse reactions was higher than that of the group with adverse reactions.Similar to the initial treatment and retreatment groups, in the sensitivity analysis, after excluding Wang 2017[7], I2 was 6%, and the heterogeneity was significantly reduced.The heterogeneity source was still considered to be the selection of the age range in this article.The forest plot is shown in Figure 4.
3.3.4 The effect of gender on efficacy was analyzed in 5 studies
And the heterogeneity test results showed low heterogeneity(I2=10%,χ2=4.43,P=0.35), with an OR (95%CI)=0.43 (0.33-0.56).The pooled effect was statistically significant (Z=6.19,P<0.01),indicating that the treatment efficacy rate in the female group was higher than that in the male group.In the sensitivity analysis, there was no significant change in heterogeneity after adjustment of the analysis.The forest plot is shown in Figure 5.
3.3.5 The impact of XDR-TB on the efficacy was included in 6 articles
The heterogeneity test result was high heterogeneity (I2=84%,2=32.10,P<0.01), OR (95%CI)=0.24 (0.12-0.52), and the combined effect was statistically significant (Z=3.70,P<0.01).In the sensitivity analysis, after adjusting the inclusion of the analysis and comparing with different effects models, the heterogeneity did not change significantly, and the factor of high heterogeneity was not suitable for combined analysis.The forest plot is shown in Figure 6
3.3.6 Publication bias
Funnel plot analysis was used to assess publication bias.Considering credibility, only studies with at least 10 included articles were analyzed.The funnel plot for the complication group showed a symmetrical distribution, indicating a low risk of publication bias.The funnel plot is shown in Figure 7.

Fig 3 Meta analysis of complications and efficacy in multidrug-resistant pulmonary tuberculosis patients
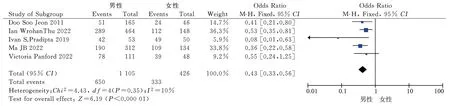
Fig 5 Meta analysis of gender and efficacy in multidrug-resistant pulmonary tuberculosis patients

Fig 7 Meta analysis funnel plot of complications and efficacy in multidrug-resistant pulmonary tuberculosis patients
4.Discussion
Due to the restrictions on travel and basic services caused by the COVID-19 pandemic, the number of newly diagnosed tuberculosis cases in 2020 and 2021 decreased significantly, but compared with 2019, the number of rifampicin resistant and multi drug resistant tuberculosis patients receiving treatment in 2020 and 2021 decreased[1], and the form of drug resistance of tuberculosis is still severe.This study combined the results of domestic and international studies on the factors affecting the efficacy of multidrug-resistant tuberculosis treatment through meta-analysis.The results showed that retreatment, adverse reactions, complications, and male gender were risk factors for effective treatment, with the strongest correlation being retreatment, with an OR (95% CI) of 0.22 (0.17-0.29).
Compared with patients who have not been treated before,patients who have been treated previously have more severe lung manifestations such as lung cavities, the extent of lesion involvement, and lung damage[34].In the literature of Javaid 2018[14]and Gadallah 2016[22], it is suggested that lung cavities is the contributing factor to the poor efficacy of MDR-PTB patients, which may be the reason for the poor efficacy of patients who have been treated previously.Male patients often do not pay enough attention to their disease conditions[35], and female patients have better treatment compliance during the anti-tuberculosis treatment[36], which ultimately leads to poor treatment efficacy.
The treatment regimen of MDR-PTB is complex, and there are many types of adverse reactions that may be caused, such as drug-induced liver injury, gastrointestinal discomfort, neurotoxic reactions.If not handled properly, it can easily lead to treatment interruption[37], resulting in treatment failure.Patients with complications such as underlying liver disease take a much higher risk of developing drug-induced liver injury during anti-tuberculosis treatment than patients without underlying liver disease[38].If the drug-induced liver injury is severe, it may require interruption of treatment[37], resulting in poor therapeutic effect.
Based on the results of the meta-analysis, in clinical practice, for patients with MDR-PTB, it is important to pay attention to the results of drug susceptibility testing during initial treatment, according to multiple drug susceptibility results in a timely manner, customize individualized treatment plans accordingly, improve the treatment efficiency of patients with initial treatment, and avoid conversion to patients with retreatment;in clinical work, adverse reactions should be detected as early as possible, and medication schemes should be adjusted in a timely manner;during medication, laboratory and imaging examinations of relevant organs should be conducted in a timely manner, and appropriate symptomatic treatment should be provided;for patients of different genders, health education should be carried out to improve patient compliance, so as to enhance the therapeutic effect for patients with MDR-PTB.
The limitations of this article are as follows: (1) Among the factors that affect the efficacy of multidrug-resistant tuberculosis treatment,age has been addressed in multiple articles, and the conclusions drawn are also varied.However, due to the inconsistent grouping method of age in each study, age was not included in the metaanalysis.(2) In the analysis of the impact of complications on the efficacy, the main source of heterogeneity among the literatures is the inconsistent definition of complications.in some literatures are defined as any complications, while others are defined as certain specific diseases, such as diabetes, HIV infection,which may lead to a certain degree of heterogeneity;Due to the limitations of the number of literature, some factors were not combined and analyzed due to the insufficient number of literature (less than 5 articles).The above conclusions still need to be verified by more high-quality research.
Conflict of interest statement All authors declare that there is no conflict of interest.
Author contribution statement Study design by Luo Qiening,Ou-Yang Fanxian;study implementation by Luo Qiening, Ou-Yang Fanxian, Liang Cuidan;data collection by Luo Qiening, Wang Weitong, Yu Huang;data analysis and interpretation by Luo Qiening,Liang Cuidan;article writing by Luo Qiening;article review and funding support by Ou-yang Fanxian.
 Journal of Hainan Medical College2023年13期
Journal of Hainan Medical College2023年13期
- Journal of Hainan Medical College的其它文章
- A comparative study of two methods for establishing a chronic non-bacterial prostatitis model in rats
- Relationship between microRNA-29c expression and clinicopathological features of gastric cancer
- Experimental study on the synergistic inhibition of malignant biological behavior of hepatocellular carcinoma cells by the combination of DMDD and sorafenib
- Effect of small interference RNA on expression of the Skp2 in human chondrocytes cell
- Regulation of Quan Du Zhong capsule on VEGF/bFGF and expression of Bcl-2/Bax and Caspase-3 protein in the repairing process of canine femoral head necrosis
- Association of novel and legacy PFAS with reproductive hormones in women of child-bearing age
