先天性心脏病合并气道异常患儿的临床分析
刘 慧 刘晓燕
先天性心脏病合并气道异常患儿的临床分析
刘 慧 刘晓燕
目的 探讨先天性心脏病(CHD)合并气道异常患儿的临床特征和预后。方法 回顾性分析重庆医科大学附属儿童医院2012年1~12月行胸部多排螺旋CT(MDCT)+气道重建和(或)纤维支气管镜(纤支镜)检查的住院CHD患儿的临床资料,按是否合并气道异常分为气道异常组和气道正常组,根据检查指征的不同,将气道异常组进一步分为心脏指征亚组和气道指征亚组。从病史中截取临床特征、CHD类型、气道异常类型、治疗和预后等资料,行气道正常组和异常组的比较。 结果 460例CHD病例进入分析。气道异常组195例(42.4%),男113例,中位年龄6月龄(1 d至14.5岁);气道正常组265例,男157例,中位年龄3.9月龄(1 d至15.4岁)。①166/195例存在1种气道异常,包括:单纯气道狭窄(125例,64.1%)、单纯气管性支气管(21例,7.2%)、单纯对称性支气管(8例,4.1%)和单纯气道软化(6例,3.1%)等,29例伴2种及以上气道异常;外源性压迫所致气道狭窄占80.9%(123/152)。②不同类型CHD合并气道异常的比例:血管环为84.2%,梗阻型为51.5%,发绀型为49.1%,左向右分流型为33.8%。气道指征亚组左向右分流型的比例高于心脏指征亚组(62.4%vs20.3%),发绀型比例低于心脏指征亚组(12.0%vs51.4%)。③气道异常组喘息、既往肺炎≥3次的比例显著高于气道正常组(P<0.05)。 ④气道异常组均未行外科治疗,随访复查MDCT+气道重建19例(轻度气道狭窄4例,中度气道狭窄15例),其中气道狭窄消失6例(CHD术后均>1年),减轻6例(CHD术后 <1年5例),无明显变化5例(出院>1 年,CHD均未矫治),加重者2例。气道异常组死亡22例。结论 儿童CHD合并气道异常的类型以气道狭窄最多见。对血管环和(或)反复呼吸道感染、喘息的CHD患儿应注意合并气道异常可能。大多数继发性轻中度气道狭窄在外源性压迫解除后1年以上,气道狭窄可能逐渐恢复正常。
先天性心脏病; 儿童; 气道异常; 临床特征
先天性心脏病(CHD)合并气道异常是危及患儿生命的重症之一,临床表现常无特异性,气道异常易被忽略,治疗棘手,病死率较高[1]。国内有学者认为有室间隔缺损(VSD)的CHD患儿合并气道异常的比例高于无VSD的CHD患儿[2],但各种CHD类型合并气道异常的相关报道较少,缺乏较大样本的研究,也缺乏大样本的随访预后分析。本文回顾性分析在重庆医科大学附属儿童医院(我院)行多排螺旋CT(MDCT)+气道重建和(或)纤维支气管镜(简称纤支镜)检查CHD患儿的临床资料,总结CHD与气道异常的相关性及特征。
1 方法
1.1 诊断及分类标准 ①CHD的诊断标准:通过超声心动图明确心脏或大血管异常,或行MDCT+血管重建或心导管检查或心血管造影明确诊断。CHD分为4个类型[3]:左向右分流型、梗阻型、发绀型及血管环;右旋心、二尖瓣病变、主肺动脉隔缺损、右冠状动脉右室瘘和左冠状动脉肺动脉瘘等,因发病率较低不纳入本文统计。②气道异常的诊断标准:通过MDCT+气道重建和(或)纤支镜诊断;气道狭窄程度=(狭窄近端气道正常直径-最狭窄处直径)/狭窄近端气道正常直径×100%;气道狭窄程度,轻度狭窄≤25%,中度狭窄~75%,重度狭窄≥75%[4]。
1.2 MDCT+气道重建和(或)纤支镜检查指征 ①需明确心脏、大血管畸形的类型。②因反复呼吸道感染、内科治疗效果欠佳或 CHD术后长期肺不张/肺实变、脱机困难考虑气道异常。
1.3 病例纳入标准 ①我院2012年1~12月住院病例电子病案系统中出院诊断包含有CHD的全部病例;②行MDCT+气道重建或纤支镜检查;③2012年前入我院和2012年多次入我院的病例,仅纳入2012年首次MDCT+气道重建或纤支镜结果。
1.4 病例排除标准 病史中未描述CHD和气道异常具体类型的病例。
1.5 分组 根据CHD是否合并气道异常分为气道异常组和气道正常组;根据检查指征的不同,将气道异常组分为心脏指征和气道指征亚组。
1.6 MDCT和纤支镜检查方法 MDCT采用GE Light Speed 64排VCT(GE,USA), 图像后处理工作站:AW 4.4 (GE,美国), 扫描范围自胸廓入口至横隔下2~3 cm,并在原始数据基础上行气管、支气管多平面重建。根据患儿年龄选择Olympus不同规格的纤支镜,在气道黏膜局部麻醉下观察气管支气管内腔变化。
1.7 随访 合并气道异常的CHD患儿均建议出院后定期来我院随访,随访内容:询问呼吸道感染次数、体重增长情况,复查心脏彩超,必要时行MDCT+气道重建复查;未能来我院随访的患儿,由科室专人电话随访呼吸道感染次数、体重增长情况及转归(存活或死亡)。
1.8 分析资料 从住院病史截取以下资料进行分析,①临床特征:咳嗽、喘息、气促/呼吸困难、既往肺炎次数等;②CHD类型:根据超声心动图、MDCT+血管重建、心导管检查及心血管造影检查报告的描述;③气道异常类型:依据纤支镜或MDCT+气道重建检查报告的描述;④入住我院期间治疗情况;④随访内容。
1.9 统计学方法 采用SPSS 17.0软件进行统计学分析,计量资料用中位数(范围)表示,计数资料比较采用χ2检验,P<0.05 为差异有统计学意义。行×列表多个组间的两两比较采用χ2检验,调整检验水准α'=2α/k(k-1), α=0.05,k为分组数。
2 结果
2.1 一般情况 2012年1~12月460例住院CHD患儿进入分析,气道异常组195例(42.4%),MDCT诊断162例,纤支镜诊断16例,MDCT和纤支镜同时诊断17例;男113例,女82例,中位年龄6月龄(1 d至14.5岁)。气道正常组265例(57.6%),男157例,女108例,中位年龄3.9月龄(1 d至15.4岁)。两组入院时年龄差异有统计学意义(P<0.05 ),性别构成差异无统计学意义(P>0.05)。
气道异常组:心脏指征亚组76例(男38例),中位年龄5.9月龄(1 d至14.5岁);气道指征亚组119例(男75例),中位年龄6.1月龄(1d至10.5岁),其中8例为CHD术后长期肺不张/肺实变、脱机困难;两亚组间年龄差异无统计学意义(P>0.05 ),性别构成差异有统计学意义(P<0.05 )。
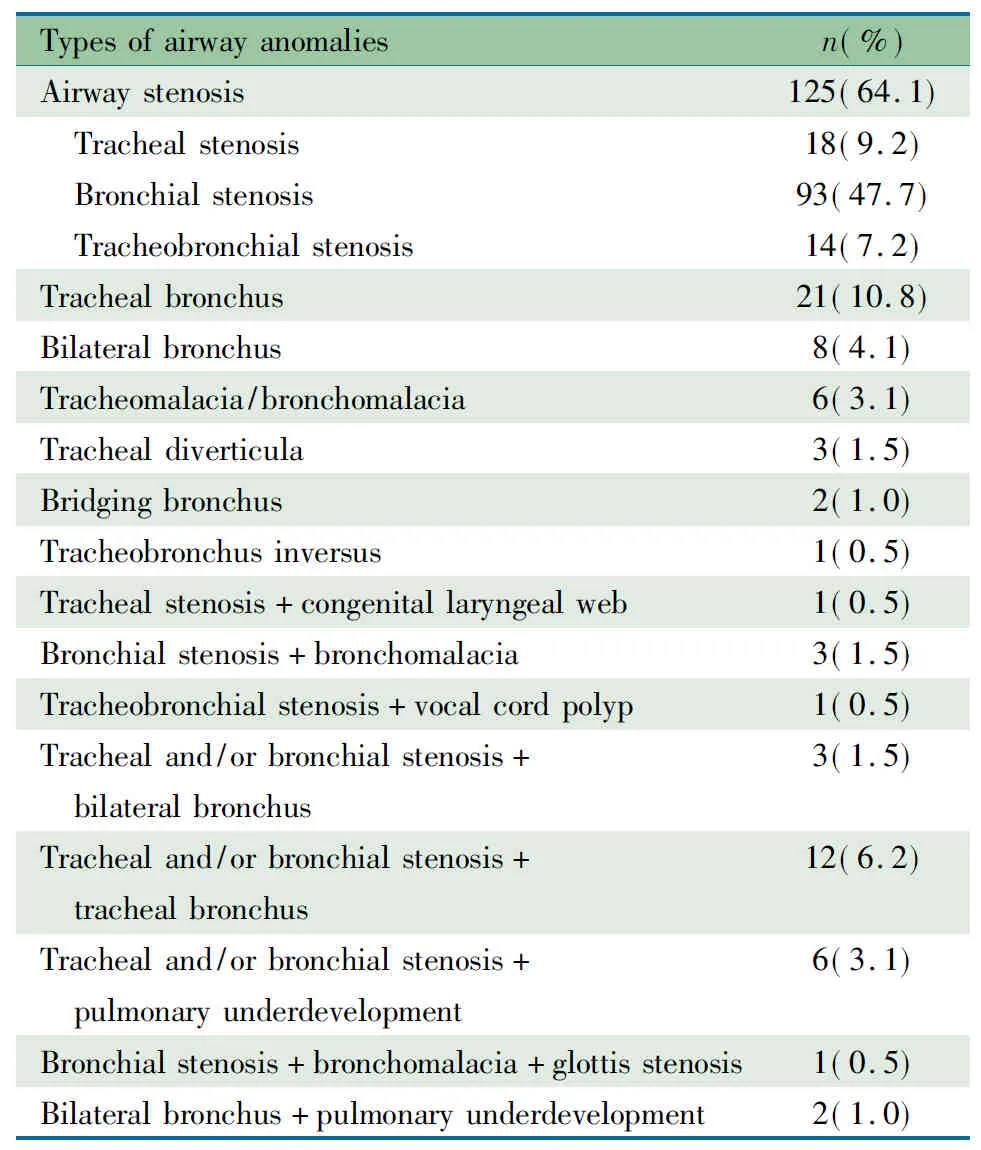
2.2 气道异常类型 表1显示,166例(85.1%)存在1种气道异常,包括单纯气道狭窄125例(轻、中、重度气道狭窄分别为67例、55例及3例),气管性支气管21例,对称性支气管8例,支气管软化6例等。29例伴2种及以上气道异常,包括支气管软化+气管/支气管狭窄12例,肺发育不良+气管/支气管狭窄6例等。123/152例(80.9%)单纯和合并气道狭窄病例,考虑因心脏增大或血管畸形外压导致的继发性气道狭窄。
表1 195例CHD患儿合并的气道异常类型
Tab 1 The types of airway anomalies of 195 cases with CHD
Typesofairwayanomaliesn(%)Airwaystenosis125(64.1) Trachealstenosis18(9.2) Bronchialstenosis93(47.7) Tracheobronchialstenosis14(7.2)Trachealbronchus21(10.8)Bilateralbronchus8(4.1)Tracheomalacia/bronchomalacia6(3.1)Trachealdiverticula3(1.5)Bridgingbronchus2(1.0)Tracheobronchusinversus1(0.5)Trachealstenosis+congenitallaryngealweb1(0.5)Bronchialstenosis+bronchomalacia3(1.5)Tracheobronchialstenosis+vocalcordpolyp1(0.5)Trachealand/orbronchialstenosis+ bilateralbronchus3(1.5)Trachealand/orbronchialstenosis+ trachealbronchus12(6.2)Trachealand/orbronchialstenosis+ pulmonaryunderdevelopment6(3.1)Bronchialstenosis+bronchomalacia+glottisste-nosis1(0.5)Bilateralbronchus+pulmonaryunderdevelop-ment2(1.0)
2.3 CHD类型与气道异常的相关性 气道异常组右旋心2例,二尖瓣病变1例,主肺动脉隔缺损1例;气道正常组主肺动脉隔缺损、右冠状动脉右室瘘和左冠状动脉肺动脉瘘各1例,不归属于本文分析的4种CHD类型,不进入分析。气道异常组2例伴有心脏畸形的血管环合并有气道狭窄,但其气道狭窄并非血管环所致,1例伴有动脉导管未闭(PDA)及ASD,归为左向右分流型;1例伴PDA、ASD及肺动脉瓣狭窄(PS),归为梗阻型。
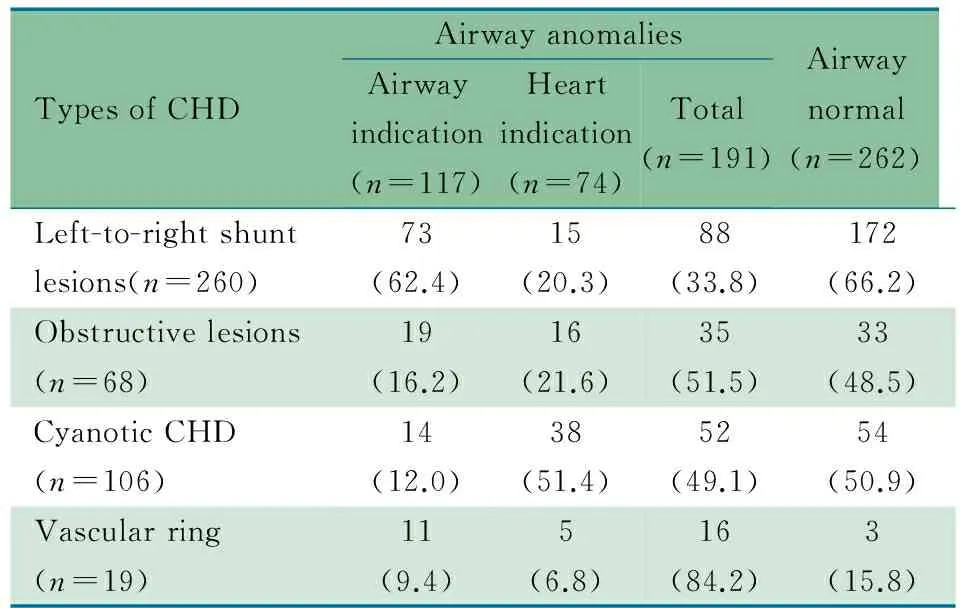
表2显示,气道异常组和气道正常组CHD类型差异有统计学意义(χ2=25.631,P<0.05)。血管环类型CHD合并气道异常占84.2%,左向右分流型CHD合并气道异常占33.8%。
进一步按指征分析,心脏指征和气道指征亚组间CHD类型不同(χ2=44.380,P<0.001),气道指征亚组左向右分流型比例较心脏指征亚组高(62.4%vs20.3%),发绀型比例较心脏指征亚组低(12.0%vs51.4%),差异均有统计学意义(P均<0.05)。
表2 不同CHD类型合并气道异常的比例[n(%)]
Tab 2 The comparison of four different types of CHD with airway anomalies[n(%)]
TypesofCHDAirwayanomaliesAirwayindication(n=117)Heartindication(n=74)Total(n=191)Airwaynormal(n=262)Left-to-rightshuntlesions(n=260)73(62.4)15(20.3)88(33.8)172(66.2)Obstructivelesions(n=68)19(16.2)16(21.6)35(51.5)33(48.5)CyanoticCHD(n=106)14(12.0)38(51.4)52(49.1)54(50.9)Vascularring(n=19)11(9.4)5(6.8)16(84.2)3(15.8)
Notes The CHD types between children with or without airway anomalies differed siginicantly,χ2=25.631,P<0.05. Airway anomalies group: Left-to-right shunt lesionsvsobstructive lesions + cyanotic congenital heart defects,χ2=11.304,P=0.001;Left-to-right shunt lesionsvsVascular ring,χ2=19.209,P=0.000; Vascular ringvsobstructive lesions + cyanotic congenital heart defects,χ2=8.056,P=0.005,α'=0.0167. The CHD types between airway indication and heart indication subgroups differed siginicantly,χ2=44.380,P<0.001
2.4 临床特征比较 表3显示,气道异常组和正常组既往患肺炎次数≥3次及喘息发生率差异有统计学意义(P<0.05),咳嗽、气促/呼吸困难、肺炎和呼吸衰竭的发生率差异无统计学意义(P均>0.05)。 与心脏指征亚组比较,气道指征亚组咳嗽(χ2=28.449,P<0.05)、喘息(χ2=23.573,P<0.05)及既往肺炎≥3次(χ2=10.230,P<0.05)发生率差异有统计学意义,气促/呼吸困难、肺炎和呼吸衰竭两亚组间发生率差异无统计学意义(P均>0.05)。
2.5 治疗与转归 气道异常组中102例行CHD外科手术,1例行CHD介入术,92例行内科治疗。均未同期行气道狭窄矫治术或气管支架植入术,3例合并气管性支气管患儿在CHD术后出现肺不张/肺实变,均行纤支镜灌洗。住院期间死亡9例(2例因肺动脉吊带所致的气道重度狭窄术后撤离呼吸机困难死亡,另外7例因复杂CHD死亡),放弃治疗9例, 177例好转出院。
112/186例(60.2%)出院后来我院随访或电话随访,平均随访15(3~25)个月。随访死亡13例,其中考虑肺动脉吊带所致重度气道狭窄1例,术后不能撤离呼吸机,放弃治疗;复杂CHD 12例(气道指征亚组2例,心脏指征亚组10例)。
表3 气道正常组和异常组临床特征比较[n(%)]
Tab 3 The comparison of clinical features between airway normal and abnormal groups[n(%)]

TypesofCHDAirwayanomaliesAirwayindication(n=119)Heartindication(n=76)Total(n=195)Airwaynormal(n=265)χ21)P1)Cough97(81.5)34(44.7)3)131(67.2)157(59.2)3.0210.082Anhelation/dyspnea81(68.1)42(55.3)123(63.1)152(57.4)1.5280.216Wheeze2)67(56.3)16(21.0)3)83(42.6)73(27.5)11.3030.001Pneumonia100(84.0)56(73.7)156(80.0)215(81.1)0.0920.761Respiratoryfailure34(28.6)16(21.1)50(25.6)66(24.9)0.0320.858Pneumonia≥3times24(20.2)3(0.4)3)27(13.8)20(7.5)4.8590.028
Notes 1) Airway anomalies groupvsairway normal group; 2) asthma was excluded; 3) Airway indication subgroupvsheart indication subgroup,P<0.05
85/186例伴气道狭窄,其中19例(手术14例)随访行MDCT+气道重建检查;6例(气道轻度狭窄1例,中度狭窄5例)CHD术后随访13~25个月气道狭窄消失;6例(气道中度狭窄)CHD术后随访3~23个月气道狭窄减轻;5例(气道轻度狭窄3例,中度狭窄2例)随访12~16个月气道狭窄较前无明显变化,导致气道狭窄的血管及心脏畸形均未矫治,其中肺血管畸形1例,迷走锁骨下动脉2例,心脏畸形2例;2例(气道中度狭窄)CHD术后随访3和8个月,狭窄范围及狭窄程度较前加重。
气道正常组14/265例住院期间死亡,余251例出院随访6~26个月,平均17个月,死亡8例。
3 讨论
本研究CHD合并气道异常195例(42.4%),我院2012年1个季度完成MDCT+气道重建和(或)纤支镜的非CHD患儿中气道异常占19.2%(62/323),提示CHD合并气道异常的比例较高。本文CHD合并气道异常病例的病死率为11.3%(22/195),高于CHD未合并气道异常的病死率(8.3%,22/265)。
CHD合并的气道异常类型多样,包括气道狭窄、气管性支气管、对称性支气管和气道软化等,多数学者认为以气道狭窄多见,亦有研究显示气管性支气管、气管/支气管软化或声带麻痹多见[5~9]。本文病例以气道狭窄多见(152/195,77.9%),其次是气管性支气管、对称性支气管和气管/支气管软化。有文献报道气道狭窄以继发性多见,多由血管畸形或增大的心脏压迫所致[1,10]。本文病例80.9%(123/152)的气道狭窄可能由外在压迫所致。气管性支气管是一种相对常见的先天性气道畸形,文献报道其发生率为1.1%(11/1 021)[11],但其开口较小,与主气管形成锐角,易致气流湍流及分泌物引流不畅;无呼吸道感染时一般无明显临床症状,一旦合并呼吸道感染,会加重病情。气管性支气管若内科治疗效果欠佳,出现肺不张/肺实变,可行纤支镜灌洗,病情反复者可行手术治疗[12]。本文气管性支气管占气道异常的16.9%(33/195),有3例CHD术后出现肺不张/肺实变(其中1例脱机困难),均行纤支镜灌洗,好转出院。
本研究结果显示,不同类型的CHD合并气道异常的比例不同,血管环合并气道异常比例最高(84.2%),易致相应气道狭窄,其中3例因气道狭窄明显、脱机困难死亡;其次是梗阻型(51.5%)和发绀型(49.1%),虽然左向右分流型合并气道异常的比例相对较低(33.8%),但其病例数占气道异常的比例为45.1%(88/195),也不容忽视。进一步分析显示,气道指征亚组和心脏指征亚组的CHD类型不同,前者左向右分流型比例较高,可能与左向右分流型多有肺淤血,易致反复呼吸道感染、肺部感染难控制有关;心脏指征亚组发绀型比例较高,考虑发绀型多为复杂CHD,早期患儿即表现为面色或指趾发绀,心脏听诊多有杂音,提示心脏或大血管畸形,为明确心脏、大血管畸形类型检查发现。
婴幼儿气道发育不完善,管腔较成人小,加之气道狭窄、软化和解剖起源异常等因素,易致气流受阻、呼吸道分泌物引流不畅,出现反复呼吸道感染、喘息、术后脱机困难和长期肺不张/肺实变。本文13.8% CHD合并气道异常患儿既往患肺炎次数≥3次,42.6%的患儿有喘息,显著高于气道正常组。同时气道指征亚组也更易合并咳嗽、喘息及反复呼吸道感染;但CHD合并气道异常的临床表现无特异性,易被漏诊。本文38.9%(76/195)的患儿因明确CHD类型,行心血管重建发现气道异常,4.1%(8/195)因CHD术后长期肺不张/肺实变、脱机困难而发现气道异常。因此提示CHD患儿出现CHD及肺炎本身不能解释的喘息、反复呼吸道感染、术后长期肺不张/肺实变和脱机困难等情况时,尤其是血管环、梗阻型及发绀型CHD患儿更应考虑气道异常可能,需完善胸部MDCT+气道重建或纤支镜等检查。
气道异常的治疗包括内科治疗、外科手术及支架植入术。根据气道异常的类型,气道病变的部位、范围及程度选择不同的治疗方法。目前CHD合并气道狭窄的治疗仍存在争议。国外有研究发现,内科治疗与气道狭窄手术治疗的病死率分别为9%和 27%,对于漏斗形及部分性气管狭窄(管腔直径>
正常的60%),内科治疗是一种安全可行的方法;同时发现气道狭窄患儿婴儿期后,气道管腔较同龄正常儿童增长快,9岁时可达到正常儿童水平[13]。但对于严重的气道狭窄,内科治疗效果欠佳,一期手术同时行气道狭窄及心脏畸形修复是比较合理的治疗方法[14]。对于呼吸道症状重不宜手术及CHD术后严重的气道狭窄,支架植入是一种较好的治疗方法[15,16]。由于我院未开展气道手术或支架植入术,均予以内科治疗。CHD术后随访发现,11/19例轻、中度气道狭窄患儿在CHD术后外在压迫解除后气道狭窄消失或有所减轻。
[1]Jhang K, Park JJ, Seo DM, et al. Perioperative evaluation of airway in arch obstruction and intracardic defects. Ann Thorac Surg,2008,85(5):1753-1758
[2]Zeng SL(曾双林),Li YJ, Huang T, et al. Relationship between congenital heart disease and bronchial dysplasia. Chin J Contemp Pediatr(中国当代儿科杂志),2011,13( 11):893-895
[3]Myung K.Park. Pediatric cardiology for practitioners. 5th edition. The United States of America: Mosby.2007, 161,192,215,303,309
[4]Wang RP(王荣品), Liang YH, Huang MP, et al. Multi-slice spiral CT in the diagnosis of congenital heart diseases associated with tracheobronchial stenosis in children. Chin J Radiol(中华放射学杂志),2010,44( 8) :811-815
[5]Qian J(钱娟),Wang Y, Yin Y, et al. A comparison between fiberoptic bronchoscopy and multislice helical CT in the diagnosis of airway anomalies of children with congenital hesrt diseases. Chin Pediatr Emerg Med(中国小儿急救医学),2007,14(6):508-510
[6]Wang CC, Chen SJ, Wu ET, et al.Lower airway anomalies in children with CATCH 22 syndrome and congenital heart disease. Pediatr Pulmonol,2013,48(6):587-591
[7]Ming Z, Lin Z. Evaluation of tracheal bronchus in Chinese children using multidetector CT. Pediatr Radiol, 2007,37(12):1230-1234
[8] Pfammatter JP,Casaulta C,Pavlovic M,et al. Important excess morbidity due to upper airway anomalies in the perioperative course in infant cardiac surgery.Ann Thorac Surg, 2006, 81(3):1008-1012
[9]Guillemaud JP,El-Hakim H,Richards S,et al. Airway pathologic abnormalities in symptomatic children with congenital cardiac and vascular disease.Arch Otolaryngol Head Neck Surg,2007,133(7):672-676
[10] Ho AS, Koltai PJ.Pediatric tracheal stenosis .Otolaryngol Clin Nort Am,2008,41(5):999-1021
[11]Dave MH, Gerber A, Bailey M, et al.The prevalence of tracheal bronchus in pediatric patients undergoing rigid bronchoscopy. J Bronchology Interv Pulmonol, 2014 ,21(1):26-31
[12]Heyer CM,Kagel T,Lemburg SP,et al.Evaluation of tracheobronchial anomalies in children using low-dose multidetector CT:report of a 13-year-old boy with a tracheal bronchus and recurrent pulmonary infections.Pediatr Pulmono1,2004,38(2):168-173
[13]Cheng W, Manson DE, Forte V,et al. The role of conservative management in congenital tracheal stenosis:an evidencebased long-term follow-up study.J Pediatr Surg,2006,41(7):1203-1207
[14]Tsai MH,Wong KS,Lien R,et a1.Heliox as the rescue therapy for a neonate with congenital tracheal stenosis, pulmonary artery sling, and intracardiac anomalies.Am J Perinatol,2009,26(5):357-360
[15]Xu X(许煊),Ding H,Li DD,et al. Study on the removal indication for children with congenital heart combined with bronchial stenosis after tracheal stenting. Chin J Evid Based Pediatr(中国循证儿科杂志), 2012,7(5):326-330
[16]Xu X, Li D, Zhao S, et al. Treatment of congenital tracheal stenosis by balloon-expandable metallic stents in paediatric intensive care unit .Interact Cardiovasc Thorac Surg,2012,14(5):548-550
(本文编辑:丁俊杰)
Clinical analysis of congenital heart disease with airway anomalies in children
LIUHui,LIUXiao-yan
(DepartmentofCardiology,Children'sHospitalofChongqingMedicalUniversity,MinistryofEducationKeyLaboratoryofChildDevelopmentandDisorders,KeyLaboratoryofPediatricsinChongqing,ChongqingInternationalScienceandTechnologyCooperationCenterforChildDevelopmentDisorders,Chongqing400014,China)
LIU Xiao-yan,E-mail:lxylxy65@163.com
ObjectiveTo investigate the prognosis and clinical features of congenital heart disease (CHD) with airway anomalies in children.MethodsChildren with CHD hospitalized from Jan. 2012 to Dec. 2012 were underwent chest multidetector helical CT airway reconstruction and/or fiberobronchoscopy. Patients were divided into airway abnormal group and airway normal group, the former group was divided into airway indication subgroup and heart indication subgroup. Clinical data including clinical features, ultrasonic cardiogram, chest multidetector helical CT airway reconstruction, and fiberobronchoscopy inspection results were retrospectively analyzed. The treatment, outcome and prognosis of CHD patients with airway anomalies were evaluated.Results A total of 460 CHD cases were recruited, of them 195(42.4%) cases of CHD accompanied with airway anomalies. The types of airway anomalies included airway stenosis, tracheal bronchus, symmetrical bronchus and airway malacia. Among them, airway stenosis was the most common(152/195, 77.9%),mainly resulting from extrinsic compression by vascular malformation or enlarged heart (80.9%,123/151).The incidences of airway anomalies differed among different CHD (vascular rings, 84.2%; outlet obstructive constipation, 51.5%; cyanotic CHD, 49.1%; left-to-right shunt, 33.8%;P<0.05). The proportion of CHD differed from airway indication subgroup and heart indication subgroup(P<0.05),the ratio of left-to-right shunt was higher in airway indication subgroup(62.4%vs20.3%),the ratio of cyanotic CHD was higher in heart indication subgroup (12.0%vs51.4%). Airway abnormal group was more likely to result in wheezing and pneumonia≥3 times than airway normal group, and airway indication subgroup was more likely to result in cough, wheezing and repeated pneumonia≥3 times than heart indication subgroup. The total mortality rate was 18.2% (22/121). None patients in airway abnormal group underwent surgery.Nineteen cases with airway stenosis (4 with mild stenosis and 15 with moderate stenosis) underwent multidetector helical CT airway reconstruction. Six of them recovered 1 year later after cardiac surgery and 6 of them improved within 1 year after operation. No change was found in 5 cases while 2 cases were progressed without correction of cardiovascular malformations. Among airway abnormal group, nine cases died in hospitalization and 13 cases died during follow-up.ConclusionThe morbidity and mortality of children with CHD and airway anomalies was high. Airway stenosis was the most common type of airway anomalies. It should be noticed that vascular rings and/or CHD patients who had repeatedly respiratory infection, wheeze, long-term pulmonary atelectasis or pulmonary consolidation of post operation and failure of ventilator weaning might be accompanied with airway anomalies. Conservative management was the first choice for mild and moderate airway stenosis. More than 1 year after release of extrinsic compression, airway stenosis could recover gradually in part of patients.
Congenital heart disease; Children; Airway anomalies; Clinical features
10.3969/j.issn.1673-5501.2015.05.005
重庆市科委自然科学基金:CSTC,2010BB5373
重庆医科大学附属儿童医院心血管内科,儿童发育疾病研究教育部重点实验室,儿科学重庆市重点实验室,重庆市儿童发育重大疾病诊治与预防国际科技合作基地 重庆,410014
刘晓燕,E-mail:lxylxy65@163.com
2015-01-17
2015-07-16)