Medium-term outcomes of artificial disc replacement for severe cervical disc narrowing
Chao-Hung Yeh, Che-Wei Hung, Cheng-Hsing Kao, Chien-Ming Chao
1Department of Neurosurgery, Chi Mei Medical Center, Tainan, Taiwan
2Department of Spine Center, Jhong Jheng Orthopedic Hospital, Kaohsiung, Taiwan
3Department of Intensive Care Medicine, Chi Mei Medical Center, Liouying, Tainan, Taiwan
4Department of Nursing, Min-Hwei College of Health Care Management, Tainan, Taiwan
Medium-term outcomes of artificial disc replacement for severe cervical disc narrowing
Chao-Hung Yeh1, Che-Wei Hung2, Cheng-Hsing Kao2, Chien-Ming Chao3,4*
1Department of Neurosurgery, Chi Mei Medical Center, Tainan, Taiwan
2Department of Spine Center, Jhong Jheng Orthopedic Hospital, Kaohsiung, Taiwan
3Department of Intensive Care Medicine, Chi Mei Medical Center, Liouying, Tainan, Taiwan
4Department of Nursing, Min-Hwei College of Health Care Management, Tainan, Taiwan
Objective: To determine if the Bryan cervical disc prosthesis could relieve objective neurological symptoms, signs, and restore mobility in patients with severe cervical disc narrowing.
Methods: Clinical data of thirty-two patients underwent Bryan cervical disc replacement has been collected from April 2006 to February 2010. Severe cervical disc narrowing with grade V disc degeneration were included in this study. Bryan cervical disc prostheses have been implanted through anterior approach. Japanese Orthopedics Association (JOA) score, visual analog scale, Odom’s scale, and flexion-extension radiological follow-ups were applied for evaluations.
Results: A total of 41 Bryan disc prostheses from 32 patients with an average follow-up duration of 33.5 months (range 23 to 44 months) were evaluated. Clinical functions of patients were significantly improved. Preoperative averaged visual analog scale score of 6.3±2.2 was decreased to 1.3±1.2 (at 36 months,P<0.001), while preoperative averaged JOA score of 14.4± 1.2 was increased to 16.3±0.9 (at 36 months, P<0.001). Thirty of 32 patients received excellent to good outcomes in Odom’s scale. Averaged mobility was restored to (9.9±3.2)° at the last follow-up evaluation of 36 months. No subsidence or migration of implant was identified.
Conclusions: Acceptable clinical outcome for treatment of severe cervical disc narrowing with cervical disc replacement technique has been performed in current study. Most patients maintained good postoperative mobility and no significant adjacent level degeneration were found. Cervical disc replacement may be applicable in treatment of severe cervical disc narrowing; however, longer follow-ups are required for ensuring the long-term efficacy of cervical disc replacement.
ARTICLE INFO
Article history:
Received 26 Dec 2014
Received in revised form 2014
Accepted
Available online
Cervical disc prosthesis
1. Introduction
Degenerative cervical disc narrowing is a common cause of neck pain, radiculopathy, and myelopathy due to degenerative disc disease (DDD). Over the past fifty years, anterior approach for cervical decompression with or without fusion has provided good clinical results[1]. However, several complications about cervical arthrodesis included graft collapse, graft expulsion, pseudoarthrosis, donor-site morbidity, neck stiffness, cervical lordotic loss[2,3], and accelerated degeneration at adjacent levels caused from arthrodesis were also reported[4-6].
Total disc replacement (TDR) is an increasingly accepted and diffusing technique used to treat cervical DDD. Symptomatic patients with soft disc hernia or moderate DDD can be considered for TDR. In consideration about the postoperative deterioration due to arthrodetic surgery, cervical artificial disc replacement was developed to preserve mobility of the implantation level, avoid deformity of spinal column, reduce stresses on adjacent discs, and restore intervertebral height to achieve decompressionwithout filling any bone grafts. At present, cervical disc replacement has demonstrated good clinical results in managing single- or multi-level spondylotic radiculopathy, myelopathy alone, or combined both of the symptoms[7-10], and could also maintain the range of motion in flexion/ extension activity[11,12]. Previousin vitroinvestigation has also found that cervical disc replacement maintained intradiscal pressures at adjacent level and approximate kinematics of reconstructed level as performances of intact spine[13].
Surgical treatment for severe cervical disc narrowing involves anatomic correction of the degenerative pathologic entities that compress a nerve root or the spinal cord. Severe cervical disc narrowing would significantly result in decrease of mobility of motion segment[14-16], which would also be the main reason to increase the adjacent level degeneration and symptoms. In cases of severe disc narrowing, the complication rates are probably higher mainly due to the fact that frequently multiple levels are operated.
Previous literature has reported the use of Bryan disc in cervical disc narrowing. However, application of cervical disc replacement specifically for treating severe cervical disc narrowing has never been performed. The purpose of this study was to firstly demonstrate the application of Bryan disc on treatment of severe cervical disc narrowing. In addition, clinical and radiologic outcomes of patients in single- and multi-level replacement during the follow-up period were evaluated. Neurological symptoms and signs, stability, and mobility restoration were considered in these postoperative follow-ups.
2. Materials and methods
2.1. Patient population
This study recruited 41 arthroplasties from 32 patients (18 males and 14 females) using the Bryan cervical disc system (Medtronic Sofamor Danek, Memphis, TN, USA) from April 2006 to February 2010 in Chi-Mei Medical Center, Tainan, Taiwan. Among these 32 patients, a single level procedure was performed in 24 patients, a two-level procedure in seven patients and a three-level procedure in one patient. All the surgeries were performed by one senior surgeon of the authors. A comprehensive grading system for cervical disc degeneration was executed based on the reported literature[16]. Inclusion criteria included grade V disc degeneration, over 40% collapse of normal disc height, and marked osteophytes (more than 2 mm) as shown in Figures1a and 2a. Patients with active systemic infection, allergy to implantation materials, osteoporosis, marked cervical instability, deformity, significant facet joint arthropathy, trauma, and tumor were excluded. Preoperative and postoperative Japanese Orthopedics Association (JOA) score, visual analog scale (VAS) and Odom’s scale[17] were recorded for outcome analysis. Odom’s scale was used as it is the most commonly used scale and is relatively simple. Quantitative information of patients was summarized in Table 1.
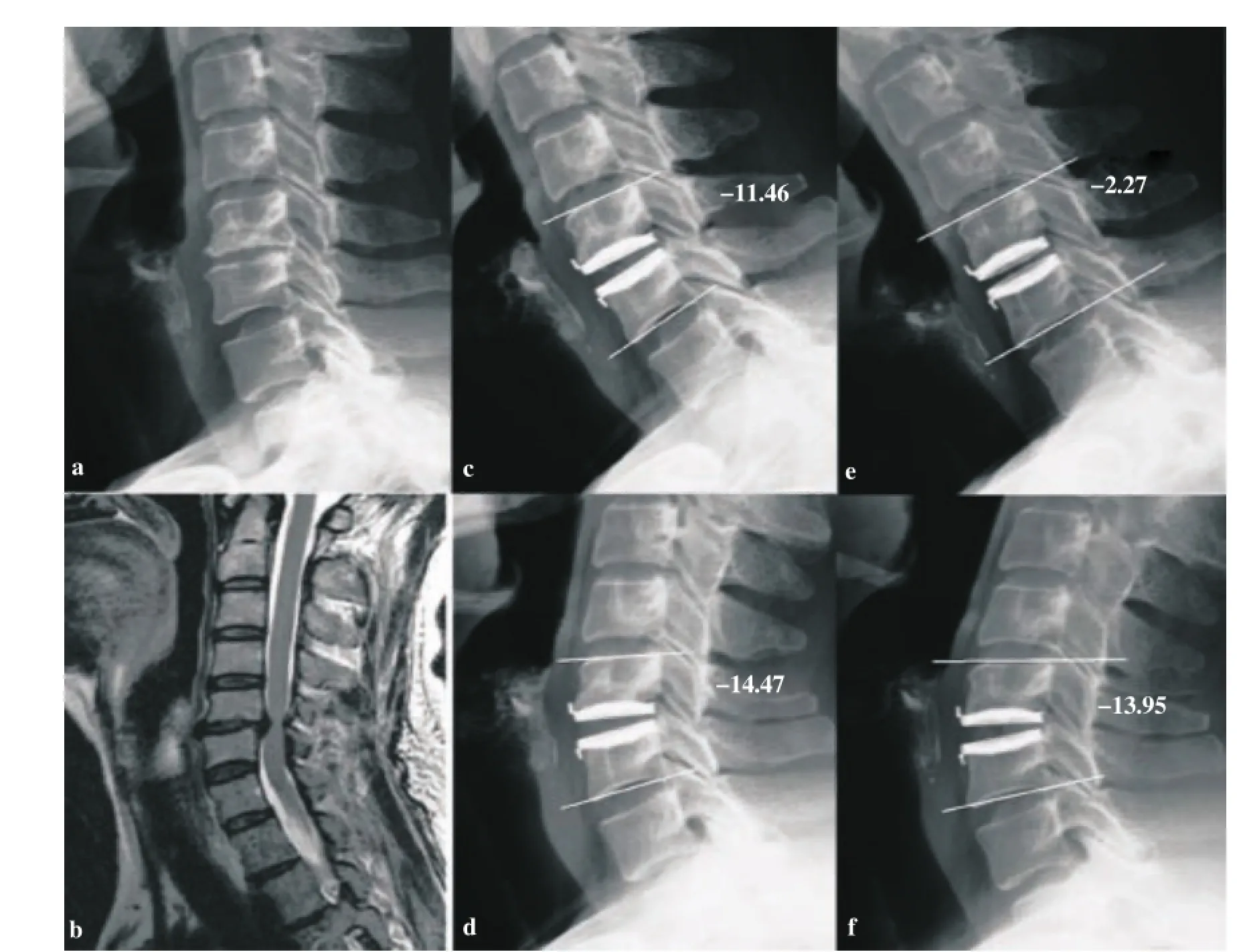
Figure 1. A 51-year-old woman had the osteophyte (a) and T2-weighted midsagittal image reveals a grade V cervical intervertebral disc degeneration at C5-6 (b). One-month postoperative lateral radiograph after replacement at C5-6 shows the range of motion was 3.0°calculated from flexion radiograph (c) and extension radiograph (d). After two years, the range of motion is 11.7°calculated from flexion (e) and extension (f). -: lordosis; +: kyphosis.
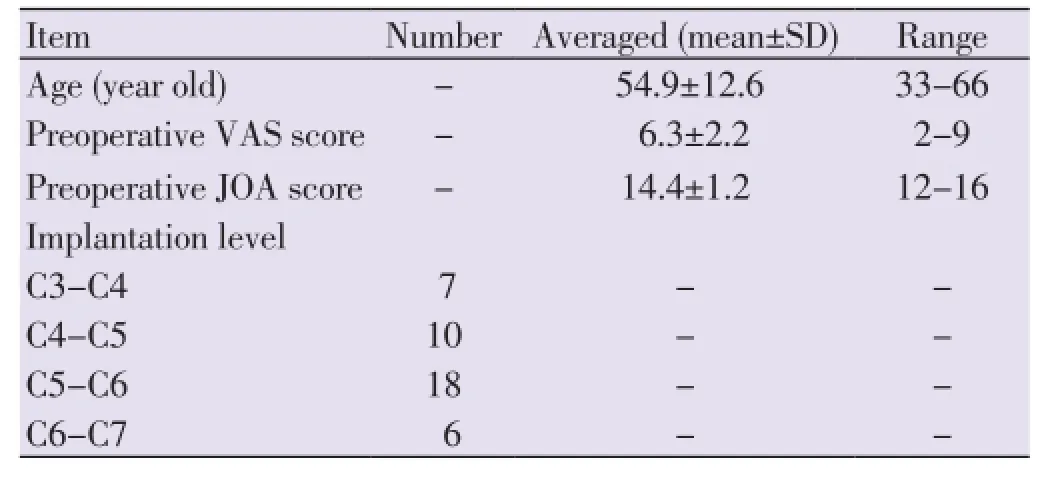
Table 1 Information of implantation levels of patients inquired.
2.2. Radiological analysis
All patients were preoperatively evaluated with static or dynamic cervical spine radiographs and magnetic resonance imaging. The magnetic resonance imaging was used to determine the radiculopathic or myelopathic origin. On T2-weighted midsagittal images, hypointense nucleus signal intensity, inhomogeneous gray to black nucleus structure and nucleus distinction loss and annulus, and disc height collapse were defined as grade V cervical intervertebral disc degeneration[16]. In this preoperative examination, A total of 12 patients with abnormal T2 cord signal met the clinical myelopathy criteria. Dynamic cervical spine radiographs were postoperatively obtained in one month, six months, 12 months, 18 months and 36 months. To analyze mobility at the proposed levels of replacement, angular range of motion was determined on the full flexion and extension radiographs. The angular range of motion was determined by drawing a line along the superior endplate of the cranial vertebrae and the inferior endplate of the caudal vertebrae. The difference between the angles on the 2 radiographs at each level was the range of motion. The mobility range of functional cervical spinal unit was defined as the difference in the Cobb’s angle between the full flexion and extension according to lateral radiographs. Pre- and postoperative variation of mobility ranges in follow-ups for all patients inquired were recorded for evaluation. Measurements of postoperative range of motion were performed by two experienced orthopaedic surgeons. Intraobserver variability was analyzed with independentt-test whileP<0.05 was considered statistically significant.
Studentt-test was used to compare differences between groups. Pairedt-test was used for assessing changes within groups from preoperative measures. APvalue of 0.05 was chosen as significant.
3. Results
3.1. Clinical findings
A total of 41 Bryan disc prostheses from 32 patients were evaluated. Clinical follow up was introduced with an average duration of 33.5 months (range 23 to 44 months). Significant change was found in averaged VAS score, that was significantly improved from 6.3±2.2 (range from 2 to 9) preoperatively to 1.3±1.2 (range from 0 to 4) postoperatively (P<0.001). Preoperative averaged JOA score was 14.4± 1.2 (range from 13 to 17) and was significantly improved (P<0.001) to 16.3±0.9 (range from 14 to 17) at the last followup (36 months). According to the Odom’s scale, 30 of 32 patients received excellent to good outcomes, and the other two patients performed fair outcomes in the last postoperative follow-up.
Both single level and multi-level groups showed improvement of their VAS and JOA scores at the last followup. Compared to preoperative scores, the VAS and JOA score at last follow-up for both single level and multi-level groups significantly decreased (P<0.05 as shown in Table 2). Between single level and multi-level groups, there is no significant difference at both the preoperative and the last follow-up. The detail clinical results of VAS, JOA score and Odom’s scale at each follow-up period are shown in Table 3.

Table 2 Clinical results with using VAS and JOA score.

Table 3 Clinical results of VAS, JOA score and Odom's scale at each followup patients period.
3.2. Range of motion
No significant intraobserver variability was found for measurements including in single level group (P=0.924),multi-level group (P=0.737), and in all evaluated samples (P=0.834). Postoperative angle measurements of the functional spinal unit at the implant level demonstrated motion of the device in flexion/extension. In consideration of mobility restoration, 34 of 41 (83%) implanted prostheses preserved sufficient mobility (more than 8 degrees) at the treated segment after the procedure in the last follow-up. Figures 1 and 2 show two of these cases representing the grade of degeneration, pre- and postoperative range of motion.
The mobility of treated segment in the early follow-up of one month postoperatively was comparatively restricted [average (8.2±3.4)°, range from 1.7° to 13.8°]. For the performance in the last follow-up evaluation of 36 months, the mobility was improved [average (9.9±3.2)°, range from 6° to 15.2°]. However, there were no statistical differences in angular range of motion of these two follow-ups (P=0.243). The angular range of motion was smaller than preoperative values in early follow-up evaluation but was restored to preoperative value at 12 months of the procedure (10.7±4.5)°. Distribution of comparative mobility during the period of follow-up was respectively illustrated in Figure 3.
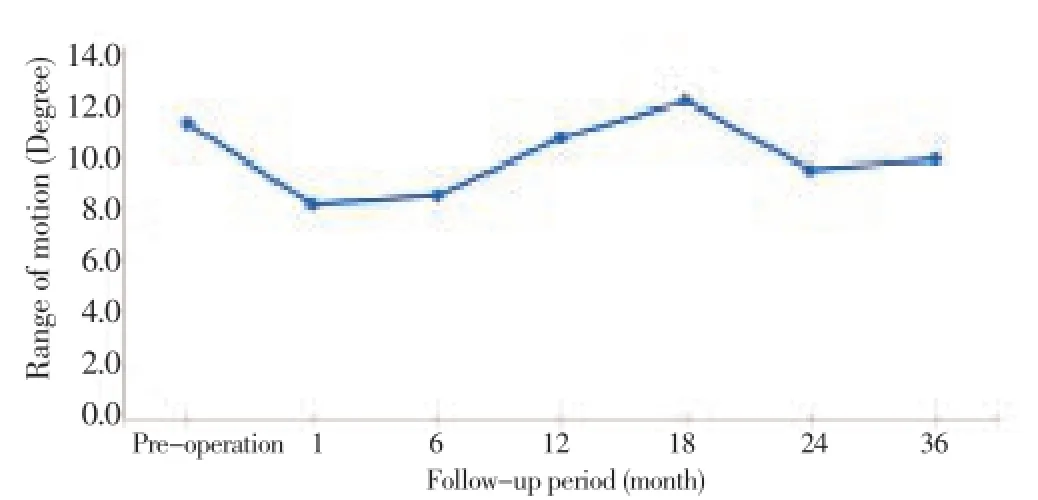
Figure 3. Distribution of comparative mobility during the periods of follow-up. Relative lower mobility in the early follow-ups; Mobility were restored in the last follow-ups.
At the 36 months follow-up, either in the single-level or multi-level group, the range of motion exhibited no statistic differences compared with preoperative results (Pvalue is 0.06 and 0.283 respectively).
3.3. Complications

Figure 2. One patient’s preoperative lateral radiograph shows marked osteophyte at C6-7 (a). T2-weighted midsagittal image shows grade V cervical intervertebral disc degeneration at C6-7 (b). One-month postoperative lateral radiograph after replacement at C6-7 with a range of motion of 0.1° calculated from flexion radiograph (c) and extension radiograph (d). After thirty months, the range of motion is 10.0° calculated from flexion (e) and extension (f).-: lordosis; +: kyphosis.
There was no prosthesis migration, subsidence, hematoma, neurological deficit, infections, or revision occurred in thesecases. The overall prevalence of heterotopic ossification in the 41 levels was 24% (Ten levels). There were one case of Class III heterotopic ossification and one case of Class IV heterotopic ossification. There are four cases having mild osteophyte increase (1.5 to 2 mm) in adjacent level after two years follow up based on the X-ray films. Nevertheless, one case of transient hoarseness was noted.
4. Discussion
Since 2002, Bryan discs have been implanted worldwide and have been the subject of clinical studies; the short- and intermediate-term clinical outcomes associated with Bryan disc have also been published[7-9,11]. Riewet al.stated that spinal motion maintained with cervical disc replacement did not appear to have an adverse effect in the setting of myelopathy up to 2 years after replacement[18]. To our knowledge and from article reviews, no study has described the clinical and radiographic outcomes according to the grade of disc degeneration. This study firstly reported the clinical and outcomes of surgical treatments of cervical disc replacement using Bryan cervical disc prostheses in patients with severe cervical disc narrowing.
The VAS and functional scores are useful indexes for evaluating clinical outcomes. In a prospective study with 2-year follow-up on 99 patients by Sassoet al[9], use of Bryan disc for replacement was favored other than anterior cervical discectomy and fusion for treatment of patient with single-level cervical disc disease; significant improvements of Neck Disability Index, neck pain and arm pain VAS scores were noted. Two-year follow-up results of Helleret al’s report indicated that cervical disc replacement achieved superior results compared with fusion in patients with persistently symptomatic, single-level cervical disc disease[19]. Yoonet al.reported their clinical outcome (averagely improved from 8.15 to 1.35) with follow-up duration of 11.8 months[12]. Their inclusion criteria included single or two level disease between C3-4 and C6-7. Amit and Dorward demonstrated that postoperative VAS score was significantly improved averagely from 8 to 4 with Bryan disc replacement from the 12-month clinical outcomes[20]. The indication of marked disc narrowing was excluded. In current study, 32 patients with 41 Bryan disc replacements for severe cervical disc narrowing were described. The majority of treated levels were C4-C5 and C5-C6. The similar performance on VAS score was improved from 7.22 to 2.11. Our results demonstrated the TDR on patients with severe cervical disc narrowing seemed to be safe and provided good preliminary functional results.
One of the primary goals of cervical disc replacement is to reproduce normal kinematics after implantation. Our investigations noted preservation of angular motion at the target level at 36 months. This statistically significant finding mirrors the findings of other investigators. Duggalet al.have demonstrated preservation of motion in Bryan-treated spinal segments (from preoperative 10.1° to postoperative 7.8° for up to 24 months)[21]. Sassoet al.reported relative lower mobility (6.43°) in preoperative compared with their final follow-up evaluation using Bryan disc arthroplasty (7.95° at 24 months) [9]. According to Goffinet al.’s clinical cases with Bryan disc replacement, average of range of motion at for one level at two year was 9.0°[8]. Their indication intended for use is DDD of the cervical spine at any one level or two adjacent levels between C3-4 and C6-7. In comparison of postoperative mobility of treated segments, restricted mobility was observed in early follow-up evaluation (8.2° at one month). Probably, in early stage of postoperative recovery, it was under the period of adaptation of spinal structure. According to Panjabi’s theory of spinal stabilizing system, intervertebral disc as a component of passive subsystem was out of function and replaced[22]. Several months were spent for mechanisms of adaptation and enhancement of spinal stabilizing capacity to restore the function of treated segment. With follow-ups over 12 months, mobility of treated segments were preserved (10.7° at 12 months), and no significant adjacent level degeneration was observed during the whole period.
Several postoperative complications for treatment with Bryan disc have been reported. Pickettet al.demonstrated early and late complications (included neurological symptom, heterotopic ossification, implant migration, prosthesis failure,etc.) in mechanical and physical conditions; the complication rate was 6.2% in average per treated level[23]. In this study, no patient required revision surgery, and no prosthesis subsidence or migration has been encountered. There is 24% incidence rate of heterotopic ossification observed in this study. The rate is higher than Leunget al.’s study (17.8%)[24]. According to their conclusion, male gender was detected to be associated with development of heterotopic ossification. In this follow up study, patient number with male gender is more than female.
In addition, some degenerative cervical diseases encompass more than one level. Previous literatures concluded that bi-level or tri-level disc replacement is feasible and safe and the patients had good outcome and restored range of motion in the early and immediate postoperative period[8,25]. Some patients underwent multilevel arthroplasties (7/32 for bi-level and 1/32 for trilevel arthroplasties) in current study. Effects of number of treatment segments were analyzed. As compared to preoperative clinical functional data, both single level and multi-level groups showed improvement of their VAS and JOA results at the 36 months follow-up. Although the cases for multi-level disc replacement in the treatment of DDD are less in current study, it is believed that the clinical results of the cervical artificial disc will be improved for multi-level applications with severe cervical disc narrowing. Another finding is that mobility of all inserted Bryan discs in single-, two- or tri-level introduced seemed no significant difference appeared in each implanted segment. Further study should carefully take these conditions into considerations to have a whole understanding for single- or multi-level replacement.
Rotational center of the motion unit is not calculated in this study. Trajectory for the instant rotational center isimportant in evaluating the motional quality of human spine. However, current study focused on the maximal range of flexion/extension activity. Only single center of rotation can be defined for each flexion/extension activity, which may not provide sufficient information of motional quality (i.e.trajectory of instant rotational center). According to the special mechanism design, the rotational center of Bryan disc would change more significantly in flexion-extension than other ball-and-socket type devices. Consequently, Bryan disc may perform better mobility than ball-andsocket type products (i.e.ProDisc-C or Prestige) for the patient with severe cervical disc narrowing. The unconstrained, mobile and more degrees of freedom may be an adequate design for severe cervical disc narrowing.
In conclusions, referring to the clinical outcomes in current study, application of Bryan disc for cervical disc replacement is effective in treatment of severe cervical disc narrowing. Treatments with the disc could preserve mobility in flexion/extension activities in current mediumterm follow-ups. Long-term follow-up and retrospective evaluation will be required to have a whole understanding for the mechanism of cervical disc replacement.
Conflict of interest statement
The authors report no conflict of interest.
[1] Bohlman HH, Emery SE, Goodfellow DB, Jones PK. Robinson anterior cervical discectomy and arthrodesis for cervical radiculopathy. Long-term follow-up of one hundred and twentytwo patients. J Bone Joint Surg Am 1993; 75: 1298-1307.
[2] Kao FC, Niu CC, Chen LH, Lai PL, Chen WJ. Maintenance of interbody space in one- and two-level anterior cervical interbody fusion: comparison of the effectiveness of autograft, allograft, and cage. Clin Orthop Relat Res 2005; (430): 108-116.
[3] Matgé G. Cervical cage fusion with 5 different implants: 250 cases. Acta Neurochir 2002; 144: 539-549.
[4] Eck JC, Humphreys SC, Lim TH, Jeong ST, Kim JG, Hodges SD, et al. Biomechanical study on the effect of cervical spine fusion on adjacent-level intradiscal pressure and segmental motion. Spine 2002; 27: 2431-2434.
[5] Goffin J, Geusens E, Vantomme N, Quintens E, Waerzeggers Y, Depreitere B, et al. Long-term follow-up after interbody fusion of the cervical spine. J Spinal Disord Tech 2004; 17: 79-85.
[6] Matsunaga S, Kabayama S, Yamamoto T, Yone K, Sakou T, Nakanishi K. Strain on intervertebral discs after anterior cervical decompression and fusion. Spine 1999; 24: 670-675.
[7] Goffin J, Casey A, Kehr P, Liebig K, Lind B, Logroscino C, et al. Preliminary clinical experience with the Bryan cervical disc prosthesis. Neurosurgery 2002; 51: 845-847.
[8] Goffin J, Van Calenbergh F, van Loon J, Casey A, Kehr P, Liebig K, et al. Intermediate follow-up after treatment of degenerative disc disease with the Bryan cervical disc prosthesis: single-level and bi-level. Spine 2003; 28: 2673-2678.
[9] Sasso RC, Smucker JD, Hacker JD, Heller JG. Artificial disc versus fusion: a prospective, randomized study with 2-year follow-up on 99 patients. Spine 2007; 32: 2933-2940.
[10] Sekhon LHS. Cervical arthroplasty in the management of spondylotic myelopathy: 18-month results. Neurosurgical Focus 2004; 17: E8.
[11] Sasso RC, Best NM, Metcalf NH, Anderson PA. Motion analysis of bryan cervical disc arthroplasty versus anterior discectomy and fusion: results from a prospective, randomized, multicenter, clinical trial. J Spinal Disord Tech 2008; 21: 393-399.
[12] Yoon DH, Yi S, Shin HC, Kim KN, Kim SH. Clinical and radiological results following cervical arthroplasty. Acta Neurochir (Wien) 2006; 148: 943-950.
[13] Dmitriev AE, Cunningham BW, Hu N, Sell G, Vigna F, McAfee PC. Adjacent level intradiscal pressure and segmental kinematics following a cervical total disc arthroplasty: an in vitro human cadaveric model. Spine 2005; 30: 1165-1172.
[14] Axelsson P, Karlsson BS. Intervertebral mobility in the progressive degenerative process. A radiostereometric analysis. Eur Spine J 2004; 13: 567-572.
[15] Dai L. Disc degeneration and cervical instability. Correlation of magnetic resonance imaging with radiography. Spine 1998; 23: 1734-1738.
[16] Miyazaki M, Hong SW, Yoon SH, Zou J, Tow B, Alanay A, et al. Kinematic analysis of the relationship between the grade of disc degeneration and motion unit of the cervical spine. Spine 2008; 33: 187-193.
[17] Odom GL, Finney W, Woodhall B. Cervical disk lesions. J Am Med Assoc 1958; 166: 23-28.
[18] Riew KD, Buchowski JM, Sasso R, Zdeblick T, Metcalf NH, Anderson PA. Cervical disc arthroplasty compared with arthrodesis for the treatment of myelopathy. J Bone Joint Surg Am 2008; 90: 2354-2364.
[19] Heller JG, Sasso RC, Papadopoulos SM, Anderson PA, Fessler RG, Hacker RJ, et al. Comparison of Bryan cervical disc arthroplasty with anterior cervical decompression and fusion: clinical and radiographic results of a randomized, controlled, clinical trial. Spine 2009; 34: 101-107.
[20] Amit A, Dorward N. Bryan cervical disc prosthesis: 12-month clinical outcome. Br J Neurosurg 2007; 21: 478-484.
[21] Duggal N, Pickett GE, Mitsis DK, Keller JL. Early clinical and biomechanical results following cervical arthroplasty. Neurosurg Focus 2004; 17: E9.
[22] Panjabi MM. The stabilizing system of the spine. Part I. Function, dysfunction, adaptation, and enhancement. J Spinal Disord 1992; 5: 383-389.
[23] Pickett GE, Sekhon LH, Sears WR, Duggal N. Complications with cervical arthroplasty. J Neurosurg Spine 2006; 4: 98-105.
[24] Leung C, Casey AT, Goffin J, Kehr P, Liebig K, Lind B, et al. Clinical significance of heterotopic ossification in cervical disc replacement: a prospective multicenter clinical trial.Neurosurgery 2005; 57: 759-763.
[25] Yang S, Wu X, Hu Y, Li J, Liu G, Xu W, et al. Early and intermediate follow-up results after treatment of degenerative disc disease with the Bryan cervical disc prosthesis: singleand multiple-level. Spine 2008; 33: E371-377.
ment heading
10.1016/S2221-6189(14)60063-9
*Corresponding author: Dr. Chien-Ming Chao, Department of Intensive Care Medicine, Chi Mei Medical Center, Liouying, Tainan, Taiwan.
Tel: +886-6-6226999
Fax: +886-6-6226999#77610
E-mail: ccm870958@yahoo.com.tw
Bryan disc
Severe cervical disc narrowing
Degenerative cervical disc disease
 Journal of Acute Disease2014年4期
Journal of Acute Disease2014年4期
- Journal of Acute Disease的其它文章
- Acute and sub-acute toxicity study of Clerodendrum inerme, Jasminum mesnyi Hance and Callistemon citrinus
- Time-critical AMI Detection: A novel and fast technique using the 12-lead ECG
- Epidemiological survey on scorpionism in Gotvand County, Southwestern Iran: an analysis of 1 067 patients
- The acute effect of the antioxidant drug “U-74389G” on red blood cells levels during hypoxia reoxygenation injury in rats
- Successful treatment of lower urinary tract obstruction with peritonealamniotic and vesicoamniotic shunting
- Simvastatin-induced Toxic Epidermal Necrolysis
