A new approach for Roux-en-Y reconstruction after pancreaticoduodenectomy
Meng Xu, Min Wang, Feng Zhu, Rui Tian, Cheng-Jian Shi, Xin Wang, Ming Shen and Ren-Yi Qin
Wuhan, China
A new approach for Roux-en-Y reconstruction after pancreaticoduodenectomy
Meng Xu, Min Wang, Feng Zhu, Rui Tian, Cheng-Jian Shi, Xin Wang, Ming Shen and Ren-Yi Qin
Wuhan, China
BACKGROUND:Postoperative pancreatic fistula remains the most common complication of pancreaticoduodenectomy (PD) and is potentially lethal. It contributes significantly to prolonged hospitalization and mortality. In this study, we introduced a new technical approach, a modified Roux-en-Y reconstruction and evaluated its safety and feasibility.
METHODS:We retrospectively reviewed the patients who had undergone PD with the modified Roux-en-Y reconstructive technique for periampullary malignancies from January 2011 to June 2012. The data on complications, hospital stay and outcomes after the modified Roux-en-Y reconstruction were analyzed.
RESULTS:The reconstruction was performed in 171 patients, of whom 92 received pancreaticogastrostomy and 79 received pancreaticojejunostomy. The median duration of surgery was 4.0 hours (range 3.1-6.9) in all patients, and the median blood loss was 530 mL (range 200-2000). Sixty-nine patients were subjected to transfusions, with a median transfusion volume of 430 mL (range 200-1400). The median hospital stay of the patients was 14 days (range 11-38). Their operative mortality was zero and overall morbidity was 18.1% (31 patients). Only four patients (2.3%) developed pancreatic fistulas (grade A fistulas in two patients and grade B in two patients); no patients developed grade C fistula. None of the patients developed bile reflux gastritis.
CONCLUSIONS:The modified Roux-en-Y reconstruction, which isolates biliary anastomosis from pancreatic, gastric or jejunalanastomosis, is a safe, reliable, and favorable technique. But it needs further investigation in randomized controlled trials.
(Hepatobiliary Pancreat Dis Int 2014;13:649-653)
pancreaticoduodenectomy;
Roux-en-Y reconstruction;
postoperative complications;
pancreatic fistula;
periampullary malignancy
Introduction
Pancreaticoduodenectomy (PD) is the primary mean for the treatment of periampullary cancer.[1-3]With advances in diagnostic imaging and surgical techniques, the mortality rate of periampullary cancer has dropped dramatically over the past decade, but its morbidity rate remains high.[4,5]Leakage due to pancreatic anastomosis is the most important cause of morbidity and prolonged hospitalization.[6-8]The risk factors for postoperative pancreatic fistula (POPF) include a soft pancreas, a small pancreatic duct, and surgeon's experience.[9,10]To prevent the formation of pancreatic fistula after PD, studies were carried out to modify pancreaticoenteric reconstruction by using pancreaticogastrostomy or pancreaticojejunostomy, invagination or duct-to-mucosa techniques, end-toend or end-to-side apposition, stents, and fibrin glue or omentum.[11-18]However, no procedure has been universally accepted as the safest and least prone to anastomotic failure.
The use of a separate Roux loop was first described in 1976, and it was intended to reduce the activation of pancreatic enzymes.[19]Roux-en-Y reconstruction after PD can reduce the pancreatic anastomotic leakrelated morbidity and mortality.[19-27]It is recognized that isolating pancreatic anastomosis from biliary or gastric anastomosis prevents the activation of pancreaticenzyme precursors by low gastric pH or enterokinase. Even if this anastomotic reconstruction fails, the resulting fistula is benign.[19,20,23,24]
In this study, we described the use of a modified Rouxen-Y reconstruction, which isolates biliary anastomosis from pancreatic, gastric or jejunal anastomosis. This report summarizes the preliminary results of this method used in patients with periampullary malignancies at a large institution.
Methods
Patients
We recruited 171 patients with resectable periampullary tumors who had undergone PD at our department from January 2011 to June 2012. Preoperative biliary drainage and concomitant surgical procedures such as colonic resection and portal vein resection or reconstruction were performed. Patients who had chronic pancreatitis without suspected malignancy, pancreatic trauma, or complications of endoscopic retrograde cholangiopancreatography and those who had the pylorus preserved after PD were excluded. Patients' age, gender, body mass index (BMI), and symptoms were prospectively recorded. The following data were collected for each patient: operation time (from incision to skin closure), estimated blood loss, volume of blood transfusion, length of hospital stay, pathologic diagnosis, POPF, delayed gastric emptying (DGE) or bile reflux gastritis, and requirement for a postoperative interventional radiology procedure. The study was approved by the medical ethics committee of our hospital.
Surgical procedures
PD was performed by a group of surgeons through radical resection of the uncinate process and the pylorus.[28]The extent of lymph node dissection included stations 1, 3, 4, 5, 6, 7, 8, 9, 12 (h, a, p, b, and c), 13, 14, 15, and 16a2.
En blocresection was made of the gallbladder, part of the common hepatic duct, common bile duct, gastric antrum, entire duodenum, pancreatic head, and its uncinate process, neck and part of the pancreatic body, and regional lymph nodes. End-to-side pancreaticogastrostomy (with two continuous hemstitch sutures) or end-to-end pancreaticojejunostomy (with transpancreatic interlocking mattress sutures) was dependent on the texture of the pancreas remnant as described.[29,30]Soft and non-fibrotic pancreatic tissue was suitable for pancreaticogastrostomy, while hard and fibrotic pancreatic tissue was an indication for pancreaticojejunostomy.
A side-to-end anastomosis was made between the posterior wall of the stomach and the end of the jejunum after pancreaticogastrostomy, while a sideto-side anastomosis was made between the stomach and jejunum 10 cm distal to the pancreatic anastomosis after pancreaticojejunostomy. The two anastomoses were performed using a gastrointestinal circular stapler (Jiangsu Brightness Medical Devices Co. Ltd., Changzhou, China).
The jejunum was transected 40-50 cm distal to the gastrojejunal anastomosis, and the distal loop was anastomosed end-to-side with the common hepatic duct using one layer of interrupted 4-0 polydioxanone suture via an incision in the transverse mesocolon. Approximately 40-50 cm distal to the hepaticojejunal anastomosis, a Roux-en-Y reconstruction of the jejunum was performed by anastomosing the two jejunal segments using a circular stapler (Fig.).
Then two drainage tubes were placed, one near the pancreaticogastric or pancreaticojejunal anastomosis and the other near the hepaticojejunal anastomosis. The drainage tubes were left in place for at least seven days after surgery and were removed when less than 30 mL of clear fluid was drained per day. Patients were treated with octreotide for 5 days after operation. The proton pump inhibitor omeprazole was given at a dosage of 20 mg, twice daily for 7 days. Total parenteral nutrition was started on the first day after surgery and replaced gradually by oral intake which begun immediately after the nasogastric tubes were removed if less than 100 mL of gastric juice was drained daily. Patients were discharged when they were able to resume approximately half of their normal intake. They were also discharged with a nasojejunic nutrition tube once the pancreatic leakage was well controlled.
Definition of outcome measures
The definition of POPF was based on the International Study Group on Pancreatic Fistula (ISGPF) criteria: a drain output of any measurable volume of fluid on orafter the third postoperative day, with a fluid amylase content three times that of serum amylase. The ISGPF grading system for POPF was used.[31]
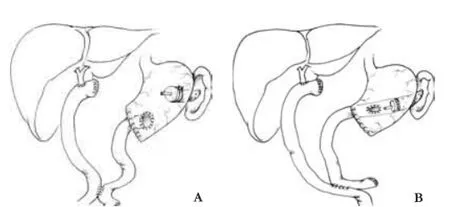
Fig.Diagrams of modified Roux-en-Y reconstruction after pancreaticogastrostomy (A) and pancreaticojejunostomy (B).
Endoscopy was performed if bile reflux gastritis was suspected. Other complications such as postpancreatectomy hemorrhage (PPH), DGE, and biliary fistula were defined and classified according to the International Study Group of Pancreatic Surgery (ISGPS).[6]
Statistical analysis
Data were analyzed using SPSS version 13.0 for Windows (SPSS Inc., Chicago, IL, USA). The mean, median, range, and frequency were analyzed as descriptive statistics.
Results
In the 171 consecutive patients with periampullary tumor (80 men and 91 women; aged 33-77 years, average 55.7), jaundice (n=117, 68.4%), abdominal pain (n=81, 47.4%), and weight loss (n=124, 72.5%) were the most common complaints (Table 1).
In all the patients, 92 patients had received pancreaticogastrostomy and 79 had undergone pancreaticojejunostomy. The mean operative time was 4.0 hours (range 3.1-6.9)and the median blood loss was 530 mL (range 200-2000). Sixty-nine patients required blood transfusions, and the median transfusion volume of blood was 430 mL (range 200-1400). The median hospital stay of the patients was 14 days (range 11-38). Malignant periampullary tumors were confirmed histologically in this series of patients: ductal cell carcinoma at the head of the pancreas in 49 patients, distal common bile duct carcinoma in 45, adenocarcinoma of Vater's ampulla in 39, adenocarcinoma of the duodenum in 36, and intraductal papillary mucinous neoplasm (IPMN) in 2 (Table 1).
There was no operative mortality or reoperations. Thirty-one patients (18.1%) had postoperative complications including POPF (4, 2.3%), DGE (6, 3.5%), biliary fistula (3, 1.8%), upper gastrointestinal bleeding (4, 2.3%), abdominal abscess (4, 2.3%; 2 caused by POPF), pulmonary infection (2, 1.1%), wound infection (3, 1.8%), arrhythmia or myocardial infarction (3, 1.8%), and urinary tract infection (2, 1.1%) (Table 2). The DGE resolved after conservative treatment for 3-4 weeks. None of the patients developed bile reflux gastritis. Of the four POPF cases, two were grade A and were treated conservatively. The other two were grade B and required percutaneous drainage under ultrasonographic guidance after the development of abdominal abscesses. No patients developed grade C fistula.

Table 1.Demographic characteristics and surgical outcomes of the patients
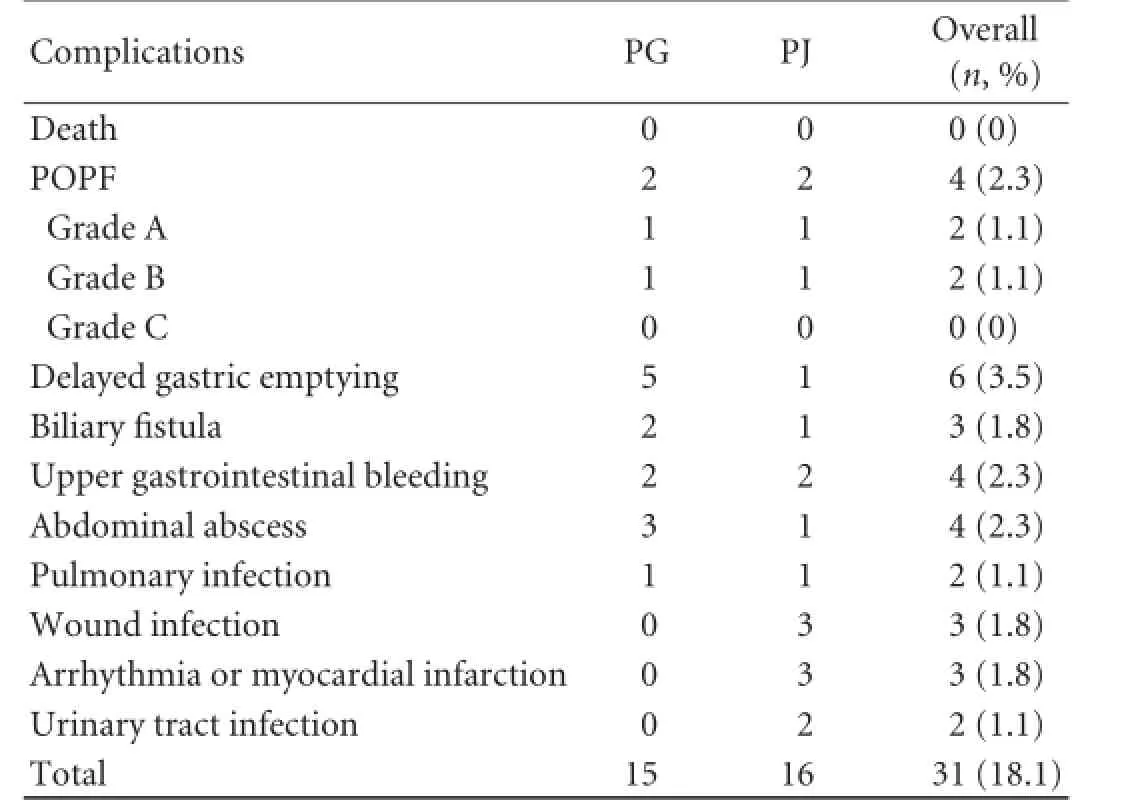
Table 2.Postoperative complications
Discussion
PD is the standard treatment for patients with malignant or benign disease of the pancreatic head or periampullary region.[32]Over the years, advances in perioperativemanagement and surgical techniques have made this a safe procedure, with an increasing number of centers reporting an operative mortality below 5%.[4,33]However, the reported morbidity rate associated with PD ranges from 25% to 65%.[34-36]Five to twenty percent of the patients are complicated with POPF which causes a significant morbidity and mortality.[6,37]Pharmacological and surgical methods for preventing pancreatic fistula have been extensively studied over the last two decades. However, there is controversy over the efficacy of these measures in reducing the pancreatic fistula rate.
In various techniques for the reconstruction of the alimentary tract after PD, Child's, Whipple's, and Cattel's procedures are the most common.[38,39]In all of these procedures, intestinal loop is used for biliary or pancreatic anastomosis. As a result, only a short segment of the intestine separates the two anastomoses, facilitating the combined outflow of biliary and pancreatic juice. If the disruption of either of the anastomoses occurs, the secretion drained through the resultant fistula impairs healing and causes damage to the surrounding tissue because of the active pancreatic juices and powerful digestive enzymes in the secretion.[19,26]This complication is similar to that of a duodenal fistula and is difficult to treat.
Roux-en-Y reconstruction after PD was popularized by Machado et al,[19]who isolated pancreaticojejunal anastomosis from the biliary anastomosis by a Rouxen-Y limb of the jejunum, a technique which seems to have a physiological rationale. A transient pancreatic fistula developed in two patients, but there was no mortality in 15 patients when this procedure was performed. This procedure can prevent the activation of enzyme precursors in pancreatic juice, so that even if the pancreatic anastomosis fails, the related morbidity or mortality is minimized. Funovics et al[20]found that the mortality of such patients after this procedure was reduced when pancreatic anastomosis was isolated on a separate Roux-en-Y jejunal loop or when the pancreatic duct was left open—not anastomosed to the gut, but drained externally. More recently, several case studies have reported a reduction of the pancreatic fistula rate and the mortality associated with pancreatic anastomotic leakage when using this technique as compared with the conventional procedures.[21-27]
In this study, we modified Roux-en-Y reconstruction by isolating the biliary anastomosis from the pancreatic and gastric or jejunal anastomosis after PD. Our method is more advantageous than traditional reconstructive procedures for the reconstruction of the alimentary tract. First, this technique reduces the morbidity and mortality resulted from leakage of either anastomoses because of the separation of pancreatic anastomosis from the biliary one. Second, separating the two anastomoses decreases the incidence of bile reflux gastritis. For example, none of the patients developed bile reflux gastritis. Finally, anastomosing the proximal jejunum to the remnant of the pancreas or stomach maximizes the digestive and absorptive capacity.
In conclusion, the modified Roux-en-Y reconstruction, which isolates biliary anastomosis from pancreatic, gastric or jejunal anastomosis, is a safe, feasible, and efficient procedure for the reconstruction of the alimentary tract. However, larger prospective randomized studies are warranted to validate this technique.
Contributors:QRY proposed the study and performed the operations. XM and WM performed research and wrote the first draft. XM and WM contributed equally to this work. TR and SCJ collected and analyzed the data. ZF, WX and SM contributed to the interpretation of the study and to further drafts. QRY is the guarantor.
Funding:This study was supported by grants from the National Natural Science Foundation of China (81272659, 81101621 and 81372353).
Ethical approval:The study was approved by the medical ethics committee of our hospital.
Competing interest:No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
1 van Heek NT, Kuhlmann KF, Scholten RJ, de Castro SM, Busch OR, van Gulik TM, et al. Hospital volume and mortality after pancreatic resection: a systematic review and an evaluation of intervention in the Netherlands. Ann Surg 2005;242:781-790.
2 Samra JS, Bachmann RA, Choi J, Gill A, Neale M, Puttaswamy V, et al. One hundred and seventy-eight consecutive pancreatoduodenectomies without mortality: role of the multidisciplinary approach. Hepatobiliary Pancreat Dis Int 2011;10:415-421.
3 Cameron JL, Riall TS, Coleman J, Belcher KA. One thousand consecutive pancreaticoduodenectomies. Ann Surg 2006;244: 10-15.
4 Govindarajan A, Tan JC, Baxter NN, Coburn NG, Law CH. Variations in surgical treatment and outcomes of patients with pancreatic cancer: a population-based study. Ann Surg Oncol 2008;15:175-185.
5 Shrikhande SV, Qureshi SS, Rajneesh N, Shukla PJ. Pancreatic anastomoses after pancreaticoduodenectomy: do we need further studies? World J Surg 2005;29:1642-1649.
6 Butturini G, Marcucci S, Molinari E, Mascetta G, Landoni L, Crippa S, et al. Complications after pancreaticoduodenectomy: the problem of current definitions. J Hepatobiliary Pancreat Surg 2006;13:207-211.
7 Callery MP, Pratt WB, Vollmer CM Jr. Prevention and management of pancreatic fistula. J Gastrointest Surg 2009;13:163-173.
8 Lai EC, Lau SH, Lau WY. Measures to prevent pancreatic fistula after pancreatoduodenectomy: a comprehensive review. Arch Surg 2009;144:1074-1080.
9 Lermite E, Pessaux P, Brehant O, Teyssedou C, Pelletier I, Etienne S, et al. Risk factors of pancreatic fistula and delayed gastric emptying after pancreaticoduodenectomy with pancreaticogastrostomy. J Am Coll Surg 2007;204:588-596.
10 Adams DB. The pancreatic anastomosis: the danger of a leak, which anastomotic technique is better? J Gastrointest Surg 2009;13:1182-1183.
11 Marcus SG, Cohen H, Ranson JH. Optimal management of the pancreatic remnant after pancreaticoduodenectomy. Ann Surg 1995;221:635-648.
12 Yeo CJ, Cameron JL, Maher MM, Sauter PK, Zahurak ML, Talamini MA, et al. A prospective randomized trial of pancreaticogastrostomy versus pancreaticojejunostomy after pancreaticoduodenectomy. Ann Surg 1995;222:580-592.
13 Nakanishi Y, Ohara M, Noguchi M, Domen H, Komuro K, Hirano S. New invagination procedure for pancreaticojejunostomy using only four sutures. World J Surg 2012;36: 892-897.
14 Zhang JL, Xiao ZY, Lai DM, Sun J, He CC, Zhang YF, et al. Comparison of duct-to-mucosa and end-to-side pancreaticojejunostomy reconstruction following pancreaticoduodenectomy. Hepatogastroenterology 2013;60: 176-179.
15 Roder JD, Stein HJ, Böttcher KA, Busch R, Heidecke CD, Siewert JR. Stented versus nonstented pancreaticojejunostomy after pancreatoduodenectomy: a prospective study. Ann Surg 1999;229:41-48.
16 Satoi S, Toyokawa H, Yanagimoto H, Yamamoto T, Hirooka S, Yui R, et al. Reinforcement of pancreticojejunostomy using polyglycolic acid mesh and fibrin glue sealant. Pancreas 2011;40:16-20.
17 Chirletti P, Peparini N, Caronna R, Fanello G, Delogu G, Meniconi RL. Roux-en-Y end-to-end and end-to-side double pancreaticojejunostomy: application of the reconstructive method of the Beger procedure to central pancreatectomy. Langenbecks Arch Surg 2010;395:89-93.
18 Tani M, Kawai M, Hirono S, Hatori T, Imaizumi T, Nakao A, et al. Use of omentum or falciform ligament does not decrease complications after pancreaticoduodenectomy: nationwide survey of the Japanese Society of Pancreatic Surgery. Surgery 2012;151:183-191.
19 Machado MC, da Cunha JE, Bacchella T, Bove P. A modified technique for the reconstruction of the alimentary tract after pancreatoduodenectomy. Surg Gynecol Obstet 1976;143:271-272.
20 Funovics JM, Zöch G, Wenzl E, Schulz F. Progress in reconstruction after resection of the head of the pancreas. Surg Gynecol Obstet 1987;164:545-548.
21 Lygidakis NJ, Brummelkamp WH. A new approach for the reconstruction of continuity of the alimentary tract after pancreaticoduodenotomy. Surg Gynecol Obstet 1985;160:453-458.
22 Kingsnorth AN. Duct to mucosa isolated Roux loop pancreaticojejunostomy as an improved anastomosis after resection of the pancreas. Surg Gynecol Obstet 1989;169:451-453.
23 Albertson DA. Pancreaticoduodenectomy with reconstruction by Roux-en-Y pancreaticojejunostomy: no operative mortality in a series of 25 cases. South Med J 1994;87:197-201.
24 Kingsnorth AN. Safety and function of isolated Roux loop pancreaticojejunostomy after Whipple's pancreaticoduodenectomy. Ann R Coll Surg Engl 1994;76:175-179.
25 Papadimitriou JD, Fotopoulos AC, Smyrniotis B, Prahalias AA, Kostopanagiotou G, Papadimitriou LJ. Subtotal pancreatoduodenectomy: use of a defunctionalized loop for pancreatic stump drainage. Arch Surg 1999;134:135-139.
26 Khan AW, Agarwal AK, Davidson BR. Isolated Roux Loop duct-to-mucosa pancreaticojejunostomy avoids pancreatic leaks in pancreaticoduodenectomy. Dig Surg 2002;19:199-204.
27 Ma YG, Li XS, Chen H, Wu MC. Pancreaticoduodenectomy with Roux-Y anastomosis in reconstructing the digestive tract: report of 26 patients. Hepatobiliary Pancreat Dis Int 2002;1:611-613.
28 Qin RY, Cao XY, Zhu F, Wang X. A new method for integrated radical resection of uncinate process of the pancreas: a report of 306 cases. Zhonghua Wai Ke Za Zhi 2010;48:1379-1382.
29 Zhu F, Wang M, Wang X, Tian R, Shi C, Xu M, et al. Modified technique of pancreaticogastrostomy for soft pancreas with two continuous hemstitch sutures: a single-center prospective study. J Gastrointest Surg 2013;17:1306-1311.
30 Wang M, Zhu F, Wang X, Tian R, Shi C, Shen M, et al. A modified technique of end-to-end pancreaticojejunostomy with transpancreatic interlocking mattress sutures. J Surg Oncol 2013;107:783-788.
31 Bassi C, Dervenis C, Butturini G, Fingerhut A, Yeo C, Izbicki J, et al. Postoperative pancreatic fistula: an international study group (ISGPF) definition. Surgery 2005;138:8-13.
32 Cascinu S, Falconi M, Valentini V, Jelic S; ESMO Guidelines Working Group. Pancreatic cancer: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol 2010;21:v55-58.
33 Yeo CJ, Cameron JL, Sohn TA, Lillemoe KD, Pitt HA, Talamini MA, et al. Six hundred fifty consecutive pancreatico duodenectomies in the 1990s: pathology, complications, and outcomes. Ann Surg 1997;226:248-260.
34 Yeo CJ. The Whipple procedure in the 1990s. Adv Surg 1999; 32:271-303.
35 Grobmyer SR, Pieracci FM, Allen PJ, Brennan MF, Jaques DP. Defining morbidity after pancreaticoduodenectomy: use of a prospective complication grading system. J Am Coll Surg 2007;204:356-364.
36 Balcom JH 4th, Rattner DW, Warshaw AL, Chang Y, Fernandezdel Castillo C. Ten-year experience with 733 pancreatic resections: changing indications, older patients, and decreasing length of hospitalization. Arch Surg 2001;136: 391-398.
37 Grobmyer SR, Rivadeneira DE, Goodman CA, Mackrell P, Lieberman MD, Daly JM. Pancreatic anastomotic failure after pancreaticoduodenectomy. Am J Surg 2000;180:117-120.
38 Doi R, Fujimoto K, Kobayashi H, Imamura M Impact of reconstruction methods on outcome of pancreatoduodenectomy in pancreatic cancer patients. World J Surg 2005;29:500-504.
39 Fragulidis GP, Arkadopoulos N, Vassiliou I, Marinis A, Theodosopoulos T, Stafyla V, et al. Pancreatic leakage after pancreaticoduodenectomy: the impact of the isolated jejunal loop length and anastomotic technique of the pancreatic stump. Pancreas 2009;38:e177-182.
Received April 15, 2013
Accepted after revision October 22, 2013
Author Affiliations: Department of Pancreatic-Biliary Surgery, Tongji Hospital, Tongji Medical College, Huazhong University of Science and Technology, Wuhan 430030, China (Xu M, Wang M, Zhu F, Tian R, Shi CJ, Wang X, Shen M and Qin RY)
Ren-Yi Qin, MD, Department of Pancreatic-Biliary Surgery, Tongji Hospital, Tongji Medical College, Huazhong University of Science and Technology, Wuhan 430030, China (Tel/Fax: +86-27-83665294; Email: ryqin@tjh.tjmu.edu.cn)
© 2014, Hepatobiliary Pancreat Dis Int. All rights reserved.
10.1016/S1499-3872(14)60047-3
Published online March 27, 2014.
 Hepatobiliary & Pancreatic Diseases International2014年6期
Hepatobiliary & Pancreatic Diseases International2014年6期
- Hepatobiliary & Pancreatic Diseases International的其它文章
- Diagnosis and treatment of autoimmune pancreatitis: experience with 100 patients
- Surgical treatment of fibrolamellar hepatocellular carcinoma: an underestimated malignant tumor?
- Comparison of brush and basket cytology in differential diagnosis of bile duct stricture at endoscopic retrograde cholangiopancreatography
- A selective approach to the surgical management of periampullary cancer patients and its outcome
- Effect of the number of positive lymph nodes and lymph node ratio on prognosis of patients after resection of pancreatic adenocarcinoma
- Pancreatic intraepithelial neoplasia arising from an ectopic pancreas in the small bowel
