血清S-100β水平和小儿危重病例量表评分预测手足口病并发脑炎患儿预后的价值研究
熊 燚,王 健,魏 笛,冯 亚
·论著·
血清S-100β水平和小儿危重病例量表评分预测手足口病并发脑炎患儿预后的价值研究
熊 燚,王 健,魏 笛,冯 亚
目的探讨血清S-100β水平与小儿危重病例量表(PCIS)评分对手足口病(HFMD)并发脑炎患儿预后评估的价值。方法选取2012年12月—2014年12月遵义市第二人民医院收治的HFMD患儿190例为研究对象,根据是否并发脑炎,将患儿分为HFMD并发脑炎组(60例)和HFMD普通组(130例)。另选取同期本院体检中心体检健康的儿童40例为对照组。收集HFMD并发脑炎患儿入院24 h内各项资料,并依据PCIS对患儿进行病情危重程度评分,据此将患儿分为非危重、危重、极危重。患儿于入院后12 h、对照组体检时抽取空腹静脉血3 ml检测S-100β水平及白细胞计数(WBC),记录HFMD患儿住院期间死亡情况。结果各组S-100β水平、WBC比较,差异均有统计学意义(P<0.05);其中,HFMD并发脑炎组S-100β水平高于HFMD普通组及对照组,HFMD普通组与HFMD并发脑炎组WBC高于对照组(P<0.05)。HFMD并发脑炎组病死率为20%(12/60),高于HFMD普通组的4.6%(6/130)(χ2=18.32,P<0.05)。不同危重程度的HFMD并发脑炎患儿S-100β水平及病死率比较,差异均有统计学意义(P<0.05);其中危重者S-100β水平及病死率高于非危重者,极危重者S-100β水平及病死率高于非危重和危重者(P<0.01)。HFMD并发脑炎患儿S-100β水平与PCIS评分呈负相关(r=-0.478,P<0.01)。S-100β水平预测HFMD并发脑炎患儿死亡的受试者工作特征(ROC)曲线下面积为0.888〔95%CI(0.834,0.947),P<0.01〕,取临界值为2.91 μg/L时,灵敏度为84.46%,特异度为82.50%。PCIS评分预测HFMD并发脑炎患儿死亡的ROC曲线下面积为0.873〔95%CI(0.808,0.938),P<0.01〕,取临界值为69分时,灵敏度为83.10%,特异度为81.24%。结论血清S-100β水平和PCIS评分可特异反映HFMD并发脑炎患儿严重程度,对预测HFMD并发脑炎患儿预后具有较高的准确性。
手足口病;脑炎;S-100β;小儿危重病例量表;预后
熊燚,王健,魏笛,等.血清S-100β水平和小儿危重病例量表评分预测手足口病并发脑炎患儿预后的价值研究[J].中国全科医学,2016,19(23):2780-2784.[www.chinagp.net]
XIONG Y,WANG J,WEI D,et al.Values of serum S-100β level and pediatric critical illness scale in predicting hand-foot-mouth disease children complicated with encephalitis[J].Chinese General Practice,2016,19(23):2780-2784.
手足口病(hand-foot-mouth disease,HFMD)是儿科常见急性传染病,主要由多种肠道病毒感染引起[1],该病好发于5岁以下儿童,主要临床表现为发热及手、足、口腔等部位出现疱疹,一般预后良好,但少数患儿可出现心肌炎、脑炎等严重并发症,致使患儿病死率显著增加。其中,HFMD并发脑炎病情发展迅速,是导致患儿死亡的主要原因之一[2]。因此,早期特异评估患儿预后,对于改善其生存率具有重要临床意义。S-100β主要由神经胶质细胞合成分泌,脑损伤时脑脊液及血清中S-100β水平明显升高,其可特异性反映脑损伤的严重程度[3]。小儿危重病例量表(PCIS)是临床中常用的针对危重患儿病情严重程度评分系统之一,但其在HFMD并发脑炎患儿病情评估及预后判断的临床意义尚不完全明确。本研究拟通过探讨HFMD并发脑炎患儿血清S-100β水平、PCIS与预后的关系,为HFMD并发脑炎患儿的早期诊断及预后评估提供更有价值的指标。
1 对象与方法
1.1研究对象选取2012年12月—2014年12月遵义市第二人民医院收治的HFMD患儿190例为研究对象,其中男105例,女85例;平均月龄(20.8±12.2)月。患儿均符合原卫生部制定的《手足口病诊疗指南(2010年版)》[4]诊断标准。排除非HFMD肠道病毒感染者,近3个月内有呼吸道感染、神经系统疾病及脑肿瘤、脑创伤史者。根据是否有神经系统受累如嗜睡、呕吐、脑膜刺激征、腱反射减弱等表现,以及实验室检查和影像学特征[4],确诊HFMD并发脑炎患儿60例(HFMD并发脑炎组),余130例为HFMD普通组。另选取同期本院体检中心体检健康的儿童40例为对照组。受试者监护人均签署知情同意书,本研究方案由本院伦理委员会批准。
1.2方法
1.2.1PCIS评分收集HFMD并发脑炎患儿入院24 h内临床资料,包括心率、血压、呼吸频率、氧分压、pH值、Na+、K+、肌酐、血红蛋白、胃肠系统(如应激性溃疡、应激性溃疡出血等)情况,每项计为4、6或10分,计算总分。危重程度评价标准:PCIS评分>80分为非危重,71~80分为危重,<71分为极危重。
1.2.2观察指标患儿于入院后12 h及对照组体检时抽取空腹静脉血3 ml检测S-100β水平及血常规。血清S-100β水平采用酶联免疫试剂盒进行测定,试剂盒购自瑞士罗氏公司,操作过程严格按说明书进行,血常规采用全自动生化分析仪测定。记录HFMD患儿住院期间死亡情况。

2 结果
2.1各组一般资料及血清S-100β水平、WBC比较各组性别、月龄比较,差异均无统计学意义(P>0.05)。各组S-100β水平、WBC比较,差异均有统计学意义(P<0.05);其中,HFMD并发脑炎组S-100β水平高于HFMD普通组及对照组,HFMD普通组及HFMD并发脑炎组WBC高于对照组,差异均有统计学意义(P<0.05,见表1)。
表1各组一般资料及血清S-100β水平、WBC比较
Table 1Comparison of the general data and serum levels of S-100β,WBC among each group

组别例数性别(男/女)月龄(月)S-100β(μg/L)WBC(×109/L)对照组4024/1620.6±5.60.45±0.156.28±0.93HFMD普通组13071/5921.0±6.20.51±0.1811.32±0.92aHFMD并发脑炎组6034/2620.8±5.93.54±0.57ab11.72±0.73aF(χ2)值0.88c0.9721.4524.74P值>0.05>0.05<0.01<0.01
注:HFMD=手足口病,WBC=白细胞计数;与对照组比较,aP<0.01;与HFMD普通组比较,bP<0.01;c为χ2值
2.2各组病死率比较HFMD普通组治愈124例,治愈率为95.4%,6例患儿因病情加重死亡,病死率为4.6%。HFMD并发脑炎组治愈48例,治愈率为80.0%,死亡12例,病死率为20.0%。HFMD并发脑炎组患儿病死率高于HFMD普通组,差异有统计学意义(χ2=18.32,P<0.05)。
2.3不同危重程度的HFMD并发脑炎患儿S-100β水平及病死率比较不同危重程度的HFMD并发脑炎患儿S-100β水平及病死率比较,差异均有统计学意义(P<0.05);其中危重者S-100β水平及病死率高于非危重者,极危重者S-100β水平及病死率高于非危重和危重者,差异均有统计学意义(P<0.01,见表2)。
表2不同危重程度的HFMD并发脑炎患儿S-100β水平及病死率比较
Table 2Comparison of the S-100β level and fatality rate among different critical illness degrees in the HFMD children complicated with encephalitis
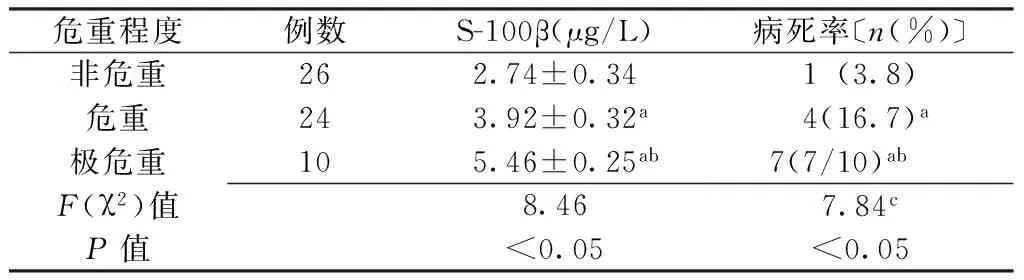
危重程度例数S-100β(μg/L)病死率〔n(%)〕非危重262.74±0.341(3.8)危重243.92±0.32a4(16.7)a极危重105.46±0.25ab7(7/10)abF(χ2)值8.467.84cP值<0.05<0.05
注:与非危重者比较,aP<0.01;与危重者比较,bP<0.01;c为χ2值
2.4HFMD并发脑炎不同预后患儿S-100β水平及PCIS评分比较HFMD并发脑炎死亡患儿S-100β水平高于存活者,PCIS评分低于存活者,差异有统计学意义(P<0.05,见表3)。
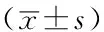
Table 3Comparison of the S-100β level and PCIS score between different clinical prognosis in the HFMD children complicated with encephalitis
预后例数S-100β(μg/L)PCIS评分(分)存活483.12±0.8377±6死亡125.82±1.1261±4t值4.538.73P值<0.01<0.01
注:PCIS=小儿危重病例量表
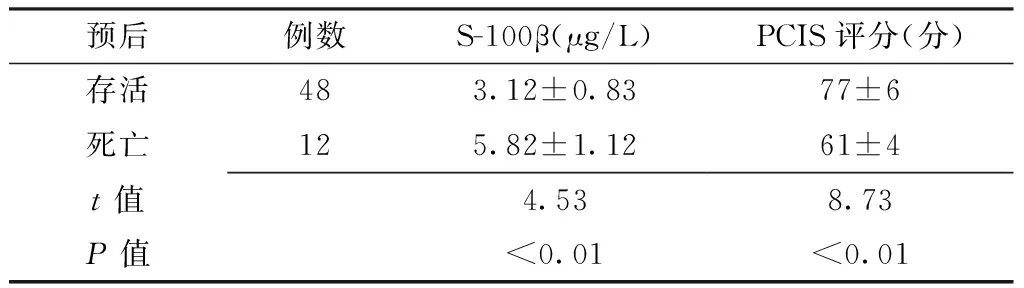
2.5血清S-100β水平与PCIS评分的相关性分析HFMD并发脑炎患儿S-100β水平与PCIS评分呈负相关(r=-0.478,P<0.01,见图1)。
注:PCIS=小儿危重病例量表
图1HFMD并发脑炎患儿S-100β水平与PCIS评分相关性的散点图
Figure 1Scatter diagram of the correlation between S-100β level and PCIS score of HFMD children complicated with encephatilis
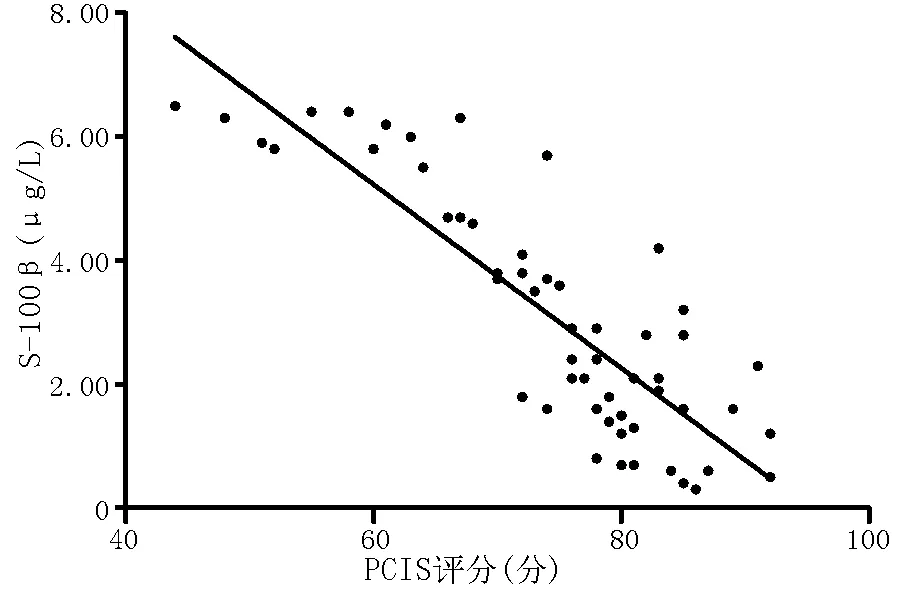
2.6ROC曲线分析S-100β水平预测HFMD并发脑炎患儿死亡的ROC曲线下面积为0.888〔95%CI(0.834,0.947),P<0.01〕,取临界值为2.91 μg/L时,灵敏度为84.46%,特异度为82.50%,阳性似然比为4.83,阴性似然比为0.19,Youden′s指数为66.96%(见图2)。PCIS评分预测HFMD并发脑炎患儿死亡的ROC曲线下面积为0.873〔95%CI(0.808,0.938),P<0.01〕,取临界值为69分时,灵敏度为83.10%,特异度为81.24%,阳性似然比为4.43,阴性似然比为0.21,Youden′s指数为64.34%(见图3)。
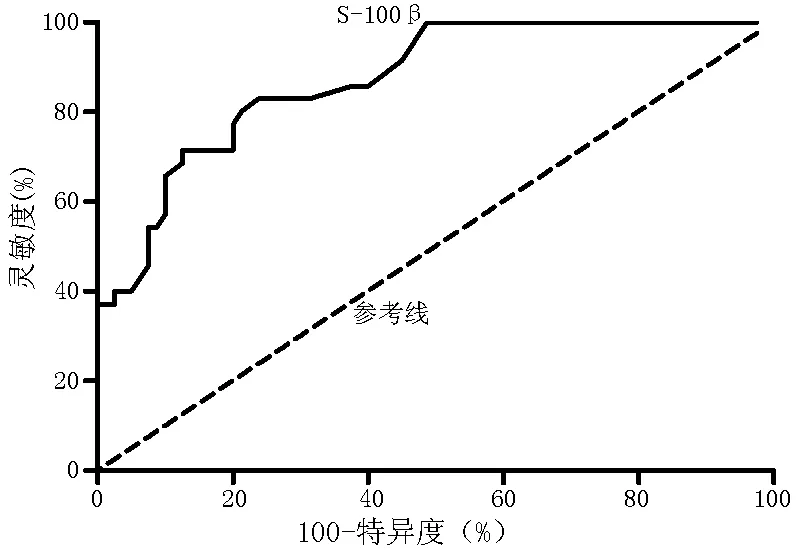
图2 S-100β水平预测HFMD并发脑炎患儿死亡的ROC曲线
Figure 2The ROC curve of the S-100β level for predicting death on the HFMD children complicated with encephalitis
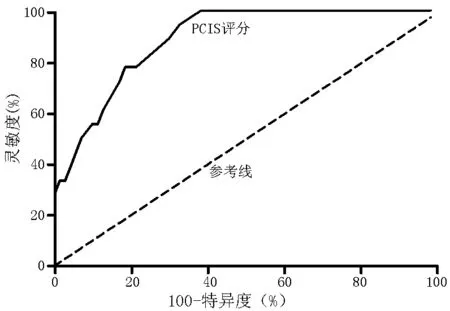
图3 PCIS评分预测HFMD并发脑炎患儿死亡的ROC曲线
Figure 3The ROC curve of the PCIS score for predicting death on the HFMD children complicated with encephalitis
3 讨论
HFMD是由肠道病毒引起的儿童急性传染病,大部分患儿病情较轻,预后良好,但少数HFMD重症患儿可并发中枢神经系统损害,即脑炎的发生,从而导致其病死率显著升高[5]。有研究报道,HFMD并发脑炎患儿较普通患儿病死率增加4.8%,且神经系统损害后遗症发生率升高14.3%[6]。因此,就HFMD并发中枢神经系统损害的患儿,及早做出诊断,准确判断其预后,对于降低其病死率及致残率具有重要的临床意义。
有研究证实,中枢神经系统损伤时血清及脑脊液中S-100β水平显著升高,其可特异性判断中枢神经系统损伤的严重程度及预后,从而受到广泛关注[7]。S-100β是主要由神经胶质细胞合成及分泌的钙结合蛋白,具有调节能量代谢、维持细胞膜完整性及参与细胞内信号传导的作用。生理情况下,脑脊液及血液中S-100β水平较低,但中枢神经系统受到损伤时,神经胶质细胞膜结构完整性被破坏,S-100β从细胞质释放入脑脊液,再通过已破坏的血-脑脊液屏障进入外周血[8]。因此,血清S-100β水平可作为评判中枢神经系统损伤的特异性标志物,同时其水平的变化可反映中枢神经系统损伤的程度及预后情况。本研究结果显示,入院24 h内,HFMD并发脑炎患儿血清S-100β水平明显高于普通HFMD患儿及健康儿童,而普通HFDM患儿与健康儿童间无差异,说明HFMD并发脑炎患儿中枢神经系统受到损害。同时,HFMD患儿WBC明显高于健康儿童,说明其体内存在明显的炎性反应,但WBC在HFMD并发脑炎组与HFMD普通组间无明显区别,提示WBC缺乏特异性,不能完全反映病情严重程度。已有相关研究显示,WBC对于评估炎症感染严重程度特异性较低,并且无法准确反映其预后情况,这可能与外周血中WBC个体差异大,不稳定即易受各种因素影响有关[9]。血清S-100β水平在非危重、危重和极危重患儿间呈升高趋势,其与PCIS评分呈明显的负相关,提示HFMD并发脑炎患儿病情越危重,其血清S-100β水平越高,死亡风险越高,预后也越差。已有研究证实,PCIS评分与患者病死率呈负相关[10]。本研究发现,HFMD并发脑炎死亡患儿血清S-100β水平高于存活患儿,并且PCIS评分低于存活患儿。S-100β水平及PCIS评分预测HFMD并发脑炎患儿死亡的ROC曲线下面积>0.850,可作为判断预后的有效指标,其中,S-100β取临界值为2.91 μg/L和PCIS评分取临界值为69分时对HFMD并发脑炎患儿预后不良的诊断准确性较高。
综上所述,血清S-100β水平及PCIS评分可特异反映HFMD并发脑炎患儿病情严重程度及预后,其对于指导患儿治疗,降低病死率具有重要临床意义。目前,HFMD并发脑炎患儿的早期诊断及预后判断尚缺乏有效的标准。通过检测HFMD并发脑炎患儿血清S-100β水平,同时结合PCIS评分可有效判断其病情的严重程度及预后。本研究没有进一步对HFMD并发脑炎患儿脑脊液、脑电图等方面做同步检测及观察,且样本量有限,研究结论可能存在一定的局限性,故需进一步加大样本量、多中心综合分析。
作者贡献:熊燚进行课题设计与实施、资料收集整理、成文并对文章负责;王健、魏笛进行课题设计与实施、评估、资料收集整理;冯亚进行质量控制及审校。
本文无利益冲突。
[1]李国英,李润青,张晓慧,等.肠道病毒71型和柯萨奇病毒A组致手足口病临床特点分析[J].中国全科医学,2012,15(4):1271-1272.
LI G Y,LI R Q,ZHANG X H,et al.Clinical features and nursing care of hand,foot and mouth disease caused by EV71 infection or CA16 infection[J].Chinese General Practice,2012,15(4):1271-1272.
[2]TSAI J D,KUO H T,CHEN S M,et al.Neurological images and the predictors for neurological sequelae of epidemic herpangina/hand-foot-mouth disease with encephalomyelitis[J].Neuropediatrics,2014,45(2):102-108.
[3]KOH S X,LEE J K.S100B as a marker for brain damage and blood-brain barrier disruption following exercise[J].Sports Med,2014,44(3):369-385.
[4]中华人民共和国卫生部.手足口病诊疗指南(2010年版)[J].国际呼吸杂志,2010,30(24):1473-1475.
Ministry of Health of the People′s Republic of China.Diagnosis and treatment guideline on hand-foot-mouth disease(2010)[J].International Journal of Respiration,2010,30(24):1473-1475.
[5]HUANG Y,ZHOU Y,LU H,et al.Characterization of severe hand,foot,and mouth disease in Shenzhen,China,2009-2013[J].J Med Virol,2015,87(9):1471-1479.
[6]ZENG H,WEN F,GAN Y,et al.MRI and associated clinical characteristics of EV71-induced brainstem encephalitis in children with hand-foot-mouth disease[J].Neuroradiology,2012,54(6):623-630.
[7]杜玉生,于佃敏.伴S100蛋白增高的缺血性脑卒中患者相关危险因素Logistic回归分析[J].现代预防医学,2012,39(16) :4079-4083.
DU Y S,YU D M.Logistic regression analysis of related risk factors of ischemic stroke patients with increased S100 protein[J].Modern Preventive Medicine,2012,39(16) :4079-4083.
[8]GEMPP E,LOUGE P,DE MAISTRE S,et al.Neuron-specific enolase and S100B protein levels in recreational scuba divers with neurological decompression sickness[J].Diving Hyperb Med,2014,44(1):26-29.
[9]LI Y,ZHU R,QIAN Y,et al.The characteristics of blood glucose and WBC counts in peripheral blood of cases of hand foot and mouth disease in China:a systematic review[J].PLoS One,2012,7(1):e29003.
[10]韩再萍,田先雨,麦光兴,等.乌司他丁对脓毒性休克患儿巨噬细胞移动抑制因子及危重程度的影响研究[J].中国妇幼保健,2014,29(1):57-59.
HAN Z P,TIAN X Y,MAI G X,et al.Effects of ulinastatin on macrophage migration inhibitory factor and risk degree of children with septic shock treatment[J].Maternal and Child Health Care of China,2014,29(1):57-59.
(本文编辑:吴立波)
Values of Serum S-100β Level and Pediatric Critical Illness Scale in Predicting Hand-foot-mouth Disease Children Complicated With Encephalitis
XIONGYi,WANGJian,WEIDi,FENGYa.
DepartmentofEmergency,theSecondPeople′sHospitalofZunyi,Zunyi563000,China
WANGJian,DepartmentofEmergency,theSecondPeople′sHospitalofZunyi,Zunyi563000,China;E-mail:wjzy02@163.com
ObjectiveTo investigate the value of serum S-100β level and pediatric critical illness scale(PCIS) in prognostic evaluating the hand-foot-mouth disease(HFMD) children complicated with encephalitis.Methods190 children with HFMD,whoP<0.05);the S-100β level of HFMD complicated with encephalitis group was higher than that of the HFMD general group and the control group,and the WBC of the HFMD general group and the HFMD complicated with encephalitis group was higher than that of the control group,which showed significant differences(P<0.05).The fatality rate of the HFMD complicated with encephalitis group was 20%(12/60),which was higher than 4.6%(6/130) in the HFMD general group,which showed significant differences(χ2=18.32,P<0.05).There was significant difference in the S-100β level and the fatality rate of the HFMD children complicated with encephalitis among different critical illness degrees(P<0.05);the S-100β level and the fatality rate of the critical illness cases were higher than those of the non-critical illness cases,and the S-100β level and the fatality rate of extremely critical illness cases were higher than those of the non-critical illness cases and critical illness cases,which showed significant differences(P<0.01).The S-100β level of the HFMD children complicated with encephalitis was negatively correlated with the score of PCIS(r=-0.478,P<0.01).The area under ROC curve of the HFMD children complicated with encephalitis,predicted as death through S-100β level,was 0.888〔95%CI(0.834,0.947),P<0.01〕,when the taken critical value was 2.91 μg/L,the sensitivity and the specificity were 84.46% and 82.50% respectively.The area under ROC curve of the HFMD children complicated with encephalitis,predicted as death through PCIS,was 0.873〔95%CI(0.808,0.938),P<0.01〕,and when the critical value was 69,the sensitivity and the specificity were 83.10% and 81.24% respectively.ConclusionThe serum S-100β level and PCIS score can reflect the severity degree of the HFMD children complicated with encephalitis,and have high accuracy in predicting the prognosis of the HFMD children complicated with encephalitis.
treatment in the Second People′s Hospital of Zunyi from December 2012 to December 2014,were enrolled as the research objects in this study.Based on whether children were complicated with encephalitis,we divided the children into HFMD complicated with encephalitis group(60 cases) and HFMD general group(130 cases).Other 40 children,who were regarded as healthy after physical examination in the physical examination center of this hospital at the same period,were included as the control group.We collected necessary information of the HFMD children complicated with encephalitis within the 24-hour after their being admitted into the hospital,and scored their critical illness condition based on PCIS,then divided the children as non-critical illness cases,critical illness cases and extremely critical illness cases.S-100β and WBC were detected by the extracted 3 ml fasting blood,which were got from HFMD children 12 h after their being admitted into the hospital and from the physical examination of control group.Also HFMD children′s death duration of hospital stay was recorded.ResultsThere were significant difference in S-100β level and WBC among the different groups(
Hand-foot-mouth disease;Encephalitis;S-100β;Pediatric critical illness scale;Prognosis
贵州省卫生厅科学技术基金项目(gzwkj2013-1-060);遵义市科学技术基金项目[遵义市科合社字(2013)37号]
563000贵州省遵义市第二人民医院急诊科(熊燚,王健,魏笛);贵州省遵义市红花岗区疾病预防控制中心(冯亚)
王健,563000贵州省遵义市第二人民医院急诊科;E-mail:wjzy02@163.com
R 512.5
A
10.3969/j.issn.1007-9572.2016.23.008
2015-06-02;
2016-04-27)

