乌司他丁对体外循环患儿炎症反应及氧自由基清除能力的影响观察
尹记辉
【摘要】 目的:觀察乌司他丁对体外循环(CPB)患儿炎症反应及氧自由基清除能力的影响。方法:选择2018年3月-2021年3月泰安市妇幼保健院收治的室间隔或房间隔缺损患儿120例作为研究对象,按照随机数字表法将患儿分为观察组及对照组,各60例。两组均根据患儿不同情况给予CPB房间隔修补术或室间隔修补术,观察组于开胸后主动脉插管前给予乌司他丁10 000 U/kg静脉推注半量,另外半量混入CPB预充液中随转机进入体内;对照组将乌司他丁换为等量生理盐水给予同观察组相同操作。记录比较两组麻醉时间、手术时间、CPB时间、主动脉阻断时间及住院时间;分别于术前(T0)、CPB停止4 h(T1)及术后24 h(T2)采血测定炎症因子水平,包括血浆白细胞介素-6(IL-6)、白细胞介素-8(IL-8)、白细胞介素-10(IL-10)、肿瘤坏死因子-α(TNF-α)及C反应蛋白(CRP)水平,氧自由基清除指标包括血浆超氧化物歧化酶(SOD)、丙二醛(MDA)水平,比较不同时间两组各因子水平差异。结果:两组麻醉时间、手术时间、CPB时间、主动脉阻断时间、住院时间比较,差异均无统计学意义(P>0.05)。两组T0的IL-6、TNF-α、IL-8、IL-10、SOD、MDA比较,差异均无统计学意义(P>0.05);T1、T2,对照组IL-6、TNF-α、IL-8、MDA及观察组IL-6、TNF-α、MDA均高于T0,观察组上述指标均低于对照组,两组IL-10均高于T0,且观察组均高于对照组(P<0.05);观察组T1的IL-8高于T0,但低于对照组(P<0.05);对照组T1、T2及观察组T1的SOD均低于T0,观察组T1、T2的SOD均高于对照组,差异均有统计学意义(P<0.05);T2,两组IL-6、TNF-α、IL-10、MDA及对照组IL-8均低于T1,对照组SOD高于T1,差异均有统计学意义(P<0.05)。结论:在患儿CPB心脏手术中,乌司他丁可有效抑制促炎因子升高,上调抗炎介质的释放,促进氧自由基清除,从而减少机体损伤。
【关键词】 乌司他丁 体外循环 炎症反应 氧自由基
Effect of Ulinastatin on Inflammatory Response and Oxygen Free Radical Scavenging Ability in Children Undergoing Cardiopulmonary Bypass/YIN Jihui. //Medical Innovation of China, 2022, 19(11): 00-005
[Abstract] Objective: To observe the effect of Ulinastatin on inflammatory response and oxygen free radical scavenging ability in children undergoing cardiopulmonary bypass (CPB). Method: A total of 120 children with ventricular septal or atrial septal defect treated in Tai’an Maternal and Child Health Care Hospital from March 2018 to March 2021 were selected as the research objects, according to the random number table method, the children were divided into observation group and control group, 60 cases in each group. Both groups were given CPB atrial septal repair or ventricular septal repair according to different conditions of children, the observation group was given half of Ulinastatin 10 000 U/kg intravenously before aortic intubation after thoracotomy, and the other half was mixed into CPB precharge and entered the body with the turn; in the control group, Ulinastatin was replaced with the same amount of Normal Saline and given the same operation as the observation group. Anesthesia time, operation time, CPB time, aortic occlusion time and hospital stay were recorded and compared between the two groups; the levels of inflammatory factors, including plasma interleukin-6 (IL-6), interleukin-8 (IL-8), interleukin-10 (IL-10) and tumor necrosis factor-α (TNF-α), and oxygen radical scavenging index, including plasma superoxide dismutase (SOD) and malondialdehyde (MDA) were measured before operation (T0), 4 h after CPB (T1) and 24 h after operation (T2), the above indexes were compared between the two groups at different times. Result: There were no significant differences in anesthesia time, operation time, CPB time, aortic occlusion time and hospital stay between the two groups (P>0.05). There were no significant differences in IL-6, TNF-α, IL-8, IL-10, SOD and MDA between the two groups at T0 (P>0.05); at T1 and T2, IL-6, TNF-α, IL-8, MDA in the control group, and IL-6, TNF-α, MDA in the observation group were higher than those at T0, the above indexes in the observation group were lower than those in the control group, IL-10 of the two groups were higher than those at T0, and the observation group were higher than those in the control group (P<0.05); IL-8 in the observation group at T1 was higher than that at T0, and that in the observation group was lower than that in the control group (P<0.05); the SOD of the control group at T1 and T2 and the observation group at T1 were lower than those at T0, and the SOD of the observation group at T1 and T2 were higher than those of the control group, the differences were statistically significant (P<0.05); at T2, IL-6, TNF-α, IL-10, MDA in the two groups and IL-8 in the control group were lower than those at T1, and SOD in the control group was higher than that at T1, the differences were statistically significant (P<0.05). Conclusion: Ulinastatin can effectively inhibit the increase of pro-inflammatory factors, up regulate the release of anti-inflammatory mediators, promote oxygen free radical scavenging and reduce body damage during CPB heart surgery in children.
[Key words] Ulinastatin Cardiopulmonary bypass Inflammatory reaction Oxygen free radical
First-author’s address: Tai’an Maternal and Child Health Care Hospital, Shandong Province, Tai’an 271000, China
doi:10.3969/j.issn.1674-4985.2022.11.001
体外循环(CPB)是婴幼儿先天性心脏病心脏直视手术治疗中的必备条件,在心脏停搏的情况下为其他组织器官提供血液供应[1-2]。在成年人中,体外循环心脏手术与全身炎症反应(SIR)显著升高相关,全身炎症反应可导致严重术后并发症,CPB引发的氧自由基的释放、炎症级联的激活可引起多脏器损伤[3]。儿科患儿,尤其是婴儿和新生儿,循环血浆量少,器官不成熟,因此,CPB引起的低体温、循环变化、血液稀释、酸碱平衡和全身炎症反应综合征(SIRS)的影响比成人大得多,且婴幼儿可能有不成熟的抗氧化防御系统,因此更容易受到氧化剂应激的影响[4-5]。乌司他丁是一种尿胰蛋白酶抑制剂,被用于治疗胰腺炎、脓毒症等炎症疾病,已有研究表明其可减少CPB后缺血再灌注损伤,从而保护心肝肾等重要脏器[6-8]。本研究选取需手术治疗的先天性心脏病患儿,研究乌司他丁对体外循环患儿炎症反应及氧自由基清除能力的影响,报道如下。
1 资料与方法
1.1 一般资料 选择2018年3月-2021年3月泰安市妇幼保健院收治的先天性心脏病患儿120例作为研究对象,纳入标准:所有患儿均行常规术前胸片检查、心电图、超声心动图、全血细胞计数和生化检查等,确诊有室间隔或房间隔缺损并需手术治疗。排除标准:(1)术前存在感染;(2)凝血功能障碍;(3)肺、肝、肾功能障碍;(4)围手术期使用类固醇治疗;(5)过敏体质。按照随机数字表法将患者分为观察组及对照组,各60例。患儿监护人知情同意本研究,且本研究经医院伦理委员会批准。
1.2 方法 所有患儿均在静吸复合麻醉下进行手术,手术方式根据患儿不同情况给予房间隔修补术或室间隔修补术。于胸骨正中切口建立CPB,根据患儿缺损部位选择心脏切口并进行缺损缝补,待患儿各指标稳定后缝合关胸。CPB建立:预充液采用乳酸格林液为基础液,阻断主动脉后灌注停跳液,辅以心脏局部深低温,肝素化后插管并建立CPB。观察组于开胸后主动脉插管前给予乌司他丁(生产厂家:广东天普生化医药股份有限公司,批准文号:国药准字H19990134,规格:10万单位)10 000 U/kg静脉推注半量,另外半量混入CPB预充液中随转机进入体内;对照组将乌司他丁换为等量生理盐水给予同观察组相同操作。
1.3 观察指标 (1)比较两组手术及住院指标:麻醉时间、手术时间、CPB时间、主动脉阻断时间及住院时间;(2)比较两组炎症因子水平及氧自由基清除指标:分别于术前(T0)、CPB停止4 h(T1)及术后24 h(T2)采血测定炎症因子水平,包括血浆白细胞介素-6(IL-6)、白细胞介素-8(IL-8)、白细胞介素-10(IL-10)、肿瘤坏死因子-α(TNF-α)及C反应蛋白(CRP)水平,氧自由基清除指标包括血浆超氧化物歧化酶(SOD)、丙二醛(MDA)水平。
1.4 统计学处理 用统计学处理软件SPSS 26.0对所得数据进行处理。计量资料中符合正态分布者用(x±s)表示,组间比较用独立样本t检验,组内比较用配对t检验;计数资料用例(%)表示,比较则用字2检验。P<0.05为差异有统计学意义。
2 结果
2.1 两组一般资料比较 观察组男33例,女27例;年龄6个月~5岁,平均(2.42±0.87)岁;体重6.32~18.78 kg,平均(12.20±3.51)kg;房间隔缺损17例,室间隔缺损43例。對照组男35例,女25例;年龄7个月~5岁,平均(2.72±0.95)岁;体重6.18~19.36 kg,平均(12.48±3.34)kg;房间隔缺损15例,室间隔缺损45例。两组一般资料比较,差异均无统计学意义(P>0.05),具有可比性。
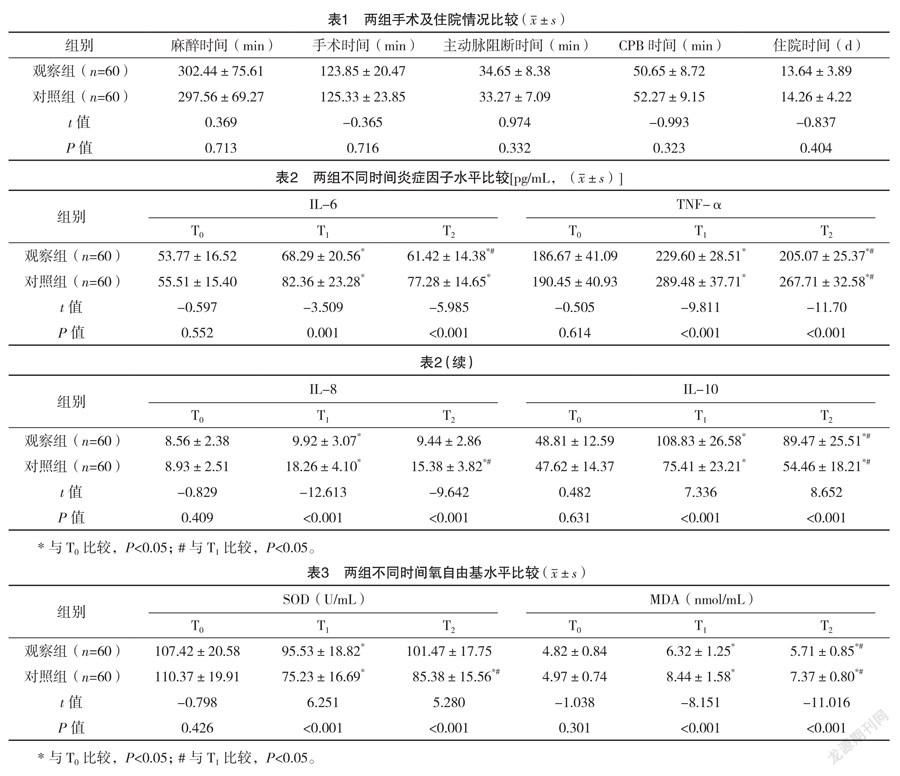
2.2 两组手术及住院情况比较 两组麻醉时间、手术时间、CPB时间、主动脉阻断时间、住院时间比较,差异均无统计学意义(P>0.05),见表1。
2.3 两组不同时间炎症因子水平比较 两组T0的IL-6、TNF-α、IL-8、IL-10比较,差异均无统计学意义(P>0.05);T1、T2,对照组IL-6、TNF-α、IL-8及观察组IL-6、TNF-α均高于T0,且观察组T1、T2的IL-6、TNF-α、IL-8均低于对照组,差异均有统计学意义(P<0.05);两组T1、T2的IL-10均高于T0,且观察组均高于对照组,差异均有统计学意义(P<0.05);观察组T1的IL-8高于T0,差异有统计学意义(P<0.05);T2,两组的IL-6、TNF-α、IL-10及对照组IL-8均低于T1,差异均有统计学意义(P<0.05)。见表2。
2.4 两组不同时间氧自由基水平比较 T0,两组SOD、MDA比较,差异均无统计学意义(P>0.05)。对照组T1、T2及观察组T1的SOD均低于T0,观察组T1、T2的SOD均高于对照组,差异均有统计学意义(P<0.05);两组T1、T2的MDA均高于T0,且观察组均低于对照组,差异均有统计学意义(P<0.05);T2,两组MDA低于T1,对照组SOD高于T1,差异均有统计学意义(P<0.05)。见表3。
3 讨论
在先天性心臟病患儿中,CPB在心脏手术期间维持组织的血液供应,并保护心肌组织免受缺血性损伤[9],然而,CPB与缺血/再灌注损伤有关,再灌注损伤是在缺血或缺氧一段时间后,当血液供应回到组织中时引起的组织损伤[10]。最近,体外和离体研究表明,氧化自由基的产生在心肌缺血-再灌注损伤中起着重要的病因学作用,婴儿和新生儿可能有不成熟的抗氧化防御系统,因此更容易受到氧化剂应激的影响[11];在使用CPB进行心脏手术期间,心脏和肺部的血液供应暂时几乎完全停止,这些器官内缺氧促使细胞积累代谢中间产物,细胞损伤诱导细胞表面黏附分子的上调和促炎细胞因子的表达[12];此外,在心脏外科手术中,不同的刺激,如血液暴露于CPB的非内皮表面及泵、人工肺、插管、抽吸和通气回路对血细胞成分施加剪切应力,损伤红细胞、白细胞和血小板,亦可能会引发炎症反应[13-14]。体液和细胞级联的激活导致循环血液中促炎细胞因子的增加和白细胞募集的增强[12],由此产生的SIRS与术后并发症有关,包括心肌功能障碍、呼吸衰竭、急性肾损伤等。减少CPB患儿炎症反应及氧化应激反应对机体恢复至关重要。
乌司他丁属蛋白酶抑制剂,可清除氧自由基,稳定溶酶体膜,抑制炎症物质,其常用于胰腺炎治疗中[6,15]。其应用于心脏手术中,可减轻炎症反应,并可明显保护患者心肺功能[3,16-18]。本研究将其应用于室间隔或房间隔缺损患儿的CPB心脏手术中,其对麻醉时间、手术时间、CPB时间、主动脉阻断时间、住院时间无明显影响,但与对照组炎症因子IL-6、TNF-α、IL-8、IL-10比较均明显改善。CPB诱发促炎和抗炎细胞因子释放的改变,在接受心脏手术的患者中,促炎细胞因子IL-6、TNF-α、IL-8水平的升高与不良临床结果相关[12],TNF-α可促进多种炎症因子释放,在炎症反应启动触发中发挥重要作用,IL-6在炎症反应急性期升高,是炎症反应敏感指标,IL-8是促进炎症反应的典型介质,而IL-10则属于抑炎因子,可保护机体免受炎症反应损害[19],本研究结果证明乌司他丁可有效抑制促炎因子升高,上调抗炎介质的释放。人体内SOD可有效地清除氧自由基,维持机体氧化与抗氧化平衡,在氧化应激反应中对细胞起到保护作用,自由基作用于脂质发生过氧化反应产生MDA,间接反应组织过氧化损伤程度,SOD与MDA结合分析有助于判断机体脂质过氧化及缺血再灌注损伤的程度[20]。Sznycer-Taub等[11]研究表明CPB心脏手术可影响心肌氧化应激,本研究中使用乌司他丁的观察组术后SOD、MDA更优,说明其有利于氧自由基清除,从而减少缺血再灌注损伤。
综上所述,在患儿CPB心脏手术中,乌司他丁可有效抑制促炎因子升高,上调抗炎介质的释放,促进氧自由基清除,从而减少机体损伤。
参考文献
[1] STURMER D,BEATY C,CLINGAN S,et al.Recent innovations in perfusion and cardiopulmonary bypass for neonatal and infant cardiac surgery[J].Transl Pediatr,2018,7(2):139-150.
[2]谢柯祺,夏氢,罗继文,等.乌司他丁对体外循环心脏手术后心肌损伤及缺血再灌注相关病理环节的影响[J].海南医学院学报,2018,24(17),1578-1581,1586.
[3] PANG X Y,FANG C C,CHEN Y Y,et al.Effects of Ulinastatin on Perioperative Inflammatory Response and Pulmonary Function in Cardiopulmonary Bypass Patients[J/OL].Am J Ther,2016,23(6):e1680-e1689.
[4] HIRATA Y.Cardiopulmonary bypass for pediatric cardiac surgery[J].Gen Thorac Cardiovasc Surg,2018,66(2):65-70.
[5] SZNYCER-TAUB N,MACKIE S,PENG Y W,et al.Myocardial Oxidative Stress in Infants Undergoing Cardiac Surgery[J].Pediatr Cardiol,2016,37(4):746-750.
[6]张雪芹,徐晓林.乌司他丁对急性胰腺炎患者氧自由基清除能力及炎性应激的改善作用[J].昆明医科大学学报,2017,38(8):90-93.
[7]梁丽俊,张丽芬.乌司他丁对法洛四联症根治术婴幼儿炎性反应的影响和心肌保护作用[J].中国药物与临床,2016,16(8):1181-1183.
[8] PERMANYER E,MUNOZ-GUIJOSA C,PADRÓ J M,et al.Mini-extracorporeal circulation surgery produces less inflammation than off-pump coronary surgery[J].Eur J Cardiothorac Surg,2020,57(3):496-503.
[9] AZARFARIN R,DASHTI M,TOTONCHI Z,et al.Efficacy of the “head-up position” in returning cardiopulmonary bypass blood to the patient and reducing the required blood transfusion: a randomized tria[J].Iran Heart J,2017,18:6-15.
[10] SCHOFIELD Z V,WOODRUFF T M,HALAI R,et al.
Neutrophilsea key component of ischemia-reperfusion injury[J].Shock,2013,40(6):463-470.
[11] SZNYCER-TAUB N,MACKIE S,PENG Y W,et al.
Myocardial Oxidative Stress in Infants Undergoing Cardiac Surgery[J].Pediatr Cardiol,2016,37(4):746-750.
[12] KRAFT F,SCHMIDT C,VAN AKEN H,et al.Inflammatory response and extracorporeal circulation[J].Best Pract Res Clin Anaesthesiol,2015,29(2):113-123.
[13] HIRATA Y.Cardiopulmonary bypass for pediatric cardiac surgery[J].Gen Thorac Cardiovasc Surg,2018,66(2):65-70.
[14] HAPONIUK I,JAWORSKI R,PACZKOWSKI K,et al.
Postoperative kinetics of common inflammatory biomarkers after congenital heart defect procedures with extracorporeal circulation in children[J].Kardiol Pol,2018,76(6):968-973.
[15] ZHANG R,MA J,ZHENG P,et al.Ulinastatin plus biapenem for severe pneumonia in the elderly and its influence on pulmonary function and inflammatory cytokines[J].Am J Transl Res,2021,13(5):5027-5034.
[16]宗晓倩,金晓玲,马钰,等.乌司他丁预处理对心脏瓣膜置换患者心肌氧化应激损伤的保护作用[J/OL].中华临床医师杂志(电子版),2016,10(10):1437-1440.
[17]于浩,颜涛,马涛,等.乌司他丁对复杂先天性心脏病患儿体外循环围术期肺保护作用的研究[J].广东医学,2017,38(20):3184-3187.
[18]李慧蕴,杨志远,谢周良,等.乌司他丁对体外循环下法洛四联症根治术患儿心肌损伤的影响[J].中华实验外科杂志,2017,34(2):321-324.
[19] GORJIPOUR F,TOTONCHI Z,GHOLAMPOUR DEHAKI M,
et al.Serum levels of interleukin-6, interleukin-8, interleukin-10, and tumor necrosis factor-α, renal function biochemical parameters and clinical outcomes in pediatric cardiopulmonary bypass surgery[J].Perfusion,2019,34(8):651-659.
[20]董向陽,李文静,翟波,等.乌司他丁在婴幼儿体外循环手术中对氧自由基的影响[J].中国实用医药,2015,10(35):31-32.
(收稿日期:2021-09-30) (本文编辑:张爽)